This article has been
cited by other articles in ScienceCentral.
Abstract
Background
It is a very important social issue for Korea to have a healthy old age as an aged society. Aging causes a lot of physical changes, especially sarcopenia. Sarcopenia is defined as a persistent decrease in skeletal muscle and muscle strength. Sarcopenic obesity is a phenomenon in which fat is replaced instead of muscle. The purpose of this study was to examine the prevalence of sarcopenia and sarcopenic obesity in Korean elderly and to analyze the relationship with chronic disease.
Methods
Data from the 2008 to 2011 the Korea National Health and Nutrition Survey were used. A total of 3,492 patients were classified into 3 groups (non-sarcopenia, sarcopenia, sarcopenic obesity), and general, anthropometry, health behavior, nutrient intake and chronic disease status were compared by the statistical analysis.
Results
The rate of moderate exercise was significantly lower in the sarcopenia and sarcopenic-obesity group than in the non-sarcopenia group (P=0.007). The sarcopenic obesity group had significantly higher energy (P=0.005), protein (P=0.046) and fat (P=0.001) intake than the sarcopenic group. The sarcopenic-obesity group had the highest ratio of diabetes (P=0.023) and dyslipidemia (P=0.004) in the 3 groups. Compared with the non-sarcopenia group, in the sarcopenia and sarcopenic obesity groups, the odds ratios (ORs) of diabetes was increased by 1.24 and 2.16 while the ORs of dyslipidemia was increased by 1.12 and 1.50, respectively.
Conclusions
Regular exercise and adequate nutrient intake (energy, protein and fat) are essential for the prevention of sarcopenia in Korean elderly, and management of chronic disease in sarcopenic obesity elderly is important.
Keywords: Aged, Chronic disease, Healthy lifestyle, Obesity, Sarcopenia
INTRODUCTION
Sarcopenia means a decrease in muscle mass and muscle strength caused by decreased synthesis or increased degradation of muscle protein.[
1] Aging reportedly affects the musculoskeletal system, nervous system, and hormonal changes and causes nutritional state imbalance and inflammation, which in turn affects sarcopenia.[
2] The incidence of sarcopenia has been increasing each year, and it is considered to be a serious social concern which gives rise to high medical cost.[
3] Recently, the concept of Sarcopenic obesity has been emphasized in the academia regarding the physiological mechanism of muscle reduction, increase of body fat, and redistribution of body fat. The sarcopenic obesity tend to be more exposed to the risk of disease than the isolated condition of sarcopenia or obesity.[
4]
Sarcopenia is associated with various factors, including chronic illness, inadequate nutrition, and reduced physical activity. The risk of sarcopenia is known to increase in individuals who engage in very little physical activity or have an inadequate sleep pattern.[
56] Furthermore, the risk of sarcopenia even increases in those who are infrequent smokers or alcohol consumption [
7] as well as those with a low serum vitamin D level.[
8] Aging increases body fat and insulin resistance, resulting in chronic illness as well as reduction in muscle strength and muscle quality; therefore, because muscle mass decreases with age, sarcopenia is recognized as a problem associated with aging. Despite the relevance of these various factors, domestic studies regarding the incidence of sarcopenia and sarcopenic obesity remain limited. Based on the results of previous studies, we hypothesized that there is a difference in lifestyle in patients with sarcopenia or sarcopenic obesity, and that chronic disease prevalence will be different.
Therefore, this study was conducted to investigate the incidence of sarcopenia and sarcopenic obesity in Koreans elderly and to compare the relationship between various health related factors and disease using Korean big data.
METHODS
1. Study subject
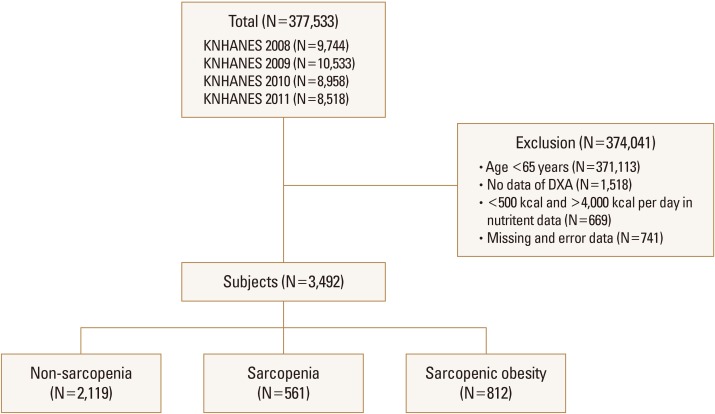
This study used data from the Korea National Health and Nutrition Survey (KNHANES) conducted from 2008 to 2011. Of the total subjects, the data of only men and women aged ≥65 years were first extracted (n=6,420), and that of only 3,492 subjects were analyzed after excluding the subjects who had missing values for multiple variables (n=2,928). The flow chart of the subjects were showed in
Figure 1. All subjects were classified into 3 groups (non-sarcopenia, sarcopenia, and sarcopenic obesity). Muscle mass decreased by dual energy X-ray absorptiometry (DXA), was divided by body weight and calculated as a percentage. When the calculated value was less than 1 standard deviation (SD), it was classified as sarcopenia.[
9] Sarcopenic obesity was defined as sarcopenia accompanies by a waist circumference of 90 cm for males or >85 cm for females (
Fig. 1).[
9]
2. Study variables
In general, age, sex, household income (low, middle-low, middle-high, high), education level (lower than elementary school, middle school, high school, university), body mass index (BMI), waist circumference, and muscle mass were used as anthropometric data in the KNHANES. We used the results associated with physical activity (vigorous, moderate), smoking and drinking status, nutrient intake (energy, carbohydrate, protein, and fat) and analyzed the comorbid conditions of the subjects such as hypertension, diabetes mellitus, dyslipidemia, and osteoporosis.
3. Statistical analysis
SPSS 18.0 programs (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis and, to identify differences among the 3 groups, means and SDs were analyzed by one-way analysis of variance (ANOVA) and frequency was analyzed by χ2 test. When significant difference appeared among the groups, turkey's multi-range test was conducted as post-hoc test. Odds ratios (ORs) were calculated using multinomial logistic regression to estimate the association be-tween disease and various factors. Adjusted ORs were derived after adjusting the covariates. The proportional changes and 95% confidence intervals (CIs) were calculated using the exponentiation of the coefficients, which means that the proportional changes in the arithmetic mean were associated with each level of covariate relative to a reference level. All P-values of less than 0.05 were considered to indicate statistical significance.
RESULTS
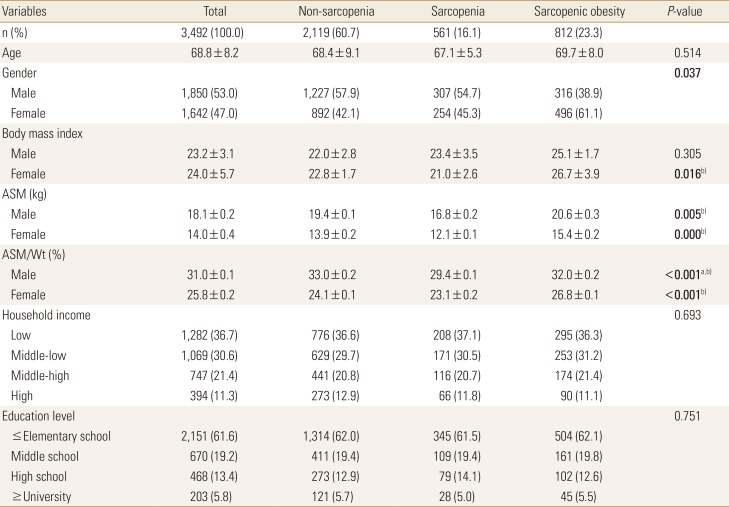
1. Demographic factors of the subjects
Among the subjects, 60.7% were classified under the non-sarcopenia group. Sarcopenia group was 16.1% and sarcopenic obesity group was 23.3%. Among the 3 groups, the sarcopenic obesity group had a slightly higher number of females and higher BMI. Appendicular skeletal muscle (ASM) and ASM/weight (%) were significantly higher in the sarcopenic obesity group than in the sarcopenia group. There were no significant differences in household income and educational level among the 3 groups (
Table 1).
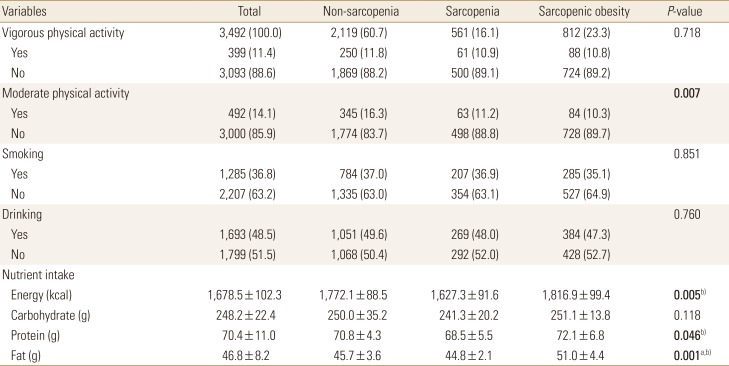
2. Health behavior and nutrient intake of the subjects
Among the 3 groups, moderate exercise and nutrition levels showed the most significant differences. Overall, the exercise rate among the subjects was low, smoking rate was 36.8%, and the alcohol consumption rate was 48.5%. The rate of moderate physical activity was significantly lower in patients belonging to the sarcopenia group and sarcopenic obesity group than in those belonging to the non-sarcopenia group. In the sarcopenic obesity group, energy, protein, and fat intake were significantly higher than those in the sarcopenia groups (
Table 2).
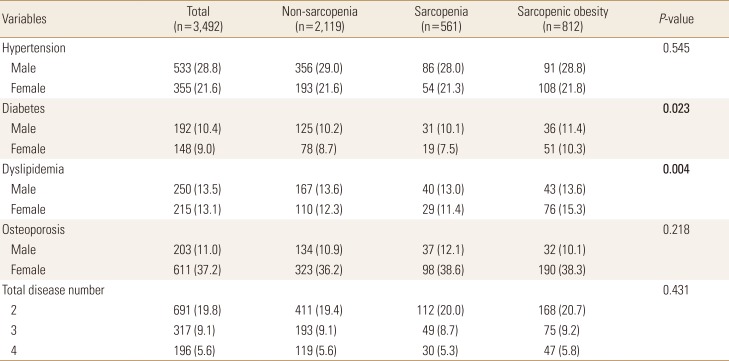
3. Disease status of the subjects
The overall incidence rate for hypertension was 25.2%; diabetes, 9.7%; dyslipidemia, 13.3%; and osteoporosis, 24.1%. Except for osteoporosis, the incidence rate for all other diseases was higher among men. Incidence of diabetes and dyslipidemia were significantly higher in the sarcopenic obesity group. There was no significant difference with regard to the number of 4 diseases (hypertension, diabetes, dyslipidemia, and osteoporosis) among the 3 groups. In the total subjects, 19.8% of the subjects had 2 disease, 9.1% had 3 disease, and 5.6% had 4 disease, respectively (
Table 3).
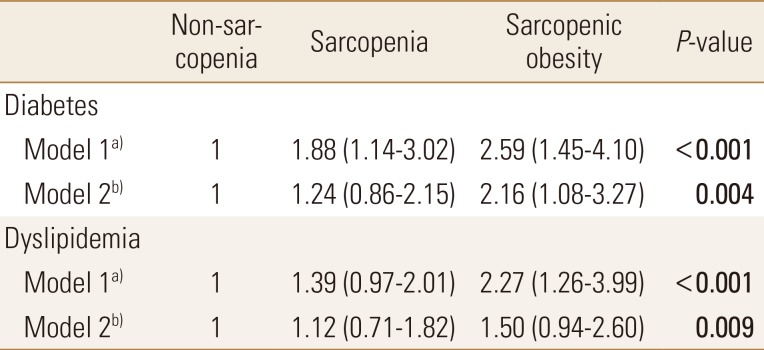
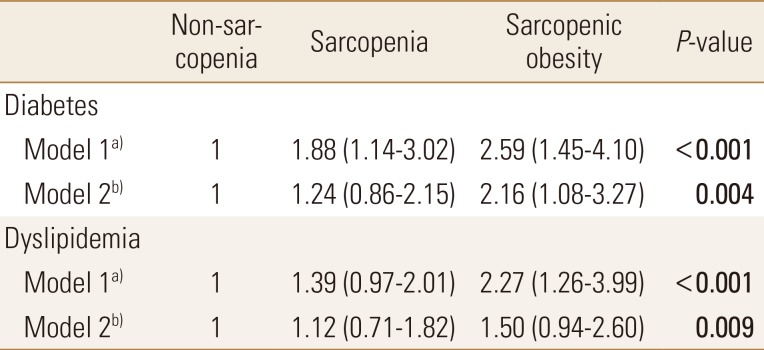
4. Risk of chronic disease according to sarcopenia
In the previous results, diabetes and dyslipidemia were significantly different between the 3 groups, and the ORs of diabetes and dyslipidemia in sarcopenia and sarcopenic obesity groups was analyzed. Compared with the non-sarcopenia group, in the sarcopenia and sarcopenic obesity groups, the ORs of diabetes was increased by 1.24 (95% CI, 0.86–2.15) and 2.16 (95% CI, 1.08–3.27) while the ORs of dyslipidemia was increased by 1.12 (95% CI, 0.71–1.82) and 1.50 (95% CI, 0.94–2.60), respectively (
Table 4).
DISCUSSION
In this study, we compared the lifestyle and chronic disease status by analyzing the sarcopenia in Korean elderly. It is known that the reduction in sex hormone levels, caused by aging, is an important cause of sarcopenia and sarcopenic obesity.[
2] Moreover, an increase in the levels of inflammatory cytokines accelerates muscle catabolism and aggravates sarcopenia.[
10] The prevalence of sarcopenia was reported to be 14.1% in the Chinese population and 30.3% in a local study conducted in Korea.[
11] In our study, the prevalence of sarcopenia was 16.0% and that of sarcopenic obesity was 23.3%. Moreover, the results of our study suggest that the incidence rate of sarcopenia is higher in males and that of sarcopenic obesity is higher in females because postmenopausal muscle strength decreases and body fat increases more rapidly. According to previous studies,[
12] the risk of sarcopenia is higher among individuals who live alone in the city than among those who live alone in the rural area; it is also increased in individuals with lower education and economic levels. The prevalence of the sarcopenia differs for different populations. There is currently no standardized diagnostic criteria for sarcopenia, so there is a limit to compare accurately. Therefore, a systematic study is needed.
Physical activity and nutritional intake reportedly affected sarcopenia. Exercise is the key to preventing sarcopenia.[
5] Less physical activity reduces limb muscle mass. Reduction in the number and size of muscle fibers is caused by a decrease in muscle cell death and physical stimulation when there is little physical activity. Low muscle mass and low physical activity levels constitute a vicious cycle and cause a decrease in total energy expenditure, leading to muscle-reducing obesity.[
13] In the present study, the rate of exercise was significantly lower in the sarcopenia and sarcopenic obesity groups than in the non-sarcopenia group. Good nutritional status is associated with sarcopenia prevention.[
14] Energy and protein intake at lower than the recommended levels is associated with a higher risk of sarcopenia.[
15] In this study, nutritional management was found to be the most essential in sarcopenic obesity group having significant differences in energy, protein, and fat intake, excluded carbohydrate intake.
It is reported that muscle weakness is related to several diseases,[
16] but reduction in muscle strength is greater in individuals with chronic diseases such as diabetes and cardiovascular disease. Blood pressure, triglycerides, and fasting blood glucose are all associated with sarcopenia in individuals aged >60 years old.[
17] Insufficient muscle mass causes greater insulin resistance.[
18] Sarcopenia may increase the risk of disease occurrence, and conversely, sarcopenia may worsen owing to an underlying disease. The prevalence of diabetes mellitus and dyslipidemia was significantly higher in the sarcopenia and sarcopenic obesity groups compared with the non-sarcopenia group.
This study is limited in that cross-sectional studies could not reveal the causal relationship between sarcopenia, sarcopenic obesity and the risk of developing chronic diseases. Further research is warranted to clarify the mechanism. However, it is meaningful that we investigated at the lifestyle and diseases state in elderly with sarcopenia using the Korean big data. And it can be deduced that increasing the muscle mass is essential to prevent and manage chronic diseases.
CONCLUSIONS
The results of the present study indicate that elderly people have a high incidence of sarcopenia, and the prevalence of obesity is especially high in women. Additionally, in the sarcopenic obesity group, physical activity was low, nutrient intake was excessive, and the risk of diabetes or dyslipidemia was high. Therefore, a personalized exercise strategy tailored according to age and sex is necessary to manage the health of the elderly. Balanced nutrition should be taken into consideration, and individuals with sarcopenic obesity should be more cautious regarding disease prevention and management.
Fig. 1
Flow chart of subjects on KNHANES data 2008 to 2011. KNHANES, the Korea National Health and Nutrition Examination Survey; DXA, dual energy X-ray absorptiometry.
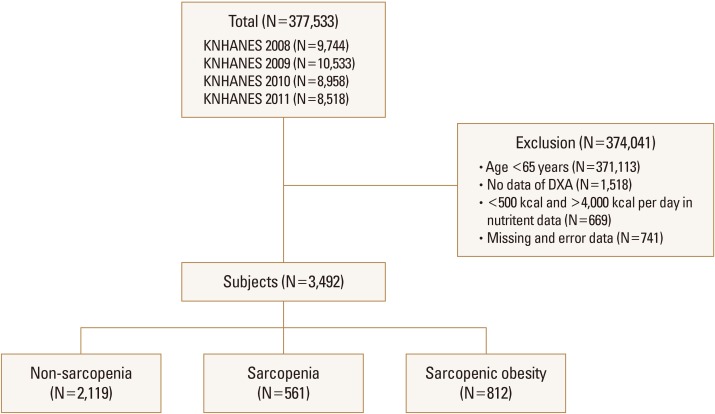
Table 1
General characteristics in the subjects
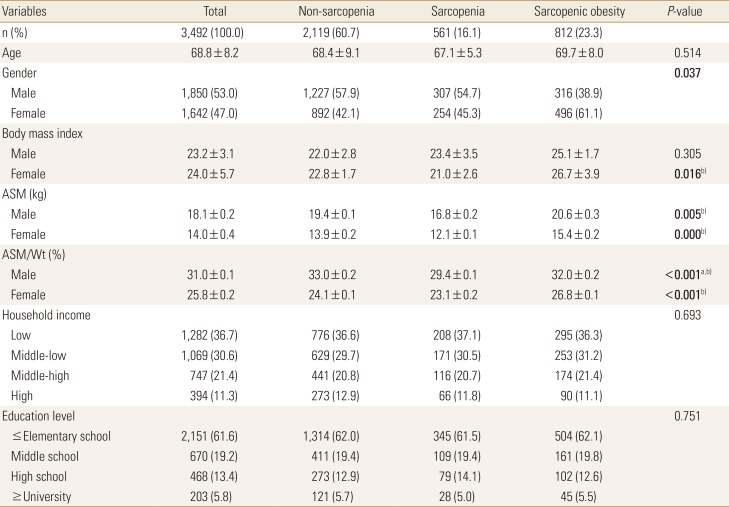
Table 2
Health behavior and nutrient intake in the subjects
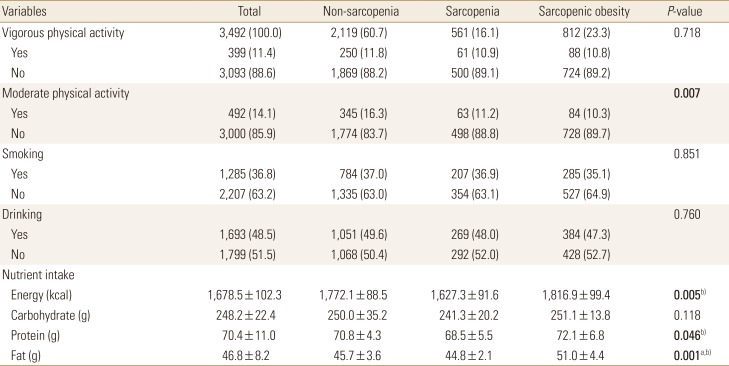
Table 3
Disease status in the subjects
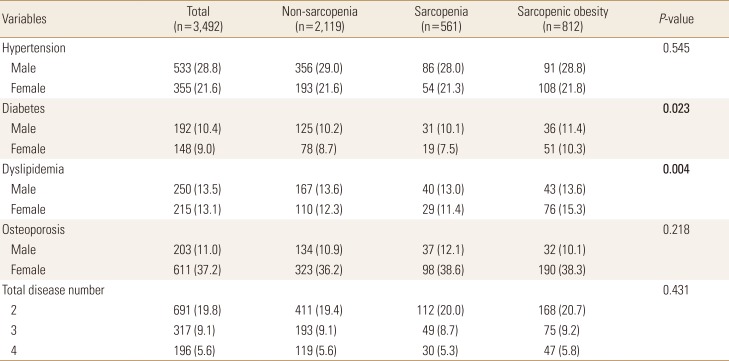
Table 4
Multivariate regression analysis of disease odds ratios in the subjects




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download