This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
Cephalomedullary nails (CMN) are commonly used for the surgical treatment of intertrochanteric fractures. This study aimed to evaluate overall postoperative local complications by reviewing patients who received surgical treatment using three different types of implants.
Materials and Methods
The study sample included 353 patients (107 males, 246 females) who underwent surgery using CMN for intertrochanteric fractures. Three different types of implants were used: i) the Gamma3® (Stryker) in 80 cases, ii) the Targon® PF (Aesculap) in 225 cases, and iii) the Compression Hip Nail® (Trademedics) in 48 cases. The mean age was 82.6 (range, 60–109) years and the average follow-up period was 15 (range, 6–80) months. Postoperative local complications and risk factors of cut-out were assessed.
Results
The most common complication was cut-out (n=26). Other complications included non-union (n=3), periprosthetic fracture (n=2), avascular necrosis (n=1), heterotopic ossification (n=1), and sleeve pull out (n=1). Multivariate analysis revealed that the cut-out group had a higher rate of poor reduction compared to the non-complicated group (P<0.001). Although the mean tip-apex distance (TAD) was 18.4 mm in the non-complicated group, lower than that of the cut-out group (P=0.001), multivariate analysis revealed that TAD was not a significant risk factor for cut-out (P=0.065).
Conclusion
Cut-out is the most common local complication associated with surgical treatment of intertrochanteric fractures using CMN. Proper reduction appears to be important in lowering the risk of cut-out. Maintaining low TAD is another critical factor in achieving sufficient fixation of lag screw to the subchondral bone of the femoral head.
Go to :

Keywords: Intertrochanteric fractures, Intramedullary nailing, Fracture reduction, Complications
INTRODUCTION
Controversy still surrounds the selection of implants for the surgical treatment of intertrochanteric fractures. In recent years, cephalomedullary nails (CMN) is increasingly being used
12). Biomechanical research has shown that CMN result in increased stability when compared with other extramedullary devices
3). Specifically, CMN are recommended for use in the fixation of unstable fractures
45).
To achieve favorable functional outcomes following the surgical management of intertrochanteric fractures, it is important to ensure that: i) the tip-apex distance (TAD) is less than 25 mm, and ii) the fracture is reduced anatomically
67). A variety of implants are used in the surgical management of intertrochanteric fractures, however, large-scale clinical studies have not been conducted to evaluate the comparative safety and effectiveness of different types of CMNs. Further studies with larger patient numbers are warranted to confirm overall outcomes following surgical intervention for the treatment of intertrochanteric fractures using a variety of implants.
The current study aimed to investigate postoperative local complications–specifically risk factors for cut-out–by reviewing medical records of patients who underwent surgery for the management of intertrochanteric fractures with three different types of CMNs and a minimum follow-up of 6 months.
Go to :

MATERIALS AND METHODS
This study was performed after gaining an approval from the institutional review board of our institution (KNUH-2018-04-005). We retrospectively reviewed 405 cases that underwent surgical management of intertrochanteric fractures using CMN by two orthopedic surgeons in our hospital from January 2010 to January 2017. Patients were excluded if they were less than 60 years old (n=15), died before fracture union (n=7) or followed up for less than 6 months (n=30); a total of 353 patients (107 males, 246 females) were thus included in our study. The implants used were the Gamma3® (Stryker, Schonkirchen, Germany; n=80), the Targon® PF (Aesculap, Tuttlingen, Germany; n=225), and the Compression Hip Nail® (Trademedics, Seongnam, Korea; n=48). Implants were not chosen according to the characteristics or facture types of patients and randomly selected at the time of surgery. The mean age at the time of surgery was 82.6 years (range, 60–109 years) and the average follow–up period was 15 months (range, 6–80 months).
Surgery was performed under general or spinal anesthesia. The patient was laid down on the fracture table and closed reduction was performed under fluoroscopic guidance by checking anteroposterior (AP) and translateral radiographs. The nail was inserted while reduction was maintained. In summary, a 5-cm skin incision was made proximal to the greater trochanter. A small hole was made using bone awl for nail insertion and the nail was placed in position by hand. The lag screw was inserted in the direction of the apex of the femoral head and then the distal locking screw was inserted.
Tolerable sitting and wheel chair ambulation were begun on the first postoperative day, and gradual weight bearing was allowed from the second postoperative day. Rehabilitation was flexibly applied depending on the patient's fracture stability, preoperative mobility and postoperative systemic condition.
Investigated variables included patient factors (i.e., age, sex, and AO/ASIF [Arbeitsgemeinschaft fur Osteosynthesefragen/Association for the Study of Internal Fixation] classification), and modifiable factors (i.e., implant type, TAD and reduction status). TAD was the sum of the distances from the tip of the lag screw to the apex of the femoral head as measured postoperatively on AP and translateral radiographs. The location of the lag screw tip was determined using the Cleveland index. Screw position in zones 5, 6, 8, and 9 having lower risk of complications and in zones 1, 2, 3, 4, and 7 were compared.
8) Reduction status was assessed using the criteria modified by Fogagnolo et al.
9) including alignment and displacement of main fragments.
Bone union was defined as the presence of bridging calluses formed in at least 3 cortices or no visible cortical or cancellous bone fracture lines visible on X-ray (AP or translateral views). Nonunion was defined as no fracture healing within 9 months of follow-up and persistent pain without progressive signs of healing at the fracture site for the latest three months.
Cut-out was defined as projection of the lag screw from the femoral head on AP or translateral view. Periprosthetic fracture, heterotopic ossification, and avascular necrosis were assessed using plain X-rays.
All statistical analyses were performed with SPSS ver. 24.0 (IBM Co., Armonk, NY, USA). The cut-out and non-complicated groups without cut-out and other complications were compared using chi-square and t-tests for categorical and continuous variables. Logistic regression analysis was performed to evaluate potential risk factors of cut-out. Multivariate analysis was done using variables with P-values less than 0.1 on univariate analysis. Differences were considered statistically significant at P<0.05.
Go to :

RESULTS
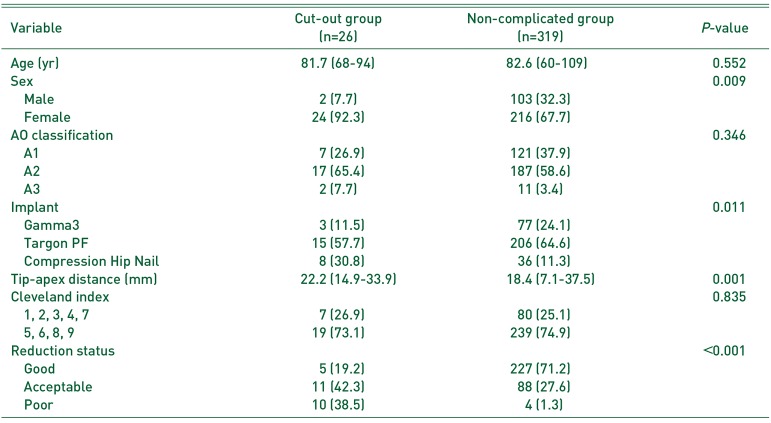
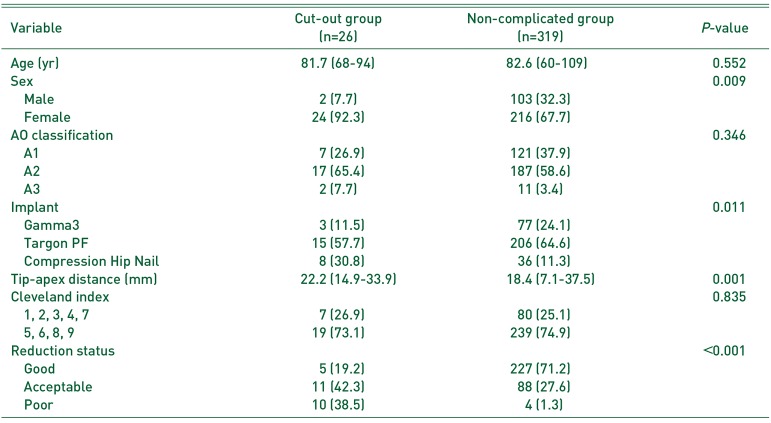
Cut-out occurred in 26 cases (7.4%). The mean onset of cut-out was 2.8 months (range, 0.5–8.0) after surgery (
Fig. 1). As shown in
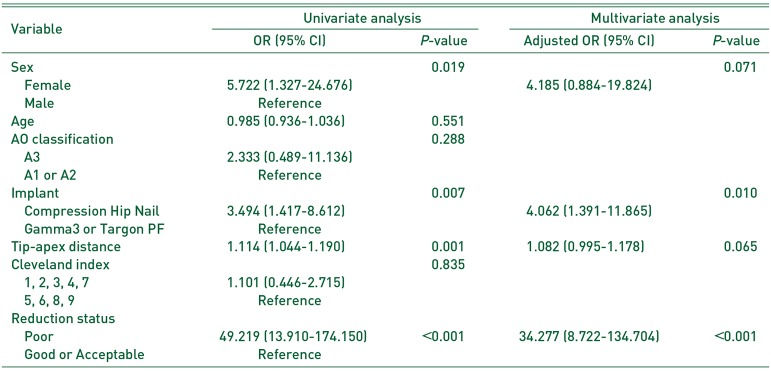
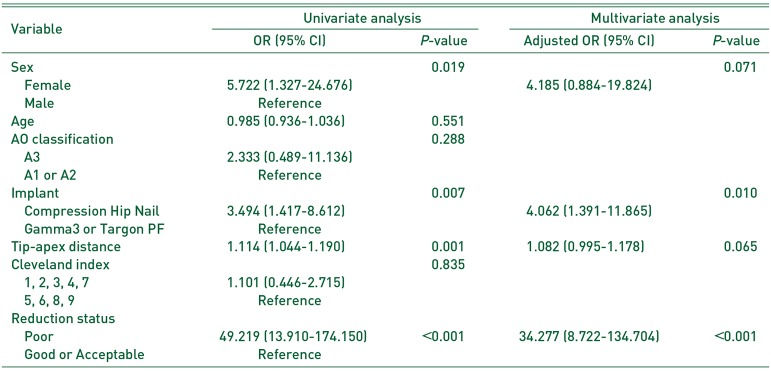
Table 1, significant differences between the cut-out and non-complicated included: i) sex, ii) TAD, iii) implant type, and iv) reduction status. Logistic regression analysis was performed to evaluate potential risk factors of cut-out; multivariate analysis revealed a significantly higher incidence rate of cut-out in patients with Compression Hip Nail or poor reduction (
Table 2). As shown in
Fig. 2, there were 8 additional cases of complications, including non-union (n=3), periprosthetic fracture (n=2), avascular necrosis (n=1), heterotopic ossification (n=1), and sleeve pull out (n=1).
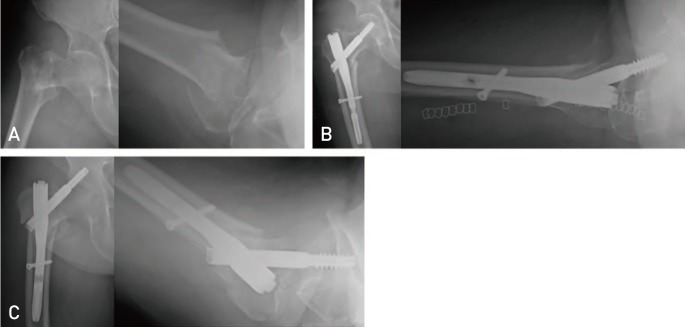
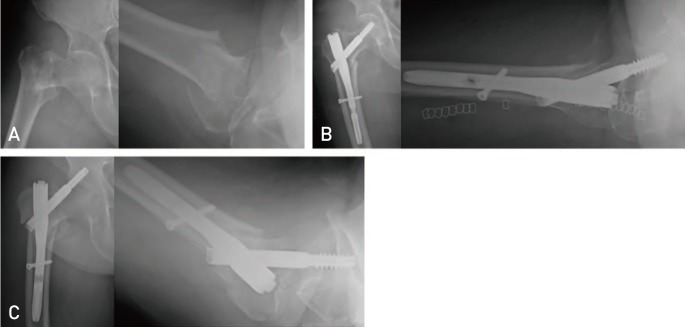 | Fig. 1A 78-year old female patient sustained an intertrochanteric fracture due to slip down (A). Although closed reduction and Compression Hip Nail fixation (Trademedics, Seongnam, Korea) was performed, it showed slight varus alignment with engagement of the proximal fragment into the shaft in immediate postoperative radiographs (B). One month later, the patient had progressive hip pain, and cut-out of lag screw with varus collapse was observed in radiographs (C).
|
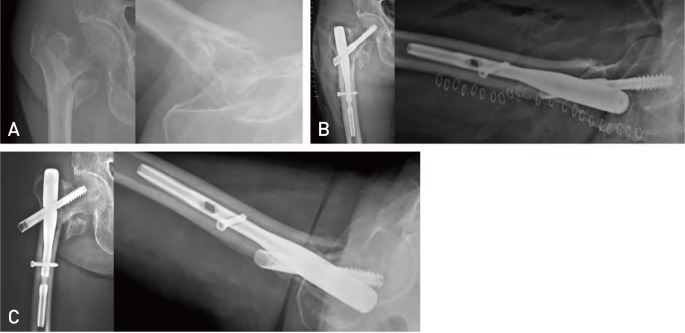
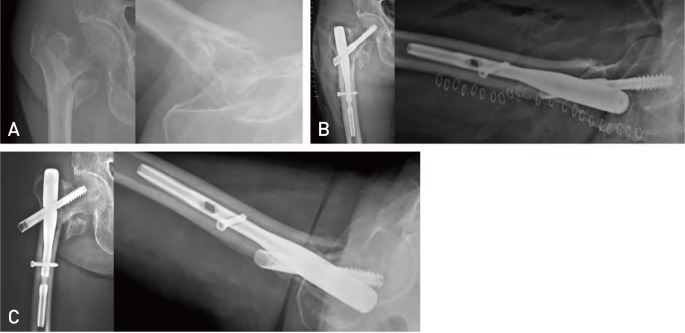 | Fig. 2A 87-year old female patient had closed reduction and internal fixation using Compression Hip Nail (Trademedics, Seongnam, Korea) for her right intertrochanteric fracture caused by slip down (A, B). At postoperative one month, a lag screw with sleeve was pulled out to the lateral side (C).
|
Table 1
Comparison between cut-out group and non-complicated group
|
Variable |
Cut-out group (n=26) |
Non-complicated group (n=319) |
P-value |
|
Age (yr) |
81.7 (68–94) |
82.6 (60–109) |
0.552 |
|
Sex |
|
|
0.009 |
|
Male |
2 (7.7) |
103 (32.3) |
|
|
Female |
24 (92.3) |
216 (67.7) |
|
|
AO classification |
|
|
0.346 |
|
A1 |
7 (26.9) |
121 (37.9) |
|
|
A2 |
17 (65.4) |
187 (58.6) |
|
|
A3 |
2 (7.7) |
11 (3.4) |
|
|
Implant |
|
|
0.011 |
|
Gamma3 |
3 (11.5) |
77 (24.1) |
|
|
Targon PF |
15 (57.7) |
206 (64.6) |
|
|
Compression Hip Nail |
8 (30.8) |
36 (11.3) |
|
|
Tip-apex distance (mm) |
22.2 (14.9–33.9) |
18.4 (7.1–37.5) |
0.001 |
|
Cleveland index |
|
|
0.835 |
|
1, 2, 3, 4, 7 |
7 (26.9) |
80 (25.1) |
|
|
5, 6, 8, 9 |
19 (73.1) |
239 (74.9) |
|
|
Reduction status |
|
|
<0.001 |
|
Good |
5 (19.2) |
227 (71.2) |
|
|
Acceptable |
11 (42.3) |
88 (27.6) |
|
|
Poor |
10 (38.5) |
4 (1.3) |
|

Table 2
Logistic regression analysis for evaluating risk factors of cut-out
|
Variable |
Univariate analysis |
Multivariate analysis |
|
OR (95% CI) |
P-value |
Adjusted OR (95% CI) |
P-value |
|
Sex |
|
0.019 |
|
0.071 |
|
Female |
5.722 (1.327–24.676) |
4.185 (0.884–19.824) |
|
Male |
Reference |
|
|
Age |
0.985 (0.936–1.036) |
0.551 |
|
|
|
AO classification |
|
0.288 |
|
|
|
A3 |
2.333 (0.489–11.136) |
|
|
A1 or A2 |
Reference |
|
|
Implant |
|
0.007 |
|
0.010 |
|
Compression Hip Nail |
3.494 (1.417–8.612) |
4.062 (1.391–11.865) |
|
Gamma3 or Targon PF |
Reference |
|
|
Tip-apex distance |
1.114 (1.044–1.190) |
0.001 |
1.082 (0.995–1.178) |
0.065 |
|
Cleveland index |
|
0.835 |
|
|
|
1, 2, 3, 4, 7 |
1.101 (0.446–2.715) |
|
|
5, 6, 8, 9 |
Reference |
|
|
Reduction status |
|
|
|
|
|
Poor |
49.219 (13.910–174.150) |
<0.001 |
34.277 (8.722–134.704) |
<0.001 |
|
Good or Acceptable |
Reference |
|
|
|

Complications occurred in a total of 34 patients (9.6%), and of these, 29 underwent additional surgery. Bipolar hemiarthroplasty was performed in 12 of 26 cases with cut-out, and total hip arthroplasty was done in 9. Of the five patients treated with Targon PF nails who experienced cut-out of anti-rotation pin, two had the anti-rotation pin removed; the remaining three did not undergo any additional surgical procedures. Considering their systemic condition and function, no surgical procedures were performed in two patients who were bed-ridden due to dementia and hemiplegia caused by cerebral infarction; a patient with mild symptoms and no functional problems was put under follow-up observation. Open reduction and internal fixation were performed in two cases with periprosthetic fracture. Two of three patients with non-union received bipolar hemiarthroplasty and total hip arthroplasty; the other patient was asymptomatic and put under follow-up observation. Total hip arthroplasty was conducted for one patient who presented with avascular necrosis, and bipolar hemiarthroplasty was performed in another patient experiencing sleeve pull out. A patient with asymptomatic heterotopic ossification was put under follow-up observation.
Go to :

DISCUSSION
Various types of CMNs are used for the management of proximal femoral fractures. Of these, the present study reviewed three different types of nails (i.e., Gamma3, Targon PF, and Compression Hip Nail). The Gamma 3 nail can control rotation by the set screw and U-blade with a lag screw and this is intended for biomechanically stable fixation
1011). The Targon PF nail is threaded in the support sleeve of the lag screw and can prevent the lateral protrusion of the implant; an additional anti-rotation pin helps prevent rotation of the fragments and this nail has been proven safe and effective in clinical trials
1213). The Compression Hip Nail is characterized by a sliding lag screw that can be controlled by the end caps of static or dynamic mode and helps relieve lateral hip pain with controlled telescoping
14). This study was meaningful in that it evaluated complications more comprehensively in a larger number of patients managed with different implant types compared to small-scale studies involving a single implant.
Baumgaertner et al.
6) described the TAD measurement as the sum of the distance from the tip of the lag screw to the femoral head apex on AP and lateral radiographs when performing sliding hip-screw fixation for peritrochanteric fractures; this group has suggested that a longer TAD increases the risk of cut-out. It has also been suggested that TAD is an important predictor of cut-out risk when using CMN, and that maintaining TAD less than 25 mm is critical in preventing cut-out
15). In this study, although TAD was kept less than 25 mm in most patients and the mean TAD was shorter (18.4 mm) in the non-complicated group compared with the complicated group (22.2 mm), multivariate analysis revealed that TAD was not a significant risk factor for cut-out. However, since the mean TAD of 22.2 mm can be interpreted as appropriate TAD in the cut-out group and only a small difference between the two groups was observed, there is a possibility that TAD is not a statistically significant risk factor for cut-out in multivariate analysis. This outcome needs to be interpreted within the context of findings of previous studies. A shorter TAD should be emphasized for lag screw fixation to the subchondral bone of osteoporotic femoral head.
Anatomical reduction is important in achieving a successful outcome after surgical treatment of intertrochanteric fractures
7). In unstable fractures, the anterior and medial cortical contact is crucial because it is more difficult to obtain contact with the posteromedial cortex
16). Fogagnolo et al.
9) assessed reduction as a criterion for determining alignment and displacement of main fragments, and reduction states were classified into “good”, “acceptable”, and “poor” by evaluating alignment and displacement of main fragments. Alignment was evaluated by assessing whether: i) there was normal cervico-diaphyseal angle or slight valgus on the AP view, and ii) it was less than 20° of angulation on the lateral view or not. Displacement of main fragments was evaluated whether more than 80% overlapping in both planes and less than 5 mm of shortening or not. “Good” reduction required both criteria above being met; reduction was considered “acceptable” if either the alignment or the displacement requirements above were met; and reduction was considered “poor” if neither of the criteria above were met. This study used the classification criteria of Fogagnolo et al.
9) for assessment of reduction status. A significant difference was shown in reduction status between the cut-out and non-complicated groups. Multivariate analysis revealed that “poor” reduction status was a significant risk factor of cut-out.
The Compression Hip Nail resulted in a significantly higher rate of cut-out when compared with other nails, and was identified as a risk factor for cut-out in multivariate analysis. A more cautious interpretation of results is warranted. Choo et al.
14) reported favorable outcomes of a controlled telescoping system for lateral hip pain relief in their study using Compression Hip Nail. Yi et al.
17) reported a higher complication rate of Compression Hip Nail in cases using 10 mm sliding lag screw. However, long-term observational studies are insufficient to comprehensively assess cut-out and other postoperative complications after surgery using Compression Hip Nail. Since this study involved a relatively small number of patients treated with the Compression Hip Nail and there may have been a selection bias relating to: i) the implant used, ii) surgeon's surgical techniques, and iii) implant factors, additional studies are warranted in the future.
There are some limitations in this study. Although no specific indications were specified relating to implant selection, selection bias is possible, selection bias is possible due to the retrospective nature of the study and complete randomization cannot be assured. This study was limited in exploring the relationship of osteoporosis and sarcopenia with postoperative outcomes because osteoporosis and sarcopenia were not thoroughly examined. A review of osteoporosis and sarcopenia-related data will allow for better overall analysis of surgical results.
Go to :

CONCLUSION
Cut-out is the most common complication resulting from surgical treatment of intertrochanteric fractures using CMN. Proper reduction is anticipated to be important in lowering the risk of cut-out. Maintaining appropriately small TAD is important in achieving sufficient fixation of the lag screw to the subchondral bone of the femoral head.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download