Abstract
Background
It is still unclear the ideal vitamin D dosage once the deficiency and insufficiency is treated. Once deficiency was corrected we prospectively treated patients with 2,000 IU of vitamin D3 to check whether this dosage is enough to keep them above the 30 ng/mL of 25-hydroxy-vitamin D (25[OH]D).
Methods
One hundred and thirty-five Saudi Arabian men and women treatment naïve for the vitamin D deficiency and insufficiency were part of this study. History and clinical examination were done to rule out any metabolic bone disease. Weight and height was taken to calculate the body mass index (BMI). Patients who were vitamin D deficient (≥30 ng/mL), a standard treatment of 50,000 IU of vitamin D3 weekly for 3 months, a blood test for the vitamin D levels at the end of 3 months, maintenance dose of 2,000 IU of vitamin D3 for 3 months and a third blood sample after 3 months.
Results
The data for 128 patients was available for analysis. The average age was 44.95±12.97 years with the mean BMI of 29.60±2.59 kg/m2. The baseline 25(OH)D level was 13.16±3.30 ng/mL. The increase in the level of 25(OH)D on 50,000 IU weekly was significant from 13.16±3.3 ng/mL to 36.97±4.67 ng/mL (P<0.001) and then 2,000 IU daily for next 3 months, the level of 25(OH)D dropped top 20.38±5.42 ng/mL (P<0.001).
Go to : 
It was recognized as early as 1860's that vitamin D is important for bone health and recently its importance in extra-skeletal health has come to light. Vitamin D deficiency has been reported around the globe. Most of patients develop due to inadequate exposure to sunlight and eating less of vitamin D containing foods.[1] Fortification of commonly used food items was one source of supplementation of vitamin D.
Till the year 2000, in United States (US) the recommended vitamin D daily dose for men and women of ≤50 years was 200 IU/day.[234] Currently the Recommended Dietary Allowance for vitamin D established by the Institute of Medicine is 600 international units per day until we reach 70 years of age, and 800 IU per day thereafter and raised the safe upper limit to 4,000 IU daily [5] and this is based on 20 ng/mL (50 nmol/L) as adequate. Whereas The Vitamin D Council recommends that healthy adults take 2,000 IU of vitamin D daily.[6]
Different protocols have been recommended to treat vitamin D deficiency. One protocol suggests 50,000 IU of vitamin D3 orally once weekly for 2 to 3 months, or 3 times weekly for 1 month.[7] But if vitamin D2 is used the levels with the same dosage does not reach the normal of 30 ng/mL in the 3 month period.[89] What is more important is once the targeted normal level of 30 ng/mL is reached, many patients do not get adequate vitamin D maintenance dosing.
It is presently believed that a maintenance daily dose of 800 to 2,000 IU may be enough irrespective of the weight of the patients, even though Holick and Colleagues [7] recommended that people of body mass index (BMI) >30 kg/m2 require a daily vitamin D dose equal to 3 times greater that of normal body weight patients. We have observed with the daily maintenance dose of 2,000 IU patients were reverting back to the deficiency and insufficiency status. With the objective to find the true status of vitamin D levels post maintenance dose of 2,000 IU for 3 months this prospective study was carried out.
Go to : 
Approval of the study was obtained from the Institutional Review Board of Imam AbdulRahman Bin Faisal University, Dammam (IRB No. 061/2016). One hundred and thirty-five Saudi Arabian men and women treatment naïve for the vitamin D deficiency and insufficiency were part of this study which was conducted between October 2016 and December 2017. The inclusion criteria was treatment naïve for vitamin D deficiency and insufficiency, will give informed consent, agree for follow up and will not change the study protocol, which was a standard treatment of 50,000 IU of vitamin D3 weekly for 3 months, a blood test for the vitamin D levels at the end of three months, maintenance dose of 2,000 IU/day of vitamin D3 for three months and a third blood sample after 3 months. Exclusion criteria was patients whose history suggestive of metabolic bone disease, renal failure or any other auto-immune disease. History and clinical examination were done to rule out any metabolic bone disease. Weight and height was taken to calculate the BMI. Baseline blood hematology, biochemistry, and bone panel were also done. Vitamin D sufficiency defined 25-hydroxy-vitamin D (25[OH]D) level of ≥75 nmol/L (≥30 ng/mL), insufficiency as 50 to 75 nmol/L (20–30 ng/mL), and deficiency as ≤50 nmol/L (≤20 ng/mL). The data was entered in the data base and analyzed using the SPSS software, version 21.0 (SPSS Inc., Chicago, IL, USA).
Go to : 
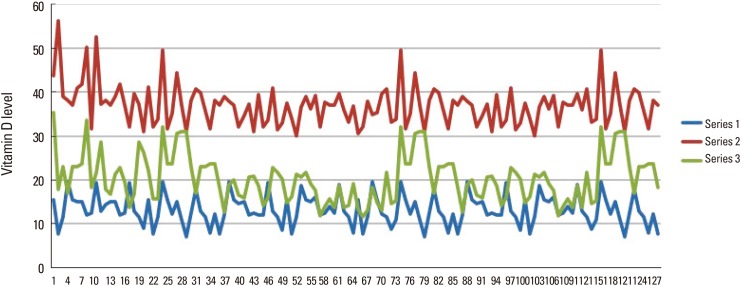
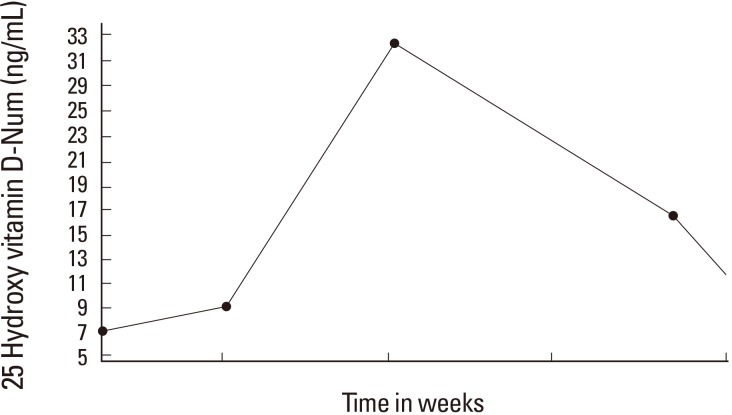
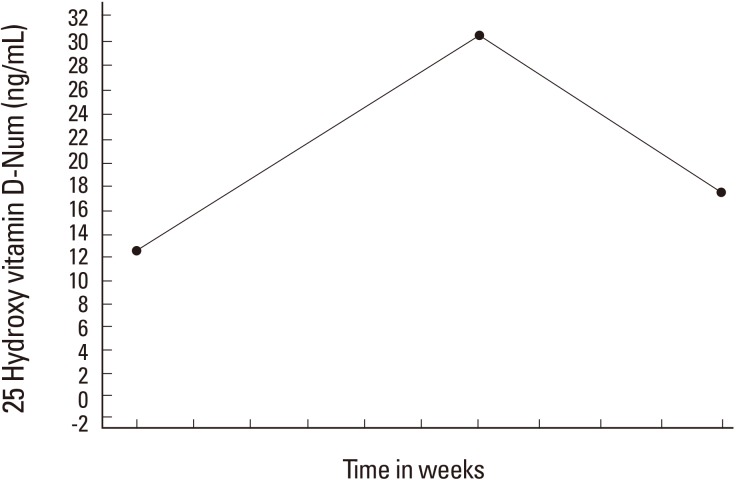
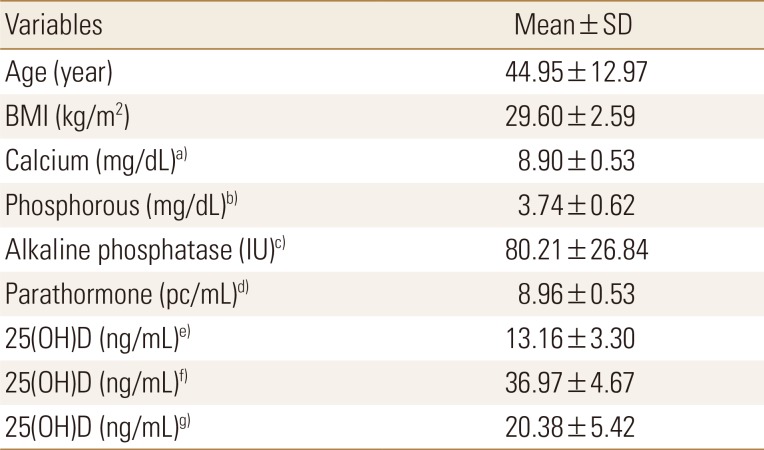
The data for 128 patients were available for analysis. Seven patients were excluded as 6 patients started taking calcium preparation twice daily which had 600 IU of vitamin D3 and 1 patient moved out of the region and did not come for follow up. The data for 128 patients were available for analysis. The average age was 44.95±12.97 years with the mean BMI of 29.60±2.59 kg/m2. The baseline 25(OH)D level was 13.16±3.30 ng/mL intact parathyroid hormone level of 8.96±0.53 pc/mL. Table 1 gives the rest of the blood investigations, post treatment by 50,000 IU weekly for 3 months. The increase in the level of 25(OH)D on 50,000 IU weekly was significant from 13.16±3.30 ng/mL to 36.97±4.67 ng/mL (P<0.001) and then 2,000 IU daily for next three months, the level of 25(OH)D dropped top 20.38±5.42 ng/mL (P<0.001). Figure 1 shows the graphic picture of the 3 levels of 25(OH)D. Only 14 (10.9%) patients continued to maintain above 30 ng/mL of 25(OH)D on 2,000 IU maintenance dose. Figure 2 and 3 shows the graphs of the levels of 25(OH)D treated with 50,000 IU weekly for 3 months and 2,000 IU for next 3 months.
Go to : 
Our study shows that once normal level of 25(OH)D is reached, the daily maintenance dose of 2,000 IU was insufficient to maintain the normal level and significantly dropped to 20.38±5.4 ng/mL. This suggests that the maintenance dose of 2,000 IU daily is not sufficient to keep the 25(OH)D at normal level of ≤30 ng/mL. Vitamin D is essential for the bone health and recently extra-skeletal benefits were highlighted. To maintain normal levels of vitamin D daily dosage has been on the rise from 400 IU to 2,000 IU.[89] Regardless of initial dosage of vitamin D therapy to treat the deficiency, an adequate maintenance daily dose is essential to avoid recurrent deficiency. Recently the National Health Service in United Kingdom [10] suggested maintenance daily dose from 800 to 2,000 IU daily but added that it might require 4,000 IU daily as well. This was further emphasized by reports from other centers.[47111213]
It is logical a deficiency occurred due to lack of daily vitamin D either due to low intake or no exposure to sunlight, if we correct the levels to normal and reduce the treatment dose from 50,000 IU weekly to 2,000 IU daily and expect that the levels will remain at normal levels does not appear true. Moreover our patients having very low fortified diet with vitamin D, supplementation remains the only source of vitamin D. As in our patients we gave 7,142.8 IU daily for 3 months and suddenly dropped to 2,000 IU a day. Many caregivers assume that adequate vitamin D intake can be obtained by diet alone; hence a supplement of 2,000 IU is suggested.
The reasons of why 2,000 IU daily was not sufficient in our patients are probably for couple of reasons. Even in the developed countries only 20% of the daily requirement come from the fortified food. Largely consumed food in Saudi Arabia has a meager amount of fortification of vitamin D. A 250 mL of fresh milk gives only 100 IU as per the label on the container and none in the cereals and juices.[14] Recently US Food and Drug Administration nearly doubled the amount of vitamin D for fortification to ingredient to milk, and beverages from almonds, soy, coconut and plant-based yoghurts.[12] As exposure to sunlight remains the major source of vitamin D [215] and as the average temperature in Saudi Arabia during 6 months in a year is close to ≥40 degrees centigrade, women are reluctant to expose to the sun and the ideal time to get vitamin D from sunlight the menfolk are in their offices. As diet does not provide enough vitamin D in the diet, supplementation becomes essential part of the maintenance of vitamin D. Secondly our patients average BMI was close to 30 kg/m2 and it was suggested that obese individuals require 2 to 3 times the higher dose than patients of normal weight.[16]
The limitation of our study is the small number of the cohort group and even though we asked patients to not to change their habits some inadvertently might have exposed to sunlight, but has the strength, which raises concern to what maintenance dose is ideal to prevent insufficiency and deficiency. Even though we were careful enough to monitor compliance issues, we found the level to drop to the pretreatment level in the majority. In conclusion our study indicates that in our patients, the maintenance dose of 2,000 IU/day was not enough to keep the level of 25(OH)D close to the normal average. Since this study was carried out in one part of Saudi Arabia and the world, we strongly recommend more studies to confirm our findings.
Go to : 
References
1. Autier P, Boniol M, Pizot C, et al. Vitamin D status and ill health: a systematic review. Lancet Diabetes Endocrinol. 2014; 2:76–89. PMID: 24622671.

3. Holick MF. Resurrection of vitamin D deficiency and rickets. J Clin Invest. 2006; 116:2062–2072. PMID: 16886050.

4. Ross AC, Manson JE, Abrams SA, et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011; 96:53–58. PMID: 21118827.
5. Institute of Medicine. Dietary reference intakes for calcium and vitamin D. Washington, DC: The National Academies Press;2011.
6. Vitamin D Council. Vitamin D. 2018. cited by 2018 March 1. Available from: https://www.vitamindcouncil.org/.
7. Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011; 96:1911–1930. PMID: 21646368.

8. Kennel KA, Drake MT, Hurley DL. Vitamin D deficiency in adults: when to test and how to treat. Mayo Clin Proc. 2010; 85:752–757. quiz 7-8. PMID: 20675513.

9. Osborn J, Germann A, St Anna L. Clinical inquiries. Which regimen treats vitamin D deficiency most effectively? J Fam Pract. 2011; 60:682–683. PMID: 22049353.
10. Greater Manchester Medicines Management Group. Treatment of vitamin D deficiency and insufficiency in adults. 2016. cited by 2016 March 1. Available from: http://gmmmg.nhs.uk/docs/nts/NTS-Recommendation-on-Vitamin-D-deficiency-and-insufficiency-adults.pdf.
11. Pludowski P, Holick MF, Grant WB, et al. Vitamin D supplementation guidelines. J Steroid Biochem Mol Biol. 2018; 175:125–135. PMID: 28216084.

12. Haq A, Wimalawansa SJ, Pludowski P, et al. Clinical practice guidelines for vitamin D in the United Arab Emirates. J Steroid Biochem Mol Biol. 2018; 175:4–11. PMID: 27693095.

13. Choi HS, Min YK, Byun DW, et al. Korean society for bone and mineral research task force report: perspectives on intermittent high-dose vitamin D supplementation. J Bone Metab. 2017; 24:141–145. PMID: 28955689.

14. Sadat-Ali M, Al Elq A, Al-Farhan M, et al. Fortification with vitamin D: comparative study in the Saudi Arabian and US markets. J Family Community Med. 2013; 20:49–52. PMID: 23723731.

15. Food and Drug Administration. Food additives permitted for direct addition to food for human consumption; Vitamin D2. Fed Regist. 2016; 81:46578–46582.
16. Ekwaru JP, Zwicker JD, Holick MF, et al. The importance of body weight for the dose response relationship of oral vitamin D supplementation and serum 25-hydroxyvitamin D in healthy volunteers. PLoS One. 2014; 9:e111265. PMID: 25372709.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download