INTRODUCTION
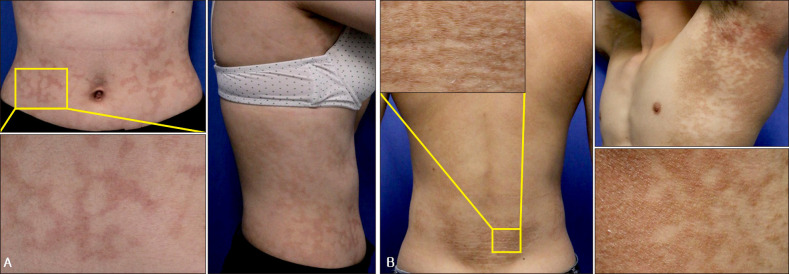
Confluent and reticulated papillomatosis (CRP) is an uncommon progressive and distinctive dermatosis characterized by persistent brown, scaly macules, papules, patches, and plaques. It was first described in 1927 by Gougerot and Carteaud as “papillomatoses pigmentée innominée”; later, they renamed it “papillomatoses pigmentée confluente et réticulée”
1. It was subsequently categorized as a new form of cutaneous papillomatosis, and its diagnostic criteria were established. Wise and Sachs
2 described the first case in the United States in 1937 and called it confluent and reticular papillomatosis. CRP is a rare dermatosis of an uncertain etiology that typically affects young adults, especially in the middle of the chest and back. It may simulate pigmented tinea versicolor, acanthosis nigricans (AN), or epidermal nevus
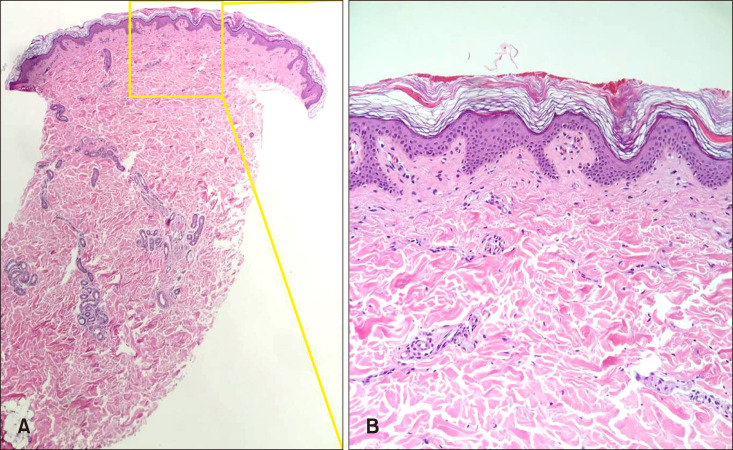
3. The histopathology of CRP involves orthohyperkeratosis, papillomatosis, minimal to mild acanthosis, and usually no significant inflammatory infiltrate. Although it has a chronic course, spontaneous resolution with subsequent recurrence can also occur
4. The aims of this study were as follows. First, because CRP is known to occur predominantly in teenage patients
5, it is necessary to clarify the histopathologic differences between teenage and adult patients. Second, studies on CRP in Asia, especially in Korea, are lacking. Based on the results of this study, differences between age groups can be identified, and information on Korean patients with CRP can be provided.
Go to :

DISCUSSION
The frequency of CRP internationally is unknown, and CRP is considered rare and is known to occur predominantly in young adults. In one study on 10 Lebanese cases
2, half were of each sex, and the mean age at diagnosis was 19 years. In this study, the mean age was 19.3 years, which is similar to those of previous studies. CRP is not only rare but also poorly recognized by physicians, including dermatologists. Since Gougerot and Carteaud
1 first identified CRP in 1927, this disease has been diagnosed on the basis of clinical courses, histologic findings, and treatment results. However, there have been misdiagnoses of CRP owing to a lack of diagnostic criteria for CRP. In a study on 39 patients, Davis et al.
5 proposed the following criteria for the diagnosis of CRP (Gougerot–Carteaud syndrome): (i) clinical findings, including brown, scaly macules and patches, at least parts of which appear reticulated and papillomatous; (ii) involvement of the upper trunk and neck; (iii) negative fungal staining of the scales; (iv) no response to antifungal treatment; and (v) excellent response to minocycline. However, a few cases of CRP without trunk involvement have been described in the literature. The reported skin lesions were located in the popliteal fossa
6, axilla
67, or antecubital regions
8. Those cases of CRP involved various flexural areas alone and fulfilled other diagnostic criteria for CRP. Jo et al.
9 suggested the addition of revised diagnostic criteria to include flexural area involvement into the previous criteria
5, which were limited to trunk and neck involvements.
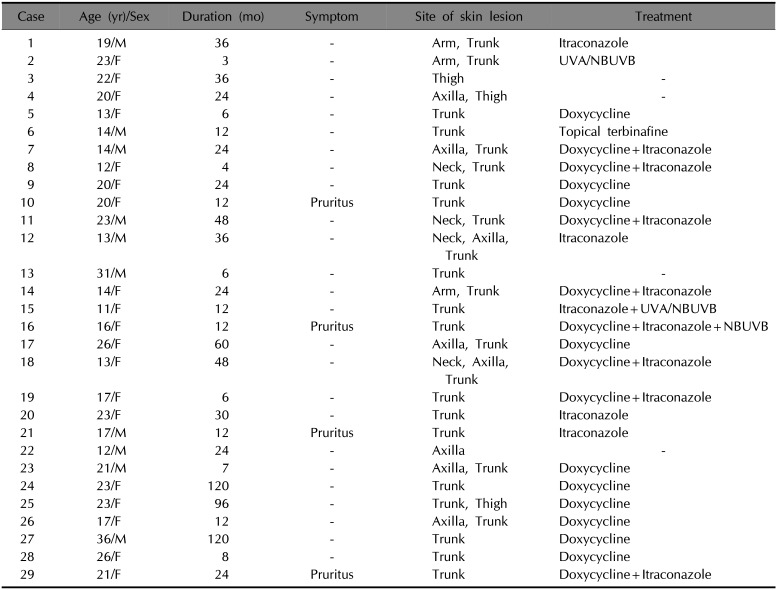
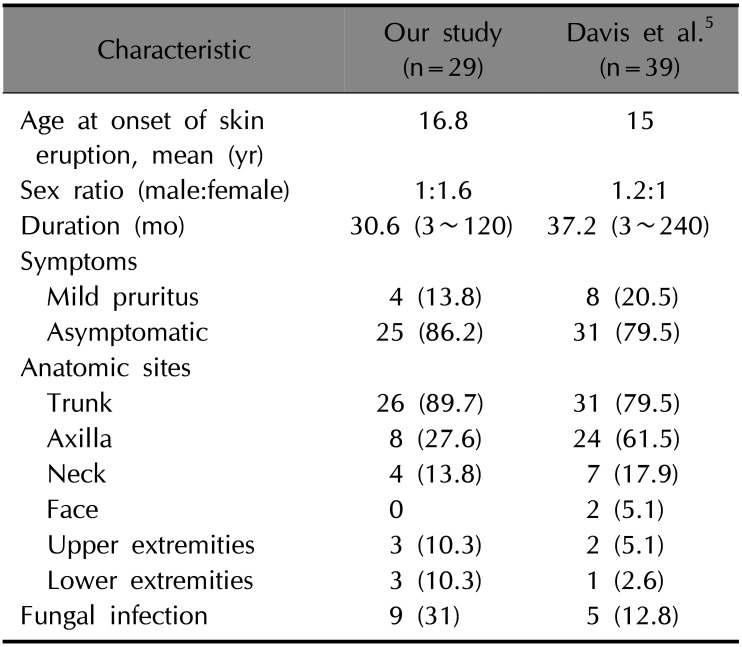
In this study, two patients had a single lesion sparing the trunk: one in the axilla and one on the thigh (
Table 1). Most of the patients had trunk lesions (89.7%), followed by axilla (27.6%) and neck (13.8%) lesions.
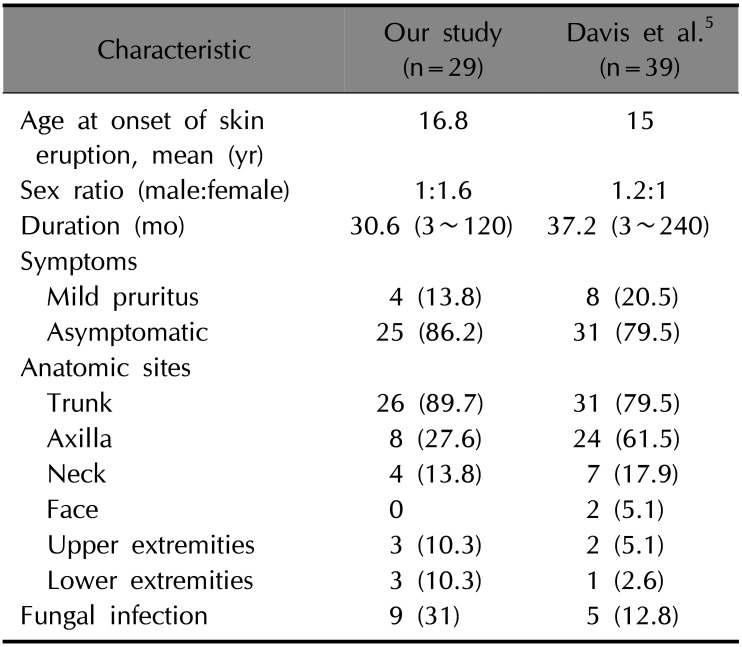
Table 4 shows the clinical characteristics of the patients in this study in comparison with those in a previous study
5. The demographics of the patients in the present study were in line with those in previous reports: CRP affects young adults. This disorder is thought to have no particular sex predilection; however, our study showed that the proportion of female patients was somewhat higher. It is uncertain whether this finding reflects its actual prevalence. Since CRP is almost asymptomatic, patients may visit the hospital seeking cosmetic improvement rather than symptom control. It also explains why the proportion of affected women was higher than that of men. Flexural area involvement, especially axillary lesions, was found in a larger number of patients in a previous study than in this study.
Table 4
Clinical characteristics compared with the previous study
|
Characteristic |
Our study (n=29) |
Davis et al.5 (n=39) |
|
Age at onset of skin eruption, mean (yr) |
16.8 |
15 |
|
Sex ratio (male:female) |
1:1.6 |
1.2:1 |
|
Duration (mo) |
30.6 (3~120) |
37.2 (3~240) |
|
Symptoms |
|
|
|
Mild pruritus |
4 (13.8) |
8 (20.5) |
|
Asymptomatic |
25 (86.2) |
31 (79.5) |
|
Anatomic sites |
|
|
|
Trunk |
26 (89.7) |
31 (79.5) |
|
Axilla |
8 (27.6) |
24 (61.5) |
|
Neck |
4 (13.8) |
7 (17.9) |
|
Face |
0 |
2 (5.1) |
|
Upper extremities |
3 (10.3) |
2 (5.1) |
|
Lower extremities |
3 (10.3) |
1 (2.6) |
|
Fungal infection |
9 (31) |
5 (12.8) |

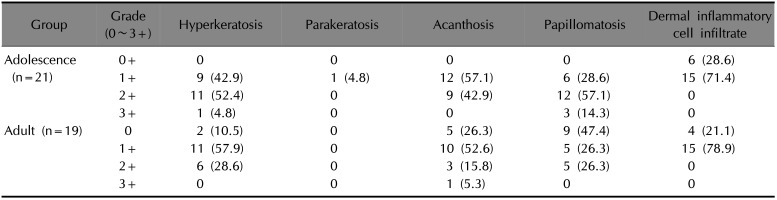
The histologic features in this study were similar to those reported in a previous study
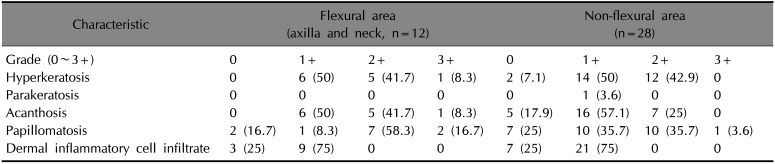
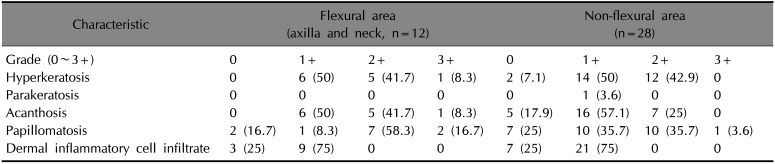
10. We found that the histologic changes were not associated with the disease duration. However, there were specific histologic changes in all patients by anatomic site.
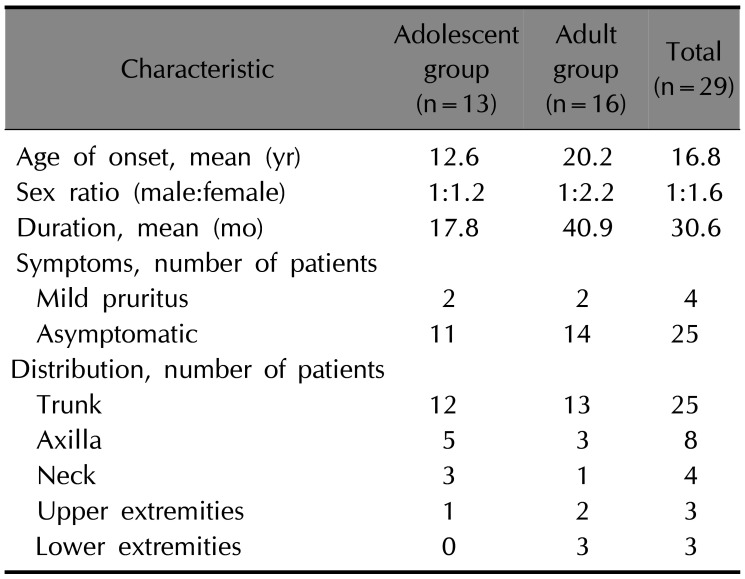
Table 5 shows the histologic features of the flexural (axilla and neck) and non-flexural areas. In the flexural area, half had high-grade (moderate to severe) hyperkeratosis, while most showed high-grade papillomatosis (75%); relatively mild hyperkeratosis and parakeratosis were seen in the non-flexural area. The acanthosis grades were similar, and it was confirmed that the flexural area had a more pronounced epidermal change than the non-flexural area. These findings were also related to the differences between the adolescent and adult groups (
Table 3). The histologic changes in the epidermis were more significant in the adolescent group than in the adult group. Of the 40 total specimens, 19 were in the adult group (of which four were in the flexural area), whereas 21 were in the adolescent group (of which seven were in the flexural area). The reason for the more prominent histologic changes in the adolescent group might be that they had a greater flexural involvement. This is the reason why histologic changes of AN were found more commonly than those of CRP because AN is mainly present in the flexural area of the body
11. As reported in many studies, patients with AN have associated malignancy
12 and endocrine problems
13; however, no such underlying disease was reported in patients with CRP in this study. Fungal infections appeared at a higher rate in the current study than in previous studies (
Table 4). Of the 29 patients, five were no longer followed up, while the patients with fungal infections were treated with doxycycline and itraconazole. The rest of the patients were treated with doxycycline alone or combination therapy with phototherapy (narrow-band ultraviolet B), and their skin lesions improved thereafter. The 24 patients who completed the treatment were then examined to see how the treatment responses varied depending on their age, sex, and anatomic site. However, due to the small sample size within each treatment group, for which the same treatment was provided, assessment of treatment response could not be analyzed.
Table 5
Histopathologic feature according to the anatomic site
|
Characteristic |
Flexural area (axilla and neck, n=12) |
Non-flexural area (n=28) |
|
Grade (0~3+) |
0 |
1+ |
2+ |
3+ |
0 |
1+ |
2+ |
3+ |
|
Hyperkeratosis |
0 |
6 (50) |
5 (41.7) |
1 (8.3) |
2 (7.1) |
14 (50) |
12 (42.9) |
0 |
|
Parakeratosis |
0 |
0 |
0 |
0 |
0 |
1 (3.6) |
0 |
0 |
|
Acanthosis |
0 |
6 (50) |
5 (41.7) |
1 (8.3) |
5 (17.9) |
16 (57.1) |
7 (25) |
0 |
|
Papillomatosis |
2 (16.7) |
1 (8.3) |
7 (58.3) |
2 (16.7) |
7 (25) |
10 (35.7) |
10 (35.7) |
1 (3.6) |
|
Dermal inflammatory cell infiltrate |
3 (25) |
9 (75) |
0 |
0 |
7 (25) |
21 (75) |
0 |
0 |

An additional study attempted to investigate whether there is a histologic difference according to erythematous-colored lesions and hyperpigmented lesions clinically seen in CRP; however, only six of the 29 patients had erythematous-colored CRP lesions. Therefore, it was difficult to obtain meaningful results owing to an insufficient number of samples.
There have been few studies regarding this condition on the Korean population, except for several case reports. In particular, an analysis of the association between age and anatomic site, as in this study, would aid in our understanding of the characteristics of CRP that have not yet been clarified.
The limitations of this study are as follows. First, the subject cohort was not large enough to enable further studies, such as determining sex-specific differences. Second, because the study had a retrospective design, there was a lack of multidisciplinary gathering of patient information, such as body weight, occupation, and previous skin problems, and many patients did not attend follow-up sessions to determine the treatment efficacy. Third, if the normal tissues of each patient were compared, individual differences might have been analyzed. In addition, histologic differences by body sites were not considered in this study. If large-scale and multicenter studies involving ethnic differences are conducted in the future, it will help us understand this disease better.
In conclusion, this study is the first to present the clinical and histologic features of CRP according to age and anatomic site in Korean patients. Skin lesions were seen at various sites, such as the neck, axillae, and bilateral extremities, in addition to the trunk. Histologic changes were more prominent in the adolescent group than in the adult group and in the flexural area than in the non-flexural area. The patients in this study more frequently had fungal infections (31%) than those in a previous study (12.8%).
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download