Abstract
Backgrounds/Aims
Despite the advances in identifying risk factors, improving operative technique, and postoperative patient care, pancreatic leakage after pancreatic resection remains a highly debated topic. The aim of this study is to describe our technique and our initial experience with the intraoperative embolization of the main pancreatic duct with an Ethylene Vinyl Alcohol Copolymer (Onyx®).
Methods
Two patients of 63 and 64 years underwent pancreaticoduodenectomy for a cholangiocarcinoma of the extrahepatic bile duct and a pancreatic adenocarcinoma, respectively. At the time of pancreatic parenchyma resection, a Wirsung duct was identified and catheterized. A wirsungography was done and then, embolization with Onyx® was carried out under fluoroscopic control.
Results
Neither of the patients developed a postoperative pancreatic fistula. They were discharged to home on the 17th and 18th postoperative day, respectively. At the last follow-up, no recurrence was found. The two patients became diabetics; both needed the support of supplementary pancreatic enzymes.
Post-operative pancreatic fistula (POPF) is the most common and troublesome complication after pancreatic resection, with reported rates ranging from 3% to 45%.123 It represents the factor most often linked with postoperative complications, longer hospital stays, readmissions, increased costs, and, above all, more postoperative deaths.45 Despite advances in operative techniques and improvements in postoperative patient care, this subject remains highly debated in the literature.6 A very controversial issue is the obliteration of the main pancreatic duct with chemicals substances.789 Numerous substances and techniques have been described with very controversial results.101112 Onyx® (Medtronic, Heerlen, the Netherlands) is an liquid agent used for embolization of vascular structures; it consists of an ethylene vinyl alcohol copolymer (EVOH), made opaque with micronized tantalum powder. Onyx® provides a good contrast for visualization under fluoroscopy, and so is used especially in the field of vascular interventional radiology1314 but also for bile duct leakage.1516 To the best of our knowledge, the obliteration of the main pancreatic duct with Onyx® has not yet been described. We present our initial technical and clinical experience with two patients who were successfully treated by intraoperative Onyx® application.
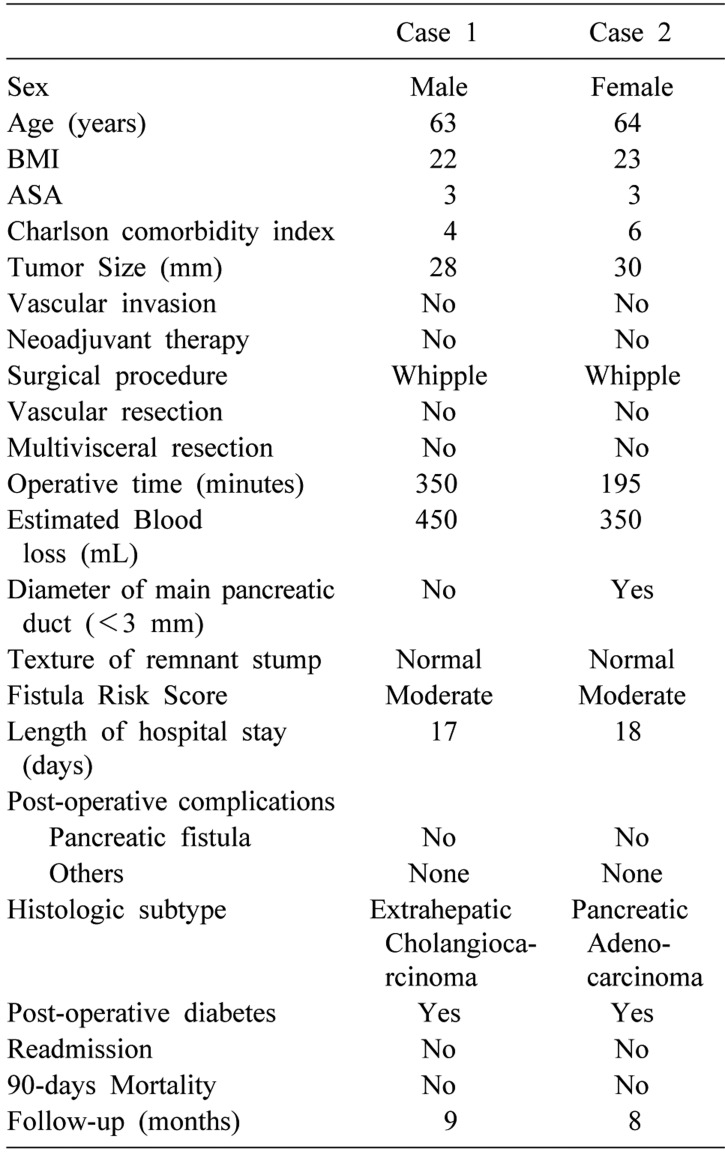
Two patients of 63 and 64 years came to our attention for a cholangiocarcinoma of the extrahepatic bile duct and pancreatic adenocarcinoma, respectively. After an accurate preoperative evaluation, the patients underwent pancreaticoduodenectomy (PD). In both cases, a Whipple resection was performed, and an extended lymphadenectomy with a third-level mesopancreas resection was carried out.
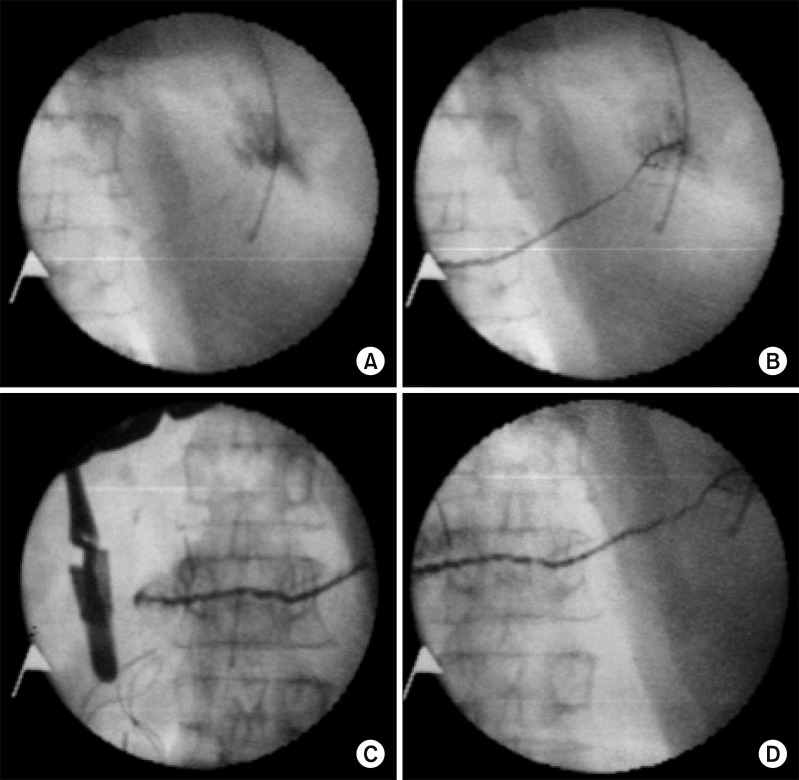
At the time of pancreatic parenchyma resection, the main pancreatic duct was identified and catheterized. An 18 G needle was placed into the Wirsung stump and, using fluoroscopic guidance, a hydrophilic microcatheter (Maestro, Merit) was introduced into the duct to reach the end of the pancreatic stump. After wirsungography, Onyx®, always under angiographic control, was slowly injected to embolize the main pancreatic duct and all secondary pancreatic branches. Immediate angiographic control after the embolization procedure demonstrated complete closure of the Wirsung (Fig. 1). After the embolization, the pancreatic extremity was further sectioned using an ECHELON FLEX™ (Ethicon, Cincinnati, OH, USA) stapling device, with a 45-mm white or blue cartridge depending on the thickness of the parenchyma. A hepaticojejunostomy was fashioned using a running 5/0 polydioxanone, and a gastroenterostomy was constructed using an ECHELON FLEX™ stapling device. Drainage was always placed in contact with the sectional pancreatic parenchyma, and two additional drains were placed in the perianastomotic sites.
Postoperative assessment included measurement of drainage and serum amylase on the first, third, and fifth postoperative day. An abdominal computed tomography (CT) scan was performed on the seventh postoperative day, and if no peripancreatic collection was detected, the drainages were removed gradually.
An enteral nutrition tube was placed beyond the gastroenterostomy during surgery, and enteral nutrition was started on the first postoperative day. Subcutaneous octreotide was not administered systematically.
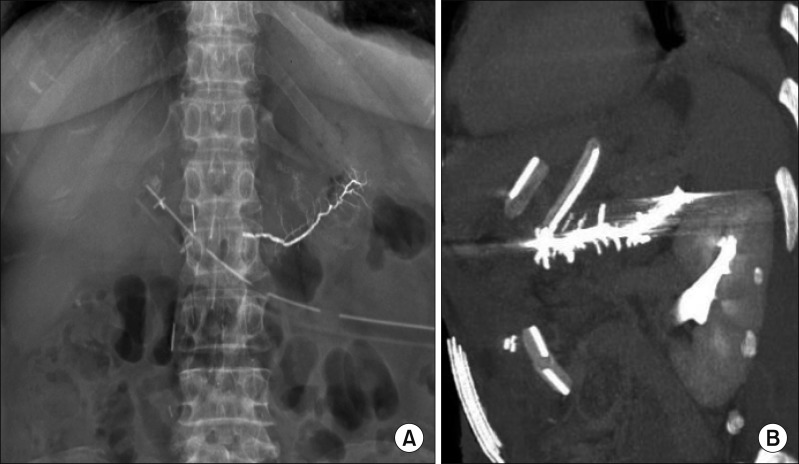
The details of the patients are summarized in Table 1. No perioperative complications related to the Onyx® application were observed. In the postoperative course, no biochemical leaks (grade A), grade B, or grade C POPF was identified. Dosages of the amylase level were always three times lower than the serum amylase activity. X-ray and thoracic-abdominal computed tomography performed on the 7th postoperative day (Fig. 2) confirmed the Wirsung mold, correlatable to total occlusion of the ducts, and no peripancreatic collection was identified. Patients were discharged to home on the 17th and 18th postoperative day, respectively. At the last follow-up, no recurrence was found. Both patients later developed diabetes mellitus and needed the support of supplementary pancreatic enzymes until the last follow-up.
We present our technique and our initial experience with the intraoperative embolization of Wirsung's duct with Onyx® in order to prevent pancreatic leakage.
Nowadays, a solution for POPF is the most important challenge for pancreatic surgeons. New classification,3 better understanding of risk factors (e.g. age, obesity, cardiovascular diseases, diabetes mellitus, pancreatic texture, and pancreatic duct size)171819 and technical advance220 are reported in the literature. Despite this, the risk of developing POPF remains high and is linked to lethal complications.45 Some authors have reported lower morbidity and death rates in a non-randomized trial using duct occlusion with synthetic glues after PD.710 However, as shown by Cheng et al.12 in a recent meta-analysis, which included nine trials involving 1095 participants who were randomized to the fibrin sealant group (N=550) and the control group (N=545) after pancreatic surgery, there was no evidence of differences in overall postoperative pancreatic fistula (fibrin sealant 29.6%, control 31.0%, p=0.58), postoperative deaths (3.1% versus 2.1%, p=0.53;), overall postoperative morbidity (29.6% versus 28.9%, p=0.77), reoperation rate (8.7% versus 10.7%, p=0.29), or length of hospital stay (12.9 days versus 13.1 days, p=0.331) between the groups. Therefore, based on the currently available evidence, fibrin sealants do not seem to prevent postoperative pancreatic fistula in people undergoing pancreatic surgery.912 We have tried to overcome these issues by using a new substance already widely used in other fields and a new technique that has never before used in this way.
The glues most frequently described in the literature and used for occlusion of the main pancreatic duct are Neoprene, Ethibloc, and Tissucol. Neoprene latex 671 (Dupont de Nemours) is a liquid synthetic rubber composed of polychloroprene homopolymer. When in contact with the pancreatic juice (pH 8 to 9), Neoprene polymerizes and hardens permanently. Ethibloc (Johnson & Johnson) is an alcoholic prolamine solution that hardens in 15 to 20 minutes in a moist environment; it disintegrates within 11 days. Tissucol (Immuno GmbH) is a modified fibrin glue solution, and in combination with thrombin (Trasylol) it will harden; it dissolves in about 7 days.8
Onyx® consists of an EVOH dissolved in various concentrations of dimethyl sulfoxide (DMSO). The viscosity of the mixture depends on the concentration of EVOH. Solutions with a higher concentration of EVOH are more viscous. When the mixture comes in contact with aqueous solutions, the DMSO diffuses away and EVOH precipitates. This precipitation starts at the interface while the core is still liquid. As pancreatic flow is substantially slower than that of blood and biliary flow, DMSO diffusion may be slower and EVOH remain liquid for a longer time. Two versions of Onyx® (18 and 34) are available with different concentrations of EVOH. We prefer to use the less-viscous version (18), with a lower concentration of EVOH (6%) in order to allow adequate progression of the embolizing material within the secondary pancreatic ducts. In fact, the Onyx® 34, with a high concentration of EVOH (8%,) is more viscous and would not ensure an adequate progression in the ducts. The physicochemical characteristics of Onyx® allow controlled application, forming a defined cast and permanent occlusion.
In addition to chemical differences from other substances, Onyx® has a substantial innovation in the application technique. All glues used until now were placed without a real objective feedback. In our technique, a wirsungography was performed prior to the Onyx®'s application, and the procedure was performed under direct fluoroscopic control.
The major limitations of a permanent occlusion of the main pancreatic duct are the consequent pancreatic atrophy and a complete loss of exocrine function.7
According to Tran et al.,8 no difference has been detected in terms of exocrine insufficiency between pancreatojejunostomy and pancreatic duct occlusion. Indeed, in their study, pancreatic enzyme substitution was, on discharge and at 3 months, significantly higher in patients with occlusion of the pancreatic duct (p=0.001 and p=0.003), but no difference was found at 12 months compared to patients with pancreatojejunostomy. In our experience, the two patients required enzyme supplementation support at the time of discharge to home and at the last follow-up.
About endocrine function, some authors suggest that occlusion of the main pancreatic duct would cause a parenchymal atrophy with a high risk of developing endocrine failure.21 Tran et al.8 reported a significantly higher incidence of endocrine insufficiency in the pancreatic duct occlusion group, with a diabetes rate of 34%. In our series, both patients had become diabetic at last examination.
In conclusion, we demonstrate that this approach is feasible and safe; studies with more patients are needed to verify the validity of this technique.
References
1. Zhang H, Zhu F, Shen M, Tian R, Shi CJ, Wang X, et al. Systematic review and meta-analysis comparing three techniques for pancreatic remnant closure following distal pancreatectomy. Br J Surg. 2015; 102:4–15. PMID: 25388952.

2. Xiong JJ, Tan CL, Szatmary P, Huang W, Ke NW, Hu WM, et al. Meta-analysis of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Br J Surg. 2014; 101:1196–1208. PMID: 25042895.

3. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017; 161:584–591. PMID: 28040257.
4. Gouma DJ, van Geenen RC, van Gulik TM, de Haan RJ, de Wit LT, Busch OR, et al. Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann Surg. 2000; 232:786–795. PMID: 11088073.

5. Vollmer CM Jr, Sanchez N, Gondek S, McAuliffe J, Kent TS, Christein JD, et al. A root-cause analysis of mortality following major pancreatectomy. J Gastrointest Surg. 2012; 16:89–102. discussion 102-103. PMID: 22065319.

6. Schulick RD, Yoshimura K. Stents, glue, etc.: is anything proven to help prevent pancreatic leaks/fistulae? J Gastrointest Surg. 2009; 13:1184–1186. PMID: 19399562.

7. Di Carlo V, Chiesa R, Pontiroli AE, Carlucci M, Staudacher C, Zerbi A, et al. Pancreatoduodenectomy with occlusion of the residual stump by Neoprene injection. World J Surg. 1989; 13:105–110. discussion 110-101. PMID: 2543144.

8. Tran K, Van Eijck C, Di Carlo V, Hop WC, Zerbi A, Balzano G, et al. Occlusion of the pancreatic duct versus pancreaticojejunostomy: a prospective randomized trial. Ann Surg. 2002; 236:422–428. discussion 428. PMID: 12368670.
9. Suc B, Msika S, Fingerhut A, Fourtanier G, Hay JM, Holmières F, et al. Temporary fibrin glue occlusion of the main pancreatic duct in the prevention of intra-abdominal complications after pancreatic resection: prospective randomized trial. Ann Surg. 2003; 237:57–65. PMID: 12496531.
10. Alfieri S, Quero G, Rosa F, Di Miceli D, Tortorelli AP, Doglietto GB. Indications and results of pancreatic stump duct occlusion after duodenopancreatectomy. Updates Surg. 2016; 68:287–293. PMID: 27631168.

11. Martin I, Au K. Does fibrin glue sealant decrease the rate of anastomotic leak after a pancreaticoduodenectomy? Results of a prospective randomized trial. HPB (Oxford). 2013; 15:561–566. PMID: 23458447.

12. Cheng Y, Ye M, Xiong X, Peng S, Wu HM, Cheng N, et al. Fibrin sealants for the prevention of postoperative pancreatic fistula following pancreatic surgery. Cochrane Database Syst Rev. 2016; 2:CD009621. PMID: 26876721.

13. Adamus Nürnberg R, Uder Erlangen M, Kleinschmidt T, Detmar K, Bolte R, Stein H, et al. Embolization of acute abdominal and thoracic hemorrhages with ethylene vinyl alcohol copolymer (onyx): initial experiences with arteries of the body trunk. Rofo. 2010; 182:900–904. PMID: 20725878.
14. Eberhardt KM, Treitl M, Sadeghi-Azandaryani M. An endovascular technique for treatment of high-risk iatrogenic aortic pseudoaneurysms with the ethylene vinyl alcohol copolymer onyx and aortic stent grafting. Rofo. 2012; 184:1163–1165. PMID: 23154857.

15. Kyokane T, Nagino M, Oda K, Nimura Y. An experimental study of selective intrahepatic biliary ablation with ethanol. J Surg Res. 2001; 96:188–196. PMID: 11266272.

16. Uller W, Müller-Wille R, Loss M, Hammer S, Schleder S, Goessmann H, et al. Percutaneous management of postoperative bile leaks with an ethylene vinyl alcohol copolymer (onyx). Rofo. 2013; 185:1182–1187. PMID: 23860801.

17. Gaujoux S, Cortes A, Couvelard A, Noullet S, Clavel L, Rebours V, et al. Fatty pancreas and increased body mass index are risk factors of pancreatic fistula after pancreaticoduodenectomy. Surgery. 2010; 148:15–23. PMID: 20138325.

18. Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM Jr. A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg. 2013; 216:1–14. PMID: 23122535.

19. Ramacciato G, Mercantini P, Petrucciani N, Nigri GR, Kazemi A, Muroni M, et al. Risk factors of pancreatic fistula after pancreaticoduodenectomy: a collective review. Am Surg. 2011; 77:257–269. PMID: 21375833.
20. Figueras J, Sabater L, Planellas P, Muñoz-Forner E, Lopez-Ben S, Falgueras L, et al. Randomized clinical trial of pancreaticogastrostomy versus pancreaticojejunostomy on the rate and severity of pancreatic fistula after pancreaticoduodenectomy. Br J Surg. 2013; 100:1597–1605. PMID: 24264781.

21. Okamoto A, Tsuruta K. Fistulation method: simple and safe pancreaticojejunostomy after pancreatoduodenectomy. Surgery. 2000; 127:433–438. PMID: 10776435.

Fig. 1
Intraoperative fluoroscopy: the procedure begins with the embolization of the distal part of the duct (A), continues to the body (B) and up to the stump (C). The final angiographic control shows the Wirsung mold, with evidence of all secondary pancreatic branches (D).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download