Abstract
Objectives
This study explored the association between a history of oligomenorrhea and onset of menopause and metabolic parameters.
Methods
The study population was 605 postmenopausal women who were patients at the Menopause Clinic, Maharaj Nakorn Chiang Mai Hospital, Chiang Mai, Thailand between February 2015 and December 2015. A questionnaire was used to ask all women about their history of oligomenorrhea. The study also collected medical data, including weight, height, waist circumference, blood pressure, and blood glucose and lipid profile.
Results
Of the 231 postmenopausal women with a complete data record, 31 had a history of oligomenorrhea and 200 did not. The age of onset of menopause was around 48 years in both groups. Prevalence of metabolic syndrome was 12.1%. More women with a waist circumference larger than 80 cm had a history of oligomenorrhea at the interview than women who had not, but a history of oligomenorrhea did not relate to other metabolic parameters. The adjusted odds ratio of a history of oligomenorrhea to waist circumference was 3.69 (95% confidence interval, 1.17–11.64).
Anovulation is a common gynecologic problem in women, usually presenting with either secondary amenorrhea or oligomenorrhea.1 The incidence of oligomenorrhea among the general population is around 13.5%.2 Nearly one half of women who reported oligomenorrhea have polycystic ovaries and higher serum luteinizing hormone and testosterone levels than women with a regular menstrual cycle.234 The most common cause of anovulation is polycystic ovary syndrome (PCOS).156 PCOS is associated with many health problems, including metabolic syndrome and cardiovascular disease.78 Other causes of anovulation, such as thyroid disease, hyperprolactinemia, and congenital adrenal hyperplasia, also associated with cardiovascular disease in both young and old patients.9101112131415 No study has followed these group of anovulatory patients from their reproductive stage until they pass through menopause. So, how anovulation/PCOS affects menopause is still unknown. Despite limited research, PCOS patients likely experience less severe symptoms as they getting older,16,17 and they tend to start menopause later than normoovulatory women.181920 In addition, postmenopausal women with either a prior history of menstrual cycle irregularity or PCOS might be at greater risk of metabolic syndrome.1721
Menopause is an important period in a woman's life; as the population ages, better health services for menopausal women are needed. Metabolic syndrome is important as associated with cardiovascular disease;22 physicians should recognize metabolic syndrome and also metabolic parameters, so they can provide appropriate disease management to this high risk group, thereby reducing cardiovascular events. This study aimed to shed light on the effect of oligomenorrhea on menopause by analyzing its correlation with age of onset of menopause and incidence of metabolic syndrome.
This study was conducted at the Menopausal Clinic, Maharaj Nakorn Chiang Mai Hospital, Thailand from February to December 2015. The Ethics Committee of the Faculty of Medicine, Chiang Mai University approved this study (OBG-2557-027880). All Thai women visiting our clinic during the study period who met the following criteria - aged 40 to 80 years and diagnosed as being in natural or surgical menopause after age 39 were asked to participate in an interview on a voluntary basis.
The interviews were designed to gather any underlying disease status, surgical history, hormone usage, and menstrual history without the use of any affecting medication from age 20 to 40 years. We also collected their medical data, including weight, height, waist circumference, blood pressure, and laboratory results of fasting blood glucose and lipid profile at the first diagnosis of menopause and the current visit.
The age of onset of menopause was defined as the age at which a woman experienced amenorrhea for one year. Women with a history of oligomenorrhea were defined as those having irregular menstruation with intervals lasting more than 35 days, but not longer than 6 months during the majority (80%) of their reproductive stage (20–40 years of age). Metabolic syndrome was diagnosed if a woman met 3 of the 5 criteria identified in “Harmonizing the Metabolic Syndrome: a Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity”.23 These are: 1) waist circumference ≥80 cm in women (cut-off point in Asians);2425 2) serum triglyceride level ≥150 mg/dL or on drug treatment for elevated triglycerides; 3) serum high-density lipoprotein cholesterol (HDL-C) < 50 mg/dL or on drug treatment for reduced HDL-C; 4) systolic blood pressure ≥130 mmHg, diastolic blood pressure ≥85 mmHg or on antihypertensive drug treatment with a history of hypertension; and 5) fasting glucose ≥100 mmHg or on drug treatment for elevated glucose.
Patients with any of the following were excluded from this study: 1) missing or incomplete medical data; 2) no history of menstruation; 3) an endocrine disorder or other chronic disease that affected malnutrition; 4) a history of chemotherapy or radiation; or 5) had ever used any medications or substances that affected menstruation, such as herbs, contraceptive medication, or hormonal treatment that was not menopausal hormonal therapy without a drug-free period.
In the absence of any previous study on the history of oligomenorrhea in menopausal women, we first conducted a pilot study using a questionnaire, interviews, and medical record review. It revealed that of 7 menopausal women with a history of oligomenorrhea, around 80% had a waist circumference greater than 80 cm, and of 120 without oligomenorrhea, only 40%. The sample size was calculated by stipulating the alpha error at 0.05 (95% confidence or 5% significance level) and a beta error equal to 0.1 (power 1-β = 90%) for the 2 independent groups. From the pilot study, this generated a needed sample size of 30 in the group of menopausal women with a history of oligomenorrhea to be able to compare differences in waist circumference with the group of women with a history of normal menstruation.
All statistical analyses were carried out using SPSS version 22.0 for Windows (SPSS Inc., Chicago, IL, USA), a combination of 3 packages (data preparation, advanced statistics, and statistics based), IBM Singapore Pte Ltd. (Changi, Singapore). A normality test was performed to confirm which variables were normally distributed. Discrete data were analyzed as frequency and percentages. Continuous variables were compared using an independent t-test or non-parametric Mann-Whitney U test. Categorical variables were compared using a χ2 test. A multivariate logistic regression was performed to assess individual risks. Results were reported as mean value ± standard deviation and categorical values were expressed in relative frequency. A P value of less than 0.05 was considered significant.
Six hundred and five postmenopausal women participated in this study. There were thirty-one women were excluded for incomplete data and 3 due to a history of hyperprolactinemia or the continuation of hormonal contraception without a free period of abstinence. Thirty-one women had a history of oligomenorrhea. The control group consisted of 200 postmenopausal women selected randomly by an internet randomizer program from 540 women with a history of normal menstruation. The mean age and body mass index (BMI) of the 540 women with a history of normal menstruation and the 200 who were selected randomly were not statistically different.
Baseline characteristics are shown in Table 1. Women with a history of oligomenorrhea had a higher BMI and a higher proportion of surgical menopause compared to those with a history of normal menstruation. The waist circumference from the start of menopause was neither measured nor recorded.
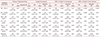
There was no significant difference in the number of patients with abnormal metabolic parameters in either group at the first visit to the menopause clinic. The prevalence of metabolic syndrome was 12.1%. More women had a waist circumference of more than 80 cm in the oligomenorrhea group at the time of interview, as shown in Table 2.
The factors that might affect metabolic parameters are BMI and surgical menopause. Multivariate analysis was applied to assess their relationship and the results are shown in Table 3. BMI was the major factor affecting metabolic syndrome in postmenopausal women.
The prevalence of oligomenorrhea among the general population is 13.5%.2 The most common cause of anovulation is PCOS,1 which occurs in 7% to 10% of reproductive women.56 The prevalence of 5.43% of postmenopausal women with a history of oligomenorrhea in this study was lower than expected. This low prevalence might have been affected by recall bias, as the mean age of participants in this study was 59 years old. However, women with a history of oligomenorrhea might have a more obvious menstruation problem than those with a history of normal menstruation.
This study found that the BMI at menopause was no different between women with a history of normal menstruation and those with oligomenorrhea, at around 23 to 25 kg/m2, which corresponded with a previous study.26 For the women in this study, BMI increased after menopause, and those with a history of oligomenorrhea had a higher BMI and bigger waist circumference than those with a history of normal menstruation. As the basal metabolic rate decreases with aging,2728 the BMI typically increases after 10 years of menopause. However, women with oligomenorrhea might have had problems related to hormone disturbance and glucose metabolism since they were young,315 contributing to their larger weight gain. BMI significantly affects metabolic parameters and health problems.293031 The adjusted odds ratio in this study revealed that a history of oligomenorrhea related to the chance of having a waist circumference of more than 80 cm; while this is a discrete variable, it could also have been associated with high BMI. As waist circumference is a factor in diagnosing metabolic syndrome, which is linked to cardiovascular disease,23 awareness needs to be raised of the increased risk of metabolic syndrome in reproductive women with anovulation and menopausal women with prior oligomenorrhea.
The majority of women participating in this study were healthy at their first menopause visit, and the prevalence of hypertension, impaired glucose tolerance, hypertriglyceridemia, and low HDL-C was similar to those published in a previous study of women aged between 40 and 49 years old.32 In general, the prevalence of hypertension, impaired glucose tolerance, hypertriglyceridemia, and low HDL-C increases with age.3233 In this study, however, the prevalence of these metabolic problems did not change much over 10 years. This study found a prevalence of metabolic syndrome of 12.1% among the women interviewed, very low compared to some previous studies that reported 34% to 45% in women aged 50 to 59 years old,3234 but similar to Indhavivadhana et al.35, who found a prevalence of 15.9% (13.6–18.2%) in Thai perimenopausal and postmenopausal women. These differences across ethnicities might reflect different lifestyles. The women participating in this study and Indhavivadhana et al.35 attended the Menopause Clinic, where they received appropriate health education and health surveillance, perhaps benefitting from better health care than the general population.
The median age of menopause among Thai females is 49.5 ± 3.6 years,36 which is a little younger than other ethnicities; i.e., 51.4 for African-American and Caucasian, 51.8 for Japanese, 51.5 for Chinese, and 51.0 for Hispanics.37 Earlier natural menopause is independently associated with several factors: current smoking, lower educational level, unmarried, unemployed, ethnicity, and a history of heart disease. The mean age at menopause of the northern Thais in this study was around 48 years old, in both those with oligomenorrhea and regular menstruation.
In this study, surgical menopause was more common among women with a history of oligomenorrhea. The anovulation relates to abnormal uterine bleeding, endometrial hyperplasia, and endometrial cancer;38 while these may be reasons for hysterectomy, clear records were not available in this study.
The strength of this study was that the data were collected from a large homogenous population with a long follow-up period attending the same menopause clinic. However, there could be some recall bias and missing data. A prospective study with a specific group of patients and larger sample size would provide a clearer conclusion.
Figures and Tables
Table 1
Comparison of characteristics between postmenopausal women with a history of normal menstruation and those with a history of oligomenorrhea

Table 2
Comparison of the number of women with abnormal metabolic parameters between the group with a history of oligomenorrhea and those with a history of normal menstruation at their first menopause visit and at the time of interview

Acknowledgement
The authors would like to acknowledge the nurses, resident trainees and staff at the Menopause Clinic, Chiang Mai University for their invaluable help in recruiting the patients. We would also like to thank all partciipating patients.
References
1. Chandeying P, Pantasri T. Prevalence of conditions causing chronic anovulation and the proposed algorithm for anovulation evaluation. J Obstet Gynaecol Res. 2015; 41:1074–1079.

2. Taponen S, Martikainen H, Järvelin MR, Laitinen J, Pouta A, Hartikainen AL, et al. Hormonal profile of women with self-reported symptoms of oligomenorrhea and/or hirsutism: Northern Finland birth cohort 1966 study. J Clin Endocrinol Metab. 2003; 88:141–147.

3. Rickenlund A, Eriksson MJ, Schenck-Gustafsson K, Hirschberg AL. Amenorrhea in female athletes is associated with endothelial dysfunction and unfavorable lipid profile. J Clin Endocrinol Metab. 2005; 90:1354–1359.

4. Taponen S, Ahonkallio S, Martikainen H, Koivunen R, Ruokonen A, Sovio U, et al. Prevalence of polycystic ovaries in women with self-reported symptoms of oligomenorrhoea and/or hirsutism: Northern Finland Birth Cohort 1966 Study. Hum Reprod. 2004; 19:1083–1088.

5. March WA, Moore VM, Willson KJ, Phillips DI, Norman RJ, Davies MJ. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod. 2010; 25:544–551.

6. Baptiste CG, Battista MC, Trottier A, Baillargeon JP. Insulin and hyperandrogenism in women with polycystic ovary syndrome. J Steroid Biochem Mol Biol. 2010; 122:42–52.

7. Norman RJ, Dewailly D, Legro RS, Hickey TE. Polycystic ovary syndrome. Lancet. 2007; 370:685–697.

8. Pantasri T, Vutyavanich T, Sreshthaputra O, Srisupundit K, Piromlertamorn W. Metabolic syndrome and insulin resistance in Thai women with polycystic ovary syndrome. J Med Assoc Thai. 2010; 93:406–412.
9. Biondi B, Klein I. Hypothyroidism as a risk factor for cardiovascular disease. Endocrine. 2004; 24:1–13.

10. Charmandari E, Chrousos GP. Metabolic syndrome manifestations in classic congenital adrenal hyperplasia: do they predispose to atherosclerotic cardiovascular disease and secondary polycystic ovary syndrome? Ann N Y Acad Sci. 2006; 1083:37–53.

11. Georgiopoulos GA, Stamatelopoulos KS, Lambrinoudaki I, Lykka M, Kyrkou K, Rizos D, et al. Prolactin and preclinical atherosclerosis in menopausal women with cardiovascular risk factors. Hypertension. 2009; 54:98–105.

12. Jiang XB, Li CL, He DS, Mao ZG, Liu DH, Fan X, et al. Increased carotid intima media thickness is associated with prolactin levels in subjects with untreated prolactinoma: a pilot study. Pituitary. 2014; 17:232–239.

13. Kim MS, Merke DP. Cardiovascular disease risk in adult women with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Semin Reprod Med. 2009; 27:316–321.

14. Souza LL, Guedes EP, Teixeira PF, Moreira RO, Godoy-Matos AF, Vaisman M. Serum TSH levels are associated with cardiovascular risk factors in overweight and obese adolescents. J Pediatr (Rio J). 2016; 92:532–538.

15. Taponen S, Martikainen H, Jarvelin MR, Sovio U, Laitinen J, Pouta A, et al. Metabolic cardiovascular disease risk factors in women with self-reported symptoms of oligomenorrhea and/or hirsutism: Northern Finland Birth Cohort 1966 Study. J Clin Endocrinol Metab. 2004; 89:2114–2118.

18. Li J, Eriksson M, Czene K, Hall P, Rodriguez-Wallberg KA. Common diseases as determinants of menopausal age. Hum Reprod. 2016; 31:2856–2864.

19. Saxena R, Bjonnes AC, Georgopoulos NA, Koika V, Panidis D, Welt CK. Gene variants associated with age at menopause are also associated with polycystic ovary syndrome, gonadotrophins and ovarian volume. Hum Reprod. 2015; 30:1697–1703.

20. Tehrani FR, Solaymani-Dodaran M, Hedayati M, Azizi F. Is polycystic ovary syndrome an exception for reproductive aging? Hum Reprod. 2010; 25:1775–1781.
21. Solomon CG, Hu FB, Dunaif A, Rich-Edwards JE, Stampfer MJ, Willett WC, et al. Menstrual cycle irregularity and risk for future cardiovascular disease. J Clin Endocrinol Metab. 2002; 87:2013–2017.

22. Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010; 56:1113–1132.
23. Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009; 120:1640–1645.
24. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005; 112:2735–2752.
25. Hara K, Matsushita Y, Horikoshi M, Yoshiike N, Yokoyama T, Tanaka H, et al. A proposal for the cutoff point of waist circumference for the diagnosis of metabolic syndrome in the Japanese population. Diabetes Care. 2006; 29:1123–1124.

27. Poehlman ET. Menopause, energy expenditure, and body composition. Acta Obstet Gynecol Scand. 2002; 81:603–611.

28. Davis SR, Castelo-Branco C, Chedraui P, Lumsden MA, Nappi RE, Shah D, et al. Understanding weight gain at menopause. Climacteric. 2012; 15:419–429.

29. Han TS, Lean ME. A clinical perspective of obesity, metabolic syndrome and cardiovascular disease. JRSM Cardiovasc Dis. 2016; 5:2048004016633371.

30. Kyrou I, Randeva HS, Tsigos C, Kaltsas G, Weickert MO. Clinical problems caused by obesity. In : De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, editors. Endotext. South Dartmouth, MA: MDText.com, Inc.;2000.
31. Rutter MK, Sullivan LM, Fox CS, Wilson PW, Nathan DM, Vasan RS, et al. Baseline levels, and changes over time in body mass index and fasting insulin, and their relationship to change in metabolic trait clustering. Metab Syndr Relat Disord. 2014; 12:372–380.

32. Aekplakorn W, Kessomboon P, Sangthong R, Chariyalertsak S, Putwatana P, Inthawong R, et al. Urban and rural variation in clustering of metabolic syndrome components in the Thai population: results from the fourth National Health Examination Survey 2009. BMC Public Health. 2011; 11:854.

33. Aekplakorn W, Chariyalertsak S, Kessomboon P, Sangthong R, Inthawong R, Putwatana P, et al. Prevalence and management of diabetes and metabolic risk factors in Thai adults: the Thai National Health Examination Survey IV, 2009. Diabetes Care. 2011; 34:1980–1985.
34. Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002; 287:356–359.

35. Indhavivadhana S, Rattanachaiyanont M, Wongvananurak T, Kanboon M, Techatraisak K, Leerasiri P, et al. Predictors for metabolic syndrome in perimenopausal and postmenopausal Thai women. Climacteric. 2011; 14:58–65.

36. Chompootweep S, Tankeyoon M, Yamarat K, Poomsuwan P, Dusitsin N. The menopausal age and climacteric complaints in Thai women in Bangkok. Maturitas. 1993; 17:63–71.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download