Abstract
Purpose
Long-term fixation of cemented acetabular components can be problematic in younger active patients. Our technique is put forward to improve outcomes and maximize implant survivorship in this particular patient population.
Materials and Methods
We report on a cohort of young adult patients (less than 55 years old) with cemented total hip replacement (THR) using a novel technique in preparing and cementing the acetabulum with a minimum follow-up of 10 years (mean follow-up, 14 years). Retrospectively collected data on clinical and radiological outcomes were reviewed.
Results
Sixty-five THRs were performed with the minimum study follow-up period. Average age for patients was 44 years old (range, 19–55 years). The mean Hip Disability and Osteoarthritis Outcome Score for patients at final appointment was 92.7. Radiographs taken at an average of 14 years after operation showed 63 of 65 hips showed no evidence of any radiological loosening. Cup survivorship was 100% at the end of the study period.
Cemented total hip arthroplasty (THA) is a globally successful intervention1). Long-term results for cemented implants has shown increased implant longevity and improved outcomes123). Long-term results have also demonstrated that the most widespread cause of failure is aseptic loosening45). While cemented polished tapered stem design in patients younger than 55 years old have had excellent results, cemented cup failure remained an issue6). Aseptic loosening occurs more frequently with acetabular components than with femoral components in cemented implants5789). Interdigitation at the bone-cement interface must be considered when evaluating the quality and longevity of cement fixation1011). Optimization of the acetabular bone surface preparation has been recognized as an important process of generating a solid bone-cement interface1213). The mechanism of action of this secure cementation technique is believed to prevent early fluid and debris penetration312). A wide spread method to achieve cemented acetabular fixation has been the introduction of reaming with retention of the subchondral bone plate (SCBP) for improved stability of fixation1415). However, retention of subchondral bone was not associated with the anticipated reduction in acetabular component loosening16). Work based on finite element analyses and stress distribution has favored acetabular bone decortication1718).
Cementless hip prosthesis is being used more widely over the last decade when compared to cemented implants. A major leading factor in the adoption of cementless fixation in younger and more active patient remained the reported long-term issues with cemented acetabular fixation in this cohort of patients1920). Concerns were raised in relation to bone loss and loss of stability in younger and more active patients. A recent report derived from the Nordic hip arthroplasty registry showed better long-term outcomes for uncemented implants in terms of revision for aseptic loosening20). In patients younger than 55 years, however, uncemented total hip replacement (THR) had higher short-term revision rates due to dislocation, periprosthetic fractures, and infection. It is therefore undeniable that uncemented cups in younger patients carry their own set of complications. Other authors have reported a high rate of revision due to problems occurring at the liner-metal shell couple21,22). Similar observations are echoed in reports from other national joint registries232425). Hence, questions prevail on whether uncemented acetabular components in primary THRs are the panacea for long-term survival in young and active patients.
Flivik et al.26) published ten years radiological and clinical outcomes of subchondral bone removal on cemented acetabular component fixation regardless of age. The authors randomized patients into removal or retention of the SCBP during THR. Removal of the SCBP was associated with greater implant stability and better cement-bone interface in the longer term.
We offer a variation in the technique and study on a younger patient population hence at a greater risk of acetabular component loosening. We hypothesize that our technique of subchondral decortication in cemented acetabular fixation in patients 55 years or younger improves outcomes and maximizes implant survivorship in this particular population. The aim of this study was therefore to assess the survivorship, clinical and radiological outcomes of cemented THR in younger and active patients and specifically whether our technique of acetabular preparation resulted in greater cup stability and better bone-cement interface in the long term.
The inclusion criteria were any patient 55 years old or under at the time of primary hip arthroplasty with at least 10 years of follow-up. The patients must have had radiographs 10 years post arthroplasty. All other patients were excluded. This study comprised a total of 53 non-selected consecutive patients who received 65 THRs. All the patients included were 55 years old or younger at the time of surgery. All operations were performed between the years 1999 and 2007, by the senior author. All patients were mobilized full weight bearing immediately post operation. Outcome measures reporting and analysis included all consecutive patients at the latest point in follow-up. The entire clinical series and subsequent follow-up were carried out in a single institution. Ethical approval was not required for this retrospective study.
The preoperative diagnosis was osteoarthritis in 52 hips (80.0%), hip dysplasia in 6 (9.2%), osteonecrosis in 5 (7.7%) and trauma in 2 (3.1%). Preoperatively all new patients were assessed clinically and radiographically by a senior orthopaedic surgeon.
The implants components implanted were the Elite Plus cemented cup (Depuy-Synthes, Warsaw, IN, USA) and Exeter stem (Stryker® Howmedica Osteonics, Mahwah, NJ, USA) in all hips. The ExeterTM femoral stem (V40TM) is a collarless double taper polished Orthinox® stainless steel (Stryker® Howmedica Osteonics), with a 125° neck-shaft angle, a 0.2-µm Ra polished surface finish and a 12/14 Eurocone Morse taper. Eleven Stem sizes are available in the central range with offsets of 35.5, 37.5, and 44 mm. All bearing surfaces were metal on polyethylene. A 28-mm-diameter modular head was used in 62 hips (95.4%). The Elite plus acetabular cup was first introduced in 1994 and has had a 10A orthopaedic data evaluation panel rating since 2008. The cups are manufactured from ultrahigh molecular weight polyethylene and gamma irradiated.
The acetabulum is first prepared by excision of osteophytic bone with a gouge osteotome (Fig. 1). Then reamers are used to get to the true floor of the acetabulum (Fig. 2). Following this multiple drill holes are made with a 6-mm drill (Fig. 3). Following this a gouge osteotome is used to excise the sclerotic subchondral bone acetabular bone (Fig. 4). Only the thinnest layer of sclerotic bone is removed to expose the healthy cancellous bone while preserving acetabular bone stock. This results in a fresh and highly irregular cancellous bed. The technique is repeated to achieve removal of the diseased subchondral bone plate. The resulting surface has a similar appearance to a porcupine back and provides an optimal micromechanical interlock with cementation. In essence the technique massively increases the surface area contact for the bone/cement interface and results in the entire acetabulum serving as a solid fixation pit. The final image of the acetabular preparation is seen in Fig. 5. It is important to try to preserve the peripheral rim of the true acetabulum after removal of exterior osteophytes. Direct pulse lavage washout is carried out and the bone bed is dried and further washed with hydrogen peroxide soaked gauze. Cement (Simplex P; Howmedica, Rutherford, NJ, USA) in the doughy stage is introduced by hand and pressurized into sequences prior to cup implantation. Post-operative radiographs demonstrating cement penetration and integration into the pelvis is demonstrated in Fig. 6.
Clinical outcomes were recorded on admission and during each follow-up when the patients are seen by the senior author or a member of his team. Standard anteroposterior radiographs of both hips were obtained at each follow-up and patients completed post-operative clinical outcome scores. Patients received a complete clinical examination and completed outcome scores at each scheduled visit. The primary outcome measure consisted of a modification of the Western Ontario McMaster (WOMAC) osteoarthritis index, the Hip Disability and Osteoarthritis Outcome Score (HOOS)2728). This is a short 36 question form which provides a validated and reliable measure of hip health for patients undergoing THR. It is specifically designed and validated for assessing physical function associated with younger populations for hip osteoarthritis. It has improved responsiveness compared to the WOMAC osteoarthritis score. The maximum possible and highest clinical score is 100, which suggests a very high level of function and satisfaction with the hip. The patients were also asked the following questions at each appointment:
Q1. How good is your hip at allowing you to perform routine every day activities such as housework, shopping, gardening and walking?
Q2. How good is your hip at enabling you to return to more vigorous activities such as tennis, trekking, running and gym workouts?
Q3. Overall how do you rate your satisfaction with the hip replacement?
Q4. Based on your experience of the hip replacement, would you recommend this operation to a friend with severe hip pain?
Secondary outcome measures consisted of radiographic evaluation of component loosening and migration. Radiological outcome was measured on anteroposterior radiographs of the pelvis specifically assessing the cup for loosening at the latest follow-up consultation. Assessments were performed by 2 authors (orthopaedic surgeon and radiologist), all abnormalities were reviewed by the senior author (TL) and final agreement was reached by consensus. Correction for magnification was performed by standardization of all measurements against the magnification of the measured size of the femoral head as compared with the known size. For the purpose of this study and pertinence to our clinical question only the acetabular components were evaluated for bone-prosthesis radiolucencies and osteolysis. This evaluation was carried-out in relation to the Charnley zones. Migration of the acetabular component was evaluated and component was considered to be loose radiographically if it had migrated >1 mm.
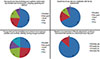
All the patients were accounted for and have therefore been included in the study. There were 65 hip replacements done with adequate follow-up who underwent subchondral bone decortication in the preparation of the acetabulum (Table 1). No cup components were revised in the study period. None of the hips were failing at their last follow-up, and all demonstrated expected subsidence of the cemented stem. One hip required revision of the femoral component due to a stem fracture. During revision of the stem, it was noted the cup was stable and well positioned and therefore it was retained. Clinical and radiological data in all of the hips was obtained with a mean follow-up of 14 years. The average HOOS for all patients was 92.7 points (95% confidence interval, 90.4 to 95.0). The responses to the 4 questions were overall very good with 56 out of 65 hips delighted with their hip at a mean of 14 years. All patients would recommend the operation. The responses to the questions can be seen in Fig. 7.
Sixty two of the 65 hips had no evidence of loosening in any of Charnley zones of the acetabulum. One patient had a radiographic lucent line occupying up to 30% of Zone 1. However this did not affect him at all clinically as his HOOS was 100. Another patient had a lucency occupying 40% of Zone 3, but once again his hip score was high (99.2) suggesting that this is not clinically loose. The final patient with radiographic loosening had cup migration of over 5 mm, 19 years after implantation of the cup for avascular necrosis. This had reached a stable point and the patient was very satisfied as he had a HOOS of 90.8. There are currently no plans to revise the implant.
Both cemented and cementless THA yield good long-term results. However, a review of comparative studies, long-term case series, prior literature reviews, meta-analysis, and national arthroplasty registry data demonstrates that cemented hip arthroplasty remains the gold standard in all age groups29). This was particularly true in the Scandinavian joint arthroplasty registries, when all cause revision rates are considered, cemented acetabular cups yield superior results when compared with cementless cups29). Yet cemented hip arthroplasty remains the operation of choice for the older patients. In the national joint registry annual report for England, Wales, and Northern Ireland, the median age for all cemented THA was 74 years compared to 65 years for uncemented THA30). The Kaplan-Meier cumulative percentage probability of revision at 10 years for cemented THA in patients younger than 55 years of age at primary operation was 6.54% for males and 5.85% for females. The same figures were significantly better for the older group at 55 to 64 years with 4.71% for males and 4.17% for females. Nevertheless, compared to the entire patient population, there is still paucity in long-term results of cemented THA in young and dysplastic hip patients.
Wroblewski et al.31) published results of 1,434 Charnley low-friction arthroplasties in patients younger than 50 years. At 15 years cemented cup survivorship in low polyethylene wear was 95.92% compared with 60.76% in high polyethylene wear cups. Results in favor of cemented fixation in younger patients are principally in relation to cemented tapered polished stem type of implant, with cementless cup fixation. In a series by Burston et al.6), 28% of the cemented cups and 15% of the uncemented cups required revision at 10 years follow-up. This study reported 19% overall revision rate for mechanical failure (aseptic loosening and liner wear) of all acetabular components in patients younger than 50 years compared with 7.5% in patients over 50 years of age. Similarly an earlier review of 105 hips with 10 to 12 years follow-up using secondgeneration cementing techniques, found a rate of aseptic loosening of 42%32). Late aseptic loosening was found to be mediated by a biologic reaction to small particles of highdensity polyethylene33). Optimizing micro-interlock between the bone-cement interface therefore appears to be central to long-term survivorship in cemented acetabular components.
Although more technically demanding, the method of subchondral bone removal described by the senior author results in better micromechanical interlock between the cement and the bone by increasing the surface area for the bone cement interface. The manual removal technique described above utilizing gouge osteotomes offers a more controlled approach to SCBP removal, as opposed to the risk of mechanical trauma and thermal damage, which might be encountered with the use of reamers only. This is echoed in the excellent patient reported outcomes and radiological evaluation observed in our analysis of cemented THA in patients 55 years and younger.
Flivik et al.26) published long-term results from a randomised study comparing clinical outcomes and radioisometric analysis in cemented THA with a mean age of 70 years. The authors showed increased proximal cup migration, cup inclination and the number of radiolucent lines in the subchondral bone retention group when compared to subchondral bone removal. These results were particularly significant at 6 and 10 years follow-up. Equally, despite the lack of significant difference in implant survivorship, the study demonstrated consistently better patient reported outcomes. The study by Flivik et al.26) also reiterated an important point demonstrated in our results and reported by several previous authors343536) which is presence of early radiolucent lines as an accurate predictor of long-term loosening in cemented acetabular component fixation. Such observations are in agreement with earlier results of late aseptic loosening from retrieval analysis33). Furthermore, finite element analysis support the mechanical properties associated with subchondral plate removal with better stiffness and stress distribution17). Hence, from both a biological and mechanical standpoint subchondral bone removal can be an important adjunct in acetabular preparation. Despite these observations, there has been paucity in the research looking at the impact of subchondral bone removal. Our study not only offers support to Flivik et al.'s26) work, but also shows excellent results in a group of patient at higher risk of aseptic loosening.
The authors recognize that the orthopaedic literature demonstrates a vast array of studies supporting alternatives to cemented hip arthroplasty. It is also undeniable that registry data even with limited time span show very good results with certain cementless designs and hybrid combinations. The success story enjoyed by cemented hip arthroplasty prevails and remains championed by data from various national registries. It is also the more tenable option from a cost-analysis standpoint given the current economic climate1,5). The results presented in our series demonstrate concordance with clinical outcomes from previous studies, and from biomechanical analyses on the modes of failure. In contrast to some of these studies we presented an explicit illustration of what is denoted by subchondral bone removal. While we still strongly advocate the basic principles of: bone preparation, cementation technique and correct orientation, our technique offers a way of optimizing acetabular component implantation.
The present study was a single surgeon and single institution longitudinal analysis of results. Although this methodology has inherent limitations in external validity, we have managed to transparently account for every case treated in the series. There were no hips lost to follow-up in the present study, a feature commonly encountered in longitudinal studies. One potential disadvantage particularly in younger groups of patients remains the loss of acetabular bone stock. However, using this technique makes acetabular component aseptic loosening very uncommon even in the high demand young patients. Nevertheless, loss of bone following any arthroplasty procedure remains a challenge if such hips were to be revised in the future.
The technique and results described in the study confirm the role of SCBP removal previously reported in small numbers within other studies. This is further supported by results in a cohort of patients at higher risk of early aseptic loosening of cemented acetabular component. Although technically challenging we conclude that this method merits serious consideration in order to improve long-term results of cemented THA in young and older patients.
Figures and Tables
Fig. 3
The subchondral bone is prepared with a 6-mm drill to begin to expose the bone under the subchondral sclerotic plate.

Fig. 4
The subchondral bone plate is further exposed by skimming the top layer of sclerotic bone off with the gouge osteotome.

Fig. 6
Post-operative radiographs of four patients having gone total hip replacement with subchondral bone decortication. (A) Sixteen years and (B, C) seventeen years after operaion.

Fig. 7
Pie charts showing responses to satisfaction questionnaires post hip replacement at the latest follow-up for each question (mean 14 years).
References
1. Clarke A, Pulikottil-Jacob R, Grove A, et al. Total hip replacement and surface replacement for the treatment of pain and disability resulting from end-stage arthritis of the hip (review of technology appraisal guidance 2 and 44): systematic review and economic evaluation. Health Technol Assess. 2015; 19:1–668. vii–viii.

2. Malchau H, Herberts P, Ahnfelt L. Prognosis of total hip replacement in Sweden. Follow-up of 9,675 operations performed 1978-1990. Acta Orthop Scand. 1993; 64:497–506.

3. Timperley AJ, Whitehouse SL, Hourigan PG. The influence of a suction device on fixation of a cemented cup using RSA. Clin Orthop Relat Res. 2009; 467:792–798.

4. Havelin LI, Fenstad AM, Salomonsson R, et al. The Nordic Arthroplasty Register Association: a unique collaboration between 3 national hip arthroplasty registries with 280, 201 THRs. Acta Orthop. 2009; 80:393–401.
5. Kynaston-Pearson F, Ashmore AM, Malak TT, et al. Primary hip replacement prostheses and their evidence base: systematic review of literature. BMJ. 2013; 347:f6956.

6. Burston BJ, Yates PJ, Hook S, Moulder E, Whitley E, Bannister GC. Cemented polished tapered stems in patients less than 50 years of age: a minimum 10-year follow-up. J Arthroplasty. 2010; 25:692–699.

7. Berry DJ, Harmsen WS, Cabanela ME, Morrey BF. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am. 2002; 84-A:171–177.
8. Callaghan JJ, Albright JC, Goetz DD, Olejniczak JP, Johnston RC. Charnley total hip arthroplasty with cement. Minimum twenty-five-year follow-up. J Bone Joint Surg Am. 2000; 82:487–497.
9. Ballard WT, Callaghan JJ, Sullivan PM, Johnston RC. The results of improved cementing techniques for total hip arthroplasty in patients less than fifty years old. A ten-year follow-up study. J Bone Joint Surg Am. 1994; 76:959–964.

10. Aspenberg P, Van der Vis H. Migration, particles, and fluid pressure. A discussion of causes of prosthetic loosening. Clin Orthop Relat Res. 1998; (352):75–80.
12. Flivik G, Sanfridsson J, Onnerfält R, Kesteris U, Ryd L. Migration of the acetabular component: effect of cement pressurization and significance of early radiolucency: a randomized 5-year study using radiostereometry. Acta Orthop. 2005; 76:159–168.

13. Majkowski RS, Bannister GC, Miles AW. The effect of bleeding on the cement-bone interface. An experimental study. Clin Orthop Relat Res. 1994; (299):293–297.
14. Carter DR, Vasu R, Harris WH. Periacetabular stress distributions after joint replacement with subchondral bone retention. Acta Orthop Scand. 1983; 54:29–35.

15. Vasu R, Carter DR, Harris WH. Stress distributions in the acetabular region--I. Before and after total joint replacement. J Biomech. 1982; 15:155–164.

16. Ritter MA, Thong AE. The role of cemented sockets in 2004: is there one? J Arthroplasty. 2004; 19:4 Suppl 1. 92–94.
17. Sutherland AG, D'Arcy S, Smart D, Ashcroft GP. Removal of the subchondral plate in acetabular preparation. Int Orthop. 2000; 24:19–22.

18. Crites BM, Berend ME, Ritter MA. Technical considerations of cemented acetabular components: a 30-year evaluation. Clin Orthop Relat Res. 2000; (381):114–119.
19. Mulroy WF, Harris WH. Acetabular and femoral fixation 15 years after cemented total hip surgery. Clin Orthop Relat Res. 1997; (337):118–128.

20. Pedersen AB, Mehnert F, Havelin LI, et al. Association between fixation technique and revision risk in total hip arthroplasty patients younger than 55 years of age. Results from the Nordic Arthroplasty Register Association. Osteoarthritis Cartilage. 2014; 22:659–667.

21. Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Uncemented total hip arthroplasty for primary osteoarthritis in young patients: a mid-to long-term follow-up study from the Finnish Arthroplasty Register. Acta Orthop. 2006; 77:57–70.

22. Mäkelä KT, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Results of 3,668 primary total hip replacements for primary osteoarthritis in patients under the age of 55 years: A follow-up of a previous report from the Finnish Arthroplasty Register. Acta Orthop. 2011; 82:521–529.

23. Jameson SS, Baker PN, Mason J, et al. The design of the acetabular component and size of the femoral head influence the risk of revision following 34 721 single-brand cemented hip replacements: a retrospective cohort study of medium-term data from a National Joint Registry. J Bone Joint Surg Br. 2012; 94:1611–1617.
24. Culliford DJ, Maskell J, Beard DJ, Murray DW, Price AJ, Arden NK. Temporal trends in hip and knee replacement in the United Kingdom: 1991 to 2006. J Bone Joint Surg Br. 2010; 92:130–135.
25. Streit MR, Weiss S, Andreas F, et al. 10-year results of the uncemented Allofit press-fit cup in young patients: 121 hips followed for 10-12 years. Acta Orthop. 2014; 85:368–374.

26. Flivik G, Kristiansson I, Ryd L. Positive effect of removal of subchondral bone plate for cemented acetabular component fixation in total hip arthroplasty: a randomised RSA study with ten-year follow-up. Bone Joint J. 2015; 97-B:35–44.
27. Nilsdotter A, Bremander A. Measures of hip function and symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopedic Surgeons (AAOS) Hip and Knee Questionnaire. Arthritis Care Res (Hoboken). 2011; 63:Suppl 11. S200–S207.
28. Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003; 4:10.

29. Clement ND, Biant LC, Breusch SJ. Total hip arthroplasty: to cement or not to cement the acetabular socket? A critical review of the literature. Arch Orthop Trauma Surg. 2012; 132:411–427.

30. National Joint Registry (NJR). 14th Annual Report of the NJR for England, Wales, Northern Ireland and the Isle of Man [Internet]. Hemel Hempstead, UK: NJR;2017. 2018 jul 1. Available from: http://www.njrcentre.org.uk/njrcentre/NewsandEvents/NJR14thAnnualReportrecordnumberofproceduresduring201617/tabid/1453/Default.aspx.
31. Wroblewski BM, Siney PD, Fleming PA. Wear of the cup in the Charnley LFA in the young patient. J Bone Joint Surg Br. 2004; 86:498–503.

32. Mulroy RD Jr, Harris WH. The effect of improved cementing techniques on component loosening in total hip replacement. An 11-year radiographic review. J Bone Joint Surg Br. 1990; 72:757–760.

33. Schmalzried TP, Kwong LM, Jasty M, et al. The mechanism of loosening of cemented acetabular components in total hip arthroplasty. Analysis of specimens retrieved at autopsy. Clin Orthop Relat Res. 1992; (274):60–78.
34. Hultmark P, Höstner J, Herberts P, Kärrholm J. Radiographic evaluation of Charnley cups used in first-time revision: repeated observations for 7-15 years. J Arthroplasty. 2003; 18:1005–1015.
35. Ritter MA, Zhou H, Keating CM, et al. Radiological factors influencing femoral and acetabular failure in cemented Charnley total hip arthroplasties. J Bone Joint Surg Br. 1999; 81:982–986.

36. García-Cimbrelo E, Diez-Vazquez V, Madero R, Munuera L. Progression of radiolucent lines adjacent to the acetabular component and factors influencing migration after Charnley low-friction total hip arthroplasty. J Bone Joint Surg Am. 1997; 79:1373–1380.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download