1. Yonsei University Medical School Dermatology. Yonsei university medical school dermatology 100 years. Seoul: Koonja;2017.
2. Roh MR, Lee KH, Lee S. HaeKwan Kung Sun Oh. In : Löser C, Plewig G, Burgdorf W, editors. Pantheon of Dermatology: outstanding historical figures. Heidelberg: Springer;2013. p. 816–820.
3. Park YK. Dermatology in Korea. Skinmed. 2007; 6:107–110. PMID:
17478987.

4. Parish LC, Woo TH. Kung Sun Oh: patriarch of Korean dermatology. Arch Dermatol. 1968; 98:406–407. PMID:
4877726.

5. Kee CD. Dr. Kung Sun Oh and the department of dermatology of Yonsei university college of medicine. Korean J Med Hist. 1996; 5:147–154.
6. Bang D, Chung KY. Early roots of western medicine and a pioneer of social work in Korea: Dr. Kung Sun Oh (1878-1963). Yonsei Med J. 2016; 57:277–282. PMID:
26847276.

7. Lee JB, Lee MG, Kim HI, Lee SN. 19S (IgM) - FTA test in untreated syphilitic patients. Korean J Dermatol. 1985; 23:630–634.
8. Lee JB, Farshy CE, Hunter EF, Hambie EA, Wobig GH, Larsen SA. Detection of immunoglobulin M in cerebrospinalfluid from syphilis patients by enzyme-linked-immunosorbent-assay. J Clin Microbiol. 1986; 24:736–740. PMID:
3533984.
9. Bang DS, Lee ES, Sohn SH, Kim DY, Cho SH, Choi MJ. Behçet's disease in Korea. Seoul: Hanuri;2013.
10. Sohn S, Lee ES, Bang D, Lee S. Behçet's disease-like symptoms induced by the herpes simplex virus in ICR mice. Eur J Dermatol. 1998; 8:21–23. PMID:
9649665.
11. Lee KH, Chung HS, Kim HS, Oh SH, Ha MK, Baik JH, et al. Human alpha-enolase from endothelial cells as a target antigen of anti-endothelial cell antibody in Behçet's disease. Arthritis Rheum. 2003; 48:2025–2035. PMID:
12847697.
12. Lee S, Bang D, Lee ES, Sohn S. Behçet's disease: a guide to its clinical understanding: textbook and atlas. Berlin: Springer;2001.
13. Hann SK, Im S, Bong HW, Park YK. Treatment of stable vitiligo with autologous epidermal grafting and PUVA. J Am Acad Dermatol. 1995; 32:943–948. PMID:
7751463.

14. Hann SK, Koo SW, Kim JB, Park YK. Detection of antibodies to human melanoma cells in vitiligo and alopecia areata by western blot analysis. J Dermatol. 1996; 23:100–103. PMID:
8839236.
15. Hann SK, Lee HJ. Segmental vitiligo: clinical findings in 208 patients. J Am Acad Dermatol. 1996; 35:671–674. PMID:
8912558.

16. Hann SK, Chang JH, Lee HS, Kim SM. The classification of segmental vitiligo on the face. Yonsei Med J. 2000; 41:209–212. PMID:
10817021.

17. Kim DY, Oh SH, Hann SK. Classification of segmental vitiligo on the face: clues for prognosis. Br J Dermatol. 2011; 164:1004–1009. PMID:
21198540.

18. Woo TH, Kook HI, Cho KY, Park YK. Clinical observation on the allergic contact dermatities in Korea. Korean J Dermatol. 1972; 10:77–83.
19. Bae JM, Choi YY, Park CO, Chung KY, Lee KH. Efficacy of allergen-specific immunotherapy for atopic dermatitis: a systematic review and meta-analysis of randomized controlled trials. J Allergy Clin Immunol. 2013; 132:110–117. PMID:
23647790.
20. Wu WH, Park CO, Oh SH, Kim HJ, Kwon YS, Bae BG, et al. Thymic stromal lymphopoietin-activated invariant natural killer T cells trigger an innate allergic immune response in atopic dermatitis. J Allergy Clin Immunol. 2010; 126:290–299. PMID:
20624642.

21. Noh S, Jin S, Park CO, Lee YS, Lee N, Lee J, et al. Elevated galectin-10 expression of IL-22-producing T cells in patients with atopic dermatitis. J Invest Dermatol. 2016; 136:328–331. PMID:
26763457.

22. Jin S, Shin JU, Noh JY, Kim H, Kim JY, Kim SH, et al. DOCK8: regulator of Treg in response to corticotropinreleasing hormone. Allergy. 2016; 71:811–819. PMID:
26799599.

23. Lew W, Bowcock AM, Krueger JG. Psoriasis vulgaris: cutaneous lymphoid tissue supports T-cell activation and "Type 1" inflammatory gene expression. Trends Immunol. 2004; 25:295–305. PMID:
15145319.

24. Kim TG, Jee H, Fuentes-Duculan J, Wu WH, Byamba D, Kim DS, et al. Dermal clusters of mature dendritic cells and T cells are associated with the CCL20/CCR6 chemokine system in chronic psoriasis. J Invest Dermatol. 2014; 134:1462–1465. PMID:
24401998.

25. Lee MG, Borkowski TA, Udey MC. Regulation of expression of B7 by murine Langerhans cells: a direct relationship between B7 mRNA levels and the level of surface expression of B7 by Langerhans cells. J Invest Dermatol. 1993; 101:883–886. PMID:
7504029.

26. Lee MG, Tang A, Sharrow SO, Udey MC. Murine dendritic T cells (DETC) express the homophilic adhesion molecule E-cadherin. Epithelial Cell Biol. 1994; 3:149–155. PMID:
7550606.
27. Park JM, Je JH, Wu WH, Jee HJ, Lee SK, Lee MG. Attenuation of contact hypersensitivity by cell-permeable heat shock protein 70 in BALB/c mouse model. Exp Dermatol. 2012; 21:969–971. PMID:
23171464.

28. Lee SH, Elias PM, Proksch E, Menon GK, Mao-Quiang M, Feingold KR. Calcium and potassium are important regulators of barrier homeostasis in murine epidermis. J Clin Invest. 1992; 89:530–538. PMID:
1737844.

29. Ahn BK, Jeong SK, Kim HS, Choi KJ, Seo JT, Choi EH, et al. Rottlerin, a specific inhibitor of protein kinase C-delta, impedes barrier repair response by increasing intracellular free calcium. J Invest Dermatol. 2006; 126:1348–1355. PMID:
16575394.

30. Lee SH, Choi EH, Feingold KR, Jiang S, Ahn SK. Iontophoresis itself on hairless mouse skin induces the loss of the epidermal calcium gradient without skin barrier impairment. J Invest Dermatol. 1998; 111:39–43. PMID:
9665384.

31. Jeong SK, Kim HJ, Youm JK, Ahn SK, Choi EH, Sohn MH, et al. Mite and cockroach allergens activate protease-activated receptor 2 and delay epidermal permeability barrier recovery. J Invest Dermatol. 2008; 128:1930–1939. PMID:
18305573.

32. Kim SC, Kwon YD, Lee IJ, Chang SN, Lee TG. cDNA cloning of the 210-kDa paraneoplastic pemphigus antigen reveals that envoplakin is a component of the antigen complex. J Invest Dermatol. 1997; 109:365–369. PMID:
9284106.

33. Kim TH, Choi Y, Lee SE, Lim JM, Kim SC. Adjuvant rituximab treatment for pemphigus: a retrospective study of 45 patients at a single center with long-term follow up. J Dermatol. 2017; 44:615–620. PMID:
28186358.

34. Oh SW, Lee JS, Kim MY, Kim SC. COL7A1 mutational analysis in Korean patients with dystrophic epidermolysis bullosa. Br J Dermatol. 2007; 157:1260–1264. PMID:
17916216.

35. Gu LH, Kim SC, Ichiki Y, Park J, Nagai M, Kitajima Y. A usual frameshift and delayed termination codon mutation in keratin 5 causes a novel type of epidermolysis bullosa simplex with migratory circinate erythema. J Invest Dermatol. 2003; 121:482–485. PMID:
12925204.

36. Kim DS, Kim DH, Goo B, Cho YH, Park JM, Lee TH, et al. Immunotherapy of malignant melanoma with tumor lysatepulsed autologous monocyte-derived dendritic cells. Yonsei Med J. 2011; 52:990–998. PMID:
22028165.

37. Oh BH, Jang HS, Lee J, Choi MJ, Nam KA, Chung KY. Delayed reconstruction for the non-amputative treatment of subungual melanoma. Ann Dermatol. 2015; 27:417–422. PMID:
26273158.

38. Lee KY, Roh MR, Chung WG, Chung KY. Comparison of Mohs micrographic surgery and wide excision for extramammary Paget's disease: Korean experience. Dermatol Surg. 2009; 35:34–40. PMID:
19018812.

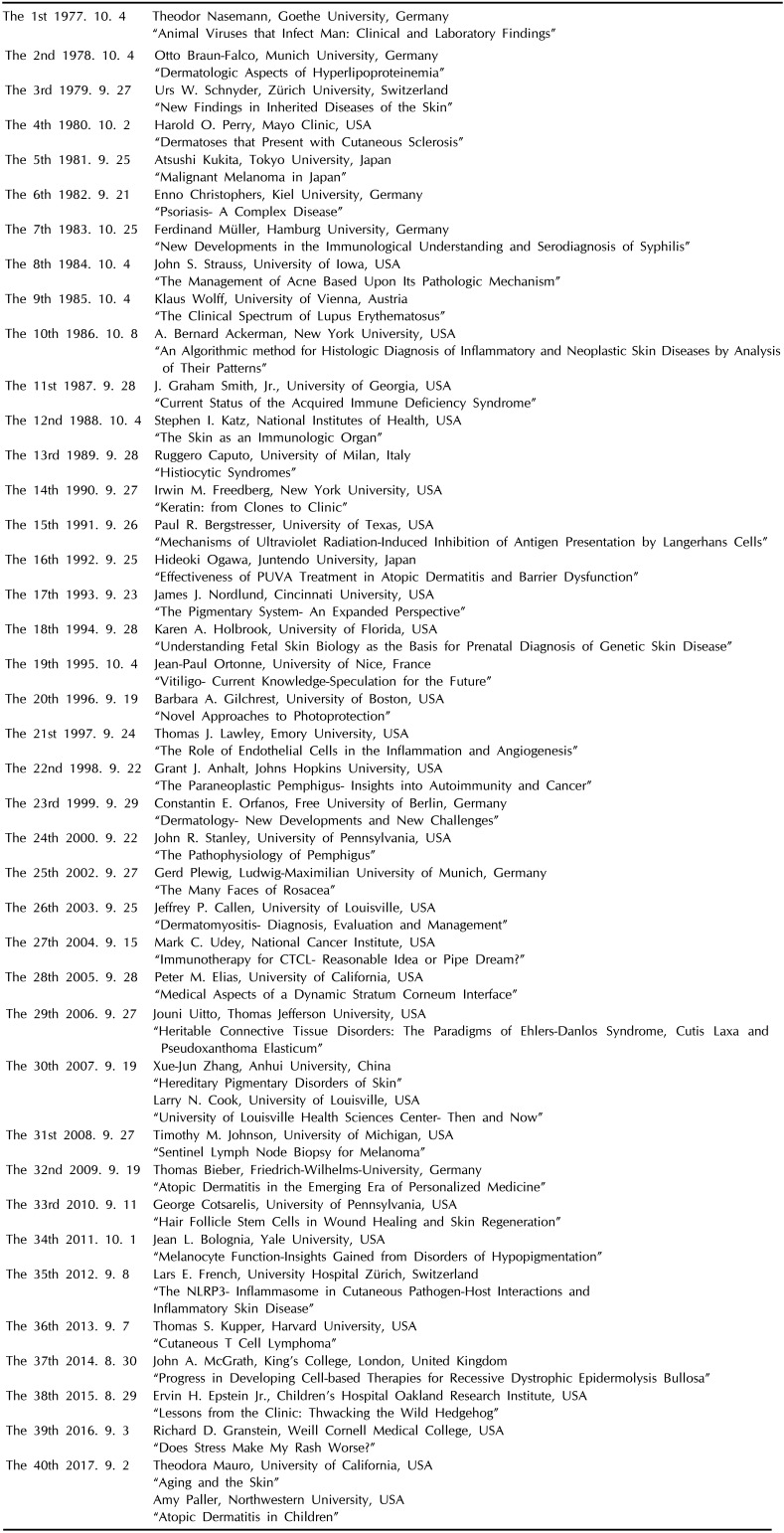
39. Nasemann T. The Kung-Sun-Oh memorial lecture and impressions on dermatology during a trip to South Korea. Hautarzt. 1978; 29:395–397. PMID:
681179.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download