Introduction
Breast cancer is the second leading cause of cancer mortality among women, after lung cancer. According to the American Cancer Society, approximately 1.3 million women worldwide are diagnosed with breast cancer annually, and >465,000 women die of this disease [
1]. In Korea, the age-standardized incidence rate of invasive breast cancer has continued to increase over time and was 84.3 cases per 100,000 women in 2014 [
2]. Postoperative adjuvant systemic therapy prolongs survival in selected women with breast cancer and reduces the odds of death by 25% per year [
3]. Tamoxifen is widely used as hormonal therapy in both, pre- and postmenopausal women with breast cancer and effectively reduces the risk of recurrence and mortality [
45].
Tamoxifen shows complex hormonal actions. It acts primarily as an anti-estrogenic drug; however, it also exerts a mild estrogenic effect depending upon the end organ, endogenous estrogen levels, and the tamoxifen dose [
6]. A few studies have shown a statistically significant association between endometrial cancer and tamoxifen in postmenopausal women with breast cancer [
789]. Additionally, endometrial polyps resected from women with breast cancer receiving tamoxifen showed a high rate of malignant transformation [
10]. Moreover, considering the estrogenic property of tamoxifen, physicians are usually concerned regarding the relationship between tamoxifen and common estrogen-dependent gynecological tumors including leiomyoma or adenomyosis.
Tamoxifen could affect the ovaries. Several studies have reported that tamoxifen exposure could be related to the development of ovarian cysts or an increased risk of ovarian cancer [
1112].
We evaluated the effects of tamoxifen on gynecological conditions including endometrial lesions, ovarian cysts, and leiomyomas or adenomyosis, in women with breast cancer.
Materials and methods
1. Patients
We evaluated 309 women with breast cancer. All women had undergone surgery for breast cancer and had received tamoxifen postoperatively. We retrospectively analyzed the clinicopathological data, the results of transvaginal ultrasonography (TV-US), and the histopathological results of endometrial biopsies from patients' medical records. Menopausal status was assessed based on the menstrual history and serum hormone levels measured in all women. Premenopausal women were defined as women with regular menstrual cycles or those with serum follicle-stimulating hormone (FSH) levels <40 mIU/mL when checked within 3 months before and after the gynecological evaluation. Postmenopausal women were defined as women with amenorrhea for >12 months and serum FSH levels >40 mIU/mL on 2 consecutive occasions.
2. Gynecological examination
TV-US was performed every 6 months in all women between January 2010 and December 2016. In premenopausal women, TV-US was performed regardless of the day of the menstrual cycle. The endometrial thickness was measured at the site of maximum thickness of the endometrium in a longitudinal plane.
In postmenopausal and amenorrheic premenopausal women with low FSH levels, endometrial thickness ≥5 mm was defined as endometrial thickening. In women with regular menstruation, endometrial thickness ≥12 mm was defined as endometrial thickening.
Indications for an endometrial biopsy were: 1) women showing thickened endometrium on TV-US (endometrial thickness ≥5 mm in premenopausal amenorrheic women or postmenopausal women, and endometrial thickness ≥12 mm in premenopausal women with regular menstruation), 2) women with abnormalities in the endometrial cavity on TV-US and, 3) women with abnormal uterine bleeding.
An endometrial biopsy was performed at the outpatient clinic or the day-surgery unit using a blind technique in women with a thickened endometrium or abnormal uterine bleeding. Women showing abnormalities on TV-US underwent diagnostic hysteroscopy at the outpatient clinic to assess endometrial lesions. Women with a hysteroscopic diagnosis of an endometrial mass underwent surgical hysteroscopy under monitored anesthesia care.
Women diagnosed with a leiomyoma or adenomyosis underwent regular 6-month follow-up to monitor the tumor size. Women newly diagnosed with ovarian cysts underwent TV-US and assessment of serum cancer antigen 125 (CA-125) levels to study the characteristics of the ovarian cyst. Women showing intracystic solid components on TV-US or elevated serum CA-125 levels underwent diagnostic radiological evaluation including computed tomography or magnetic resonance imaging. Women showing multiseptated ovarian cysts with serum CA-125 levels within the normal range underwent more frequent TV-US assessment (at 2–3-month intervals).
3. Statistical analysis
Statistical analysis was performed using the IBM SPSS software version 18.0 (IBM Corp., Armonk, NY, USA). Age, body mass index (BMI), and duration of tamoxifen treatment were compared using the Student's t-test. Hormonal status of breast cancer tissue, endometrial thickness, and menopausal status were compared using the χ2 test. A P-value <0.05 was considered statistically significant.
Results
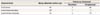
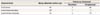
Patient characteristics are shown in
Table 1. Postmenopausal women were older. Additionally, the BMI was higher and the duration of tamoxifen treatment was longer in post- than in premenopausal women.
Table 1
Clinicopathological and demographic characteristics of women receiving tamoxifen

|
Characteristics |
All patients (n=309) |
Premenopausal women (n=92) |
Postmenopausal women (n=217) |
P-value |
|
Age (yr) |
50.5±8.9 |
42.9±4.6 |
53.4±8.8 |
0.000 |
|
BMI (kg/m2) |
23.0±2.9 |
22.3±2.9 |
23.2±2.8 |
0.008 |
|
Duration of tamoxifen treatment (yr) |
4.1±1.7 |
3.7±1.5 |
4.2±1.7 |
0.013 |
|
Breast cancer stage |
|
|
|
0.314 |
|
CIS |
35 (11.3) |
13 (14.1) |
22 (10.1) |
|
|
I |
108 (35.0) |
25 (27.2) |
83 (38.2) |
|
|
II |
126 (40.8) |
37 (40.2) |
89 (41.0) |
|
|
III |
34 (11.0) |
15 (16.3) |
19 (8.8) |
|
|
IV |
6 (1.9) |
2 (2.2) |
4 (1.8) |
|
|
Hormonal status of breast cancer tissue |
|
|
|
|
|
ER + |
261 (84.5) |
77 (84) |
184 (84.8) |
0.808 |
|
PR + |
247 (79.9) |
75 (82) |
172 (79.3) |
0.652 |

Based on TV-US, 34 women were diagnosed with endometrial thickening. The prevalence of endometrial thickening was 12% in the pre- and 10.6% in the postmenopausal group. No intergroup difference was observed in the ratio of the thickened endometrium identified using TV-US. An ovarian cyst was detected in 25 women based on TV-US. Women diagnosed with an ovarian cyst were younger than those without an ovarian cyst (46.9±7.4 vs. 50.9±9.0 years, P=0.015). However, no significant intergroup differences were observed in age, BMI, duration of tamoxifen treatment, menopausal status, and hormonal status of breast cancer tissue (data are not shown).
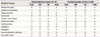
Among the 25 women diagnosed with ovarian cysts, 23 showed benign lesions on TV-US and normal serum CA-125 levels. These women underwent follow-up TV-US 6 months later. The results of follow-up TV-US are presented in
Table 2. Total abdominal hysterectomy and bilateral salpingo-oophorectomy were performed in 1 woman with adenomyosis and a septated right ovarian cyst that was diagnosed as a serous cystadenoma based on histopathological examination. One woman was not followed-up after being diagnosed with an ovarian cyst.
Table 2
The number of ovarian cysts detected by ultrasonographic examination
|
Characteristics |
Newly detected ovarian cyst |
Follow-up ultrasound |
|
Persistent |
Disappeared |
|
In all women |
25 |
3 |
20 |
|
In premenopausal group |
10a)
|
1 |
7 |
|
In postmenopausal group |
15 |
2 |
13 |

Leiomyoma was detected in 29 women (10 in pre- and 19 in postmenopausal women). Adenomyosis was diagnosed in only 9 postmenopausal women.
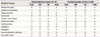
The indications and results of an endometrial biopsy are presented in
Table 3. The indications for an endometrial biopsy were thickened endometrium, abnormalities detected on TV-US, and abnormal uterine bleeding. One woman in the postmenopausal group who reported abnormal uterine bleeding was diagnosed with endometrial adenocarcinoma. Five women in the postmenopausal group with endometrial thickening were diagnosed with atrophic endometrium. All 5 reported a history of postoperative chemotherapy.
Table 3
Indications and results of endometrial biopsy performed in 43 women
|
Result of biopsy |
Premenopausal women (n=14) |
Postmenopausal women (n=29) |
|
Total |
EM |
US |
AUB |
Total |
EM |
US |
AUB |
|
Endometrial polyp |
5 |
2 |
1 |
2 |
9 |
4 |
2 |
3 |
|
Endometrial hyperplasia |
1 |
0 |
0 |
1 |
3 |
2 |
0 |
1 |
|
Adenocarcinoma |
0 |
0 |
0 |
0 |
1 |
0 |
0 |
1 |
|
Leiomyoma |
0 |
0 |
0 |
0 |
1 |
0 |
1 |
0 |
|
Atrophic endometrium |
2 |
0 |
0 |
2 |
9 |
5 |
0 |
4 |
|
Proliferative phase |
3 |
2 |
0 |
1 |
0 |
0 |
0 |
0 |
|
Secretory phase |
2 |
2 |
0 |
0 |
0 |
0 |
0 |
0 |
|
hematoma |
0 |
0 |
0 |
0 |
3 |
2 |
0 |
1 |
|
Metaplasia |
0 |
0 |
0 |
0 |
2 |
1 |
1 |
0 |
|
Stromal-glandular breakdown |
1 |
1 |
0 |
0 |
0 |
0 |
0 |
0 |
|
Granulation tissue |
0 |
0 |
0 |
0 |
1 |
1 |
0 |
0 |

Discussion
Tamoxifen, which shows anti-estrogenic effects in breast tissue is an effective adjuvant treatment for breast cancer in pre- and postmenopausal women. However, it shows complex hormonal actions, and it could produce a mild estrogenic effect [
6]. Therefore, clinicians are concerned regarding the tamoxifen-induced estrogenic stimulation observed in several gynecological diseases.
Based on TV-US measurements, tamoxifen is known to trigger endometrial thickening. Gerber et al. [
13] reported a significant increase in the mean endometrial thickness after 3 years of tamoxifen administration. Notably, a significant increase (>50%) in secondary endometrial thickening measured by TV-US in postmenopausal women treated with tamoxifen, has been associated with a high rate of endometrial pathologies including endometrial cancer [
14].
The utility of TV-US for screening of tamoxifen-induced endometrial proliferation is debatable. Gerber et al. [
13] reported that among 52 asymptomatic women with thickened (≥10 mm) or morphologically suspect endometrium who underwent hysteroscopy and dilation and curettage, uterine perforation occurred in 4 and asymptomatic endometrial carcinoma in only 1 woman. Owing to increased iatrogenic morbidity and high false-positive rates of TV-US, this study expressed uncertainty regarding the utility of endometrial screening using TV-US in women treated with tamoxifen [
13]. In our study, endometrial biopsy was performed in 43 women, and no case of uterine perforation was reported. In women with a small and atrophied uterus, we used misoprostol for cervical dilation. Therefore, we concluded that the risk of iatrogenic morbidity during an endometrial biopsy was not as high as reported by Gerber et al. [
13]. In the study reported by Gerber et al. [
13], endometrial thickening was defined as endometrial thickness ≥10 mm. In our study, we used endometrial thickness ≥5 mm as the cut-off value. This cut-off value was adopted based on widely accepted endometrial thickness values observed in healthy postmenopausal women [
14].
In our study, endometrial hyperplasia and endometrial carcinoma were diagnosed in women with abnormal uterine bleeding not with thickened endometrium (≥5 mm) and abnormalities identified on TV-US. This finding implies that a single assessment of endometrial thickness using TV-US or the cut-off level ≥5 mm is not a reliable predictor of endometrial pathology in women receiving tamoxifen. Further studies are warranted to define more specific ultrasonographic criteria to determine endometrial pathology.
The risk of development of polyps and endometrial hyperplasia and cancer in women receiving tamoxifen is 2- to 4-fold higher than that in women not receiving tamoxifen [
15]. Consistent with this study, endometrial polyps are the most common endometrial pathology (occurrence rate 8–36%) associated with tamoxifen use in postmenopausal women. These polyps are distinguished from typical polyps in that these are more translucent with a higher fibrotic content [
1617]. However, the incidence of endometrial polyps was relatively low in our study—5.4% in pre- and 4.1% in postmenopausal women. Additionally, we could not exclude the possibility that a few endometrial polyps existing before the administration of tamoxifen were diagnosed only after these women were included in this study. These results suggest that the incidence of endometrial polyps in Korean women might be lower than that in women of other ethnicities.
Endometrial polyps may show components with simple or complex endometrial hyperplasia (with or without atypia) and a small focus of endometrial carcinoma [
16]. In our study, endometrial polyps did not show any endometrial hyperplasia or cancer.
Metindir et al. [
6] reported that tamoxifen can cause ovarian cyst formation. In their study, ovarian cysts were detected in 49.1% of pre- and 1.1% of postmenopausal women, and adjuvant chemotherapy did not show a significant association with the development of ovarian cysts. In our study, ovarian cysts were detected in 15 of 92 (16.3%) pre- and 10 of 217 (4.6%) postmenopausal women, which concurs with previous reports on Korean women [
15]. Kim et al. [
15] reported that the prevalence of ovarian cysts in women receiving tamoxifen was 19.4% in pre- and 6.3% in postmenopausal women. The exact mechanism by which tamoxifen triggers the development of ovarian cysts remains unclear. One of the suggested mechanisms is a tamoxifen-induced increase in the secretion of gonadotropin-releasing hormone (GnRH) (via its anti-estrogenic effect). Tamoxifen structurally resembles clomiphene, and clomiphene decreases circulating estrogen levels available to the hypothalamus. This process induces the secretion of GnRH [
18]. Another possibility is that tamoxifen directly acts on the ovaries. Sherman et al. [
19] have shown that serum estradiol and progesterone concentrations in premenopausal women receiving 10 mg of tamoxifen twice daily were 2–3 times higher than those in women not receiving tamoxifen. Tamoxifen can cause excessive growth of ovarian follicles, resulting in elevated estradiol levels.
Although ovarian cysts may cause complications and be revealed as malignancy, most women in our study showed resolution of cysts without any complications reported during follow-up. Therefore, ovarian cysts in women receiving tamoxifen could be managed with close and careful follow-up without requiring immediate surgery.
Limitations of this study: 1) The number of women included in this study was relatively small, and the follow-up period was not long enough to accurately observe the hormonal influence of tamoxifen on various gynecological conditions. 2) TV-US was performed by several gynecologists, which may not guarantee unified diagnostic criteria of TV-US. 3) This study did not include a control group comprising women who did not receive tamoxifen; thus, comparative analysis was not possible. In this study, we focused on the differences between the pre- and postmenopausal groups but did not compare these with controls. This fact could serve as an important limitation. However, the natural history of gynecological diseases including leiomyoma, endometrial polyps, and ovarian cysts in women not prescribed tamoxifen is already known in detail. Therefore, in our view, the results of this study do have intuitive value in clinical practice.
Gynecologists should be familiar with the effects of tamoxifen treatment to avoid unnecessary surgery [
6]. Despite a few limitations, this study provides important information regarding the effects of tamoxifen in Korean women. Further prospective studies are warranted to gain a better understanding in this context.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download