1. Ulrich SD, Seyler TM, Bennett D, et al. Total hip arthroplasties: what are the reasons for revision. Int Orthop. 2008; 32:597–604. PMID:
17443324.

2. Oleske DM, Bonafede MM, Jick S, Ji M, Hall JA. Electronic health databases for epidemiological research on joint replacements: considerations when making cross-national comparisons. Ann Epidemiol. 2014; 24:660–665. PMID:
25088754.

3. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007; 89:780–785. PMID:
17403800.

4. Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004; 351:1645–1654. PMID:
15483283.

5. Achermann Y, Vogt M, Spormann C, et al. Characteristics and outcome of 27 elbow periprosthetic joint infections: results from a 14-year cohort study of 358 elbow prostheses. Clin Microbiol Infect. 2011; 17:432–438. PMID:
20412190.

6. Alp E, Cevahir F, Ersoy S, Guney A. Incidence and economic burden of prosthetic joint infections in a university hospital: A report from a middle-income country. J Infect Public Health. 2016; 9:494–498. PMID:
26829894.

7. Haenle M, Skripitz C, Mittelmeier W, Skripitz R. Economic impact of infected total knee arthroplasty. Scientific World Journal. 2012; 2012:196515. PMID:
22619626.

8. Aggarwal VK, Bakhshi H, Ecker NU, Parvizi J, Gehrke T, Kendoff D. Organism profile in periprosthetic joint infection: pathogens differ at two arthroplasty infection referral centers in Europe and in the United States. J Knee Surg. 2014; 27:399–406. PMID:
24414388.

9. Piper KE, Jacobson MJ, Cofield RH, et al. Microbiologic diagnosis of prosthetic shoulder infection by use of implant sonication. J Clin Microbiol. 2009; 47:1878–1884. PMID:
19261785.

10. Gbejuade HO, Lovering AM, Webb JC. The role of microbial biofilms in prosthetic joint infections. Acta Orthop. 2015; 86:147–158. PMID:
25238433.

11. Corvec S, Portillo ME, Pasticci BM, Borens O, Trampuz A. Epidemiology and new developments in the diagnosis of prosthetic joint infection. Int J Artif Organs. 2012; 35:923–934. PMID:
23138706.

12. Trampuz A, Steckelberg J. Advances in the laboratory diagnosis of prosthetic joint infection. Expert Opin Med Diagn. 2003; 14:1–14.

13. Osmon DR, Berbari EF, Berendt AR, et al. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013; 56:e1–e25. PMID:
23223583.
14. Parvizi J, Gehrke T, Chen AF. Proceedings of the international consensus on periprosthetic joint infection. Bone Joint J. 2013; 95-B:1450–1452. PMID:
24151261.

15. Ochsner PE, Borens O, Bodler PM. Infections of the musculoskeletal system: basic principles, prevention, diagnosis and treatment. Grandvaux: Swiss orthopaedics in-house-publisher;2014.
16. Renz N, Yermak K, Perka C, Trampuz A. Alpha defensin lateral flow test for diagnosis of periprosthetic joint infection: not a screening but a confirmatory test. J Bone Joint Surg Am. 2018; 100:742–750. PMID:
29715222.
17. Ahmad SS, Becker R, Chen AF, Kohl S. EKA survey: diagnosis of prosthetic knee joint infection. Knee Surg Sports Traumatol Arthrosc. 2016; 24:3050–3055. PMID:
27637855.

18. Pérez-Prieto D, Portillo ME, Puig-Verdie L, et al. C-reactive protein may misdiagnose prosthetic joint infections, particularly chronic and low-grade infections. Int Orthop. 2017; 41:1315–1319. PMID:
28321490.

19. Piper KE, Fernandez-Sampedro M, Steckelberg KE, et al. Creactive protein, erythrocyte sedimentation rate and orthopedic implant infection. PLoS One. 2010; 5:e9358. PMID:
20179760.

20. Austin MS, Ghanem E, Joshi A, Lindsay A, Parvizi J. A simple, cost-effective screening protocol to rule out periprosthetic infection. J Arthroplasty. 2008; 23:65–68. PMID:
18165031.

21. Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev. 2014; 27:302–345. PMID:
24696437.

22. Trampuz A, Hanssen AD, Osmon DR, Mandrekar J, Steckelberg JM, Patel R. Synovial fluid leukocyte count and differential for the diagnosis of prosthetic knee infection. Am J Med. 2004; 117:556–562. PMID:
15465503.

23. Morgenstern C, Cabric S, Perka C, Trampuz A, Renz N. Synovial fluid multiplex PCR is superior to culture for detection of lowvirulent pathogens causing periprosthetic joint infection. Diagn Microbiol Infect Dis. 2018; 90:115–119. PMID:
29191466.

24. Schinsky MF, Della Valle CJ, Sporer SM, Paprosky WG. Perioperative testing for joint infection in patients undergoing revision total hip arthroplasty. J Bone Joint Surg Am. 2008; 90:1869–1875. PMID:
18762646.

25. Müller M, Morawietz L, Hasart O, Strube P, Perka C, Tohtz S. Diagnosis of periprosthetic infection following total hip arthroplasty--evaluation of the diagnostic values of preand intraoperative parameters and the associated strategy to preoperatively select patients with a high probability of joint infection. J Orthop Surg Res. 2008; 3:31. PMID:
18644107.

26. Krenn VT, Liebisch M, Kölbel B, et al. CD15 focus score: Infection diagnosis and stratification into low-virulence and high-virulence microbial pathogens in periprosthetic joint infection. Pathol Res Pract. 2017; 213:541–547. PMID:
28343870.

27. Trampuz A, Piper KE, Jacobson MJ, et al. Sonication of removed hip and knee prostheses for diagnosis of infection. N Engl J Med. 2007; 357:654–663. PMID:
17699815.

28. Spangehl MJ, Masri BA, O'Connell JX, Duncan CP. Prospective analysis of preoperative and intraoperative investigations for the diagnosis of infection at the sites of two hundred and two revision total hip arthroplasties. J Bone Joint Surg Am. 1999; 81:672–683. PMID:
10360695.

29. Portillo ME, Salvadó M, Trampuz A, et al. Improved diagnosis of orthopedic implant-associated infection by inoculation of sonication fluid into blood culture bottles. J Clin Microbiol. 2015; 53:1622–1627. PMID:
25740775.

30. Janz V, Trampuz A, Perka CF, Wassilew GI. Reduced culture time and improved isolation rate through culture of sonicate fluid in blood culture bottles. Technol Health Care. 2017; 25:635–640. PMID:
28436397.

31. Tigges S, Stiles RG, Roberson JR. Appearance of septic hip prostheses on plain radiographs. AJR Am J Roentgenol. 1994; 163:377–380. PMID:
8037035.

32. Kwee TC, Basu S, Torigian DA, Zhuang H, Alavi A. FDG PET imaging for diagnosing prosthetic joint infection: discussing the facts, rectifying the unsupported claims and call for evidence-based and scientific approach. Eur J Nucl Med Mol Imaging. 2013; 40:464–466. PMID:
23296643.

33. Kwee TC, Kwee RM, Alavi A. FDG-PET for diagnosing prosthetic joint infection: systematic review and metaanalysis. Eur J Nucl Med Mol Imaging. 2008; 35:2122–2132. PMID:
18704405.

34. Portillo ME, Salvadó M, Sorli L, et al. Multiplex PCR of sonication fluid accurately differentiates between prosthetic joint infection and aseptic failure. J Infect. 2012; 65:541–548. PMID:
22960370.

35. Qu X, Zhai Z, Li H, et al. PCR-based diagnosis of prosthetic joint infection. J Clin Microbiol. 2013; 51:2742–2746. PMID:
23740731.
36. Bonanzinga T, Zahar A, Dütsch M, Lausmann C, Kendoff D, Gehrke T. How reliable is the alpha-defensin immunoassay test for diagnosing periprosthetic joint infection? A prospective study. Clin Orthop Relat Res. 2017; 475:408–415. PMID:
27343056.

37. Sigmund IK, Holinka J, Gamper J, et al. Qualitativeα-defensin test (Synovasure) for the diagnosis of periprosthetic infection in revision total joint arthroplasty. Bone Joint J. 2017; 99-B:66–72. PMID:
28053259.
38. Deirmengian C, Kardos K, Kilmartin P, et al. The alpha-defensin test for periprosthetic joint infection outperforms the leukocyte esterase test strip. Clin Orthop Relat Res. 2015; 473:198–203. PMID:
24942960.

39. Borens O, Yusuf E, Steinrücken J, Trampuz A. Accurate and early diagnosis of orthopedic device-related infection by microbial heat production and sonication. J Orthop Res. 2013; 31:1700–1703. PMID:
23813873.

40. Giulieri SG, Graber P, Ochsner PE, Zimmerli W. Management of infection associated with total hip arthroplasty according to a treatment algorithm. Infection. 2004; 32:222–228. PMID:
15293078.

41. Deirmengian C, Greenbaum J, Lotke PA, Booth RE Jr, Lonner JH. Limited success with open debridement and retention of components in the treatment of acute Staphylococcus aureus infections after total knee arthroplasty. J Arthroplasty. 2003; 18(7 Suppl 1):22–26. PMID:
14560406.

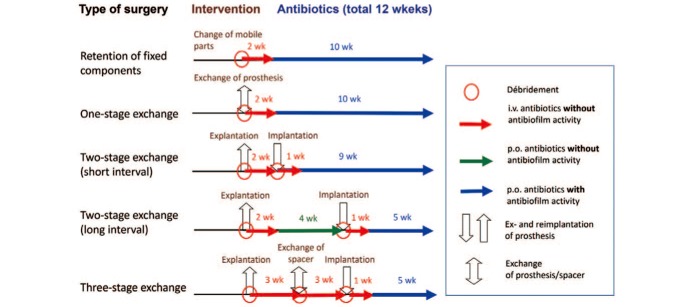
42. Trampuz A, Zimmerli W. Prosthetic joint infections: update in diagnosis and treatment. Swiss Med Wkly. 2005; 135:243–251. PMID:
15965826.
43. Tschudin-Sutter S, Frei R, Dangel M, et al. Validation of a treatment algorithm for orthopaedic implant-related infections with device-retention-results from a prospective observational cohort study. Clin Microbiol Infect. 2016; 22:457. PMID:
26806134.

44. Ilchmann T, Zimmerli W, Ochsner PE, et al. One-stage revision of infected hip arthroplasty: outcome of 39 consecutive hips. Int Orthop. 2016; 40:913–918. PMID:
26224611.

45. Zahar A, Webb J, Gehrke T, Kendoff D. One-stage exchange for prosthetic joint infection of the hip. Hip Int. 2015; 25:301–307. PMID:
26109160.

46. Kunutsor SK, Whitehouse MR, Blom AW, Beswick AD. Reinfection outcomes following one- and two-stage surgical revision of infected hip prosthesis: a systematic review and meta-analysis. PLoS One. 2015; 10:e0139166. PMID:
26407003.

47. Cha MS, Cho SH, Kim DH, et al. Two-stage total knee arthroplasty for prosthetic joint infection. Knee Surg Relat Res. 2015; 27:82–89. PMID:
26060606.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download