This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
Despite advances in flexible ureteroscopy, the high cost and long repair time of ureteroscopes limit their use in the urology. We compared the performance of a novel flexible ureteroscope (fURS) ‘HF-EH’ with that of the two contemporary fURSs ‘URF-P6’ and ‘COBRA’.
Materials and Methods
We compared in vitro measurements of deflection angle, irrigation flow rate, and image quality between HF-EH and URF-P6 while also inspecting renal collecting systems in five female pigs. For clinical testing, we performed retrograde intrarenal surgeries using HF-EH in four patients. Experienced urologists compared performance parameters (irrigation, convenience, and maneuverability) between the HF-EH and COBRA.
Results
The flow rate of HF-EH (21.0 mL/min) was worse, and its resolution (1.59 line pairs/mm) was inferior to that of URF-P6 (28.7 mL/min and 3.17 line pairs/mm, respectively). However, HF-EH was superior to URF-P6 in terms of loss of deflection angle with the insertion of accessories (1.8% vs. 12.7%). In vivo and clinical testing revealed that the performance parameters of HF-EH were slightly inferior to those of conventional domestic fURSs. We successfully performed retrograde intrarenal surgeries using HF-EH in four patients and achieved stone-free statuses in two. None of the patients exhibited any procedure-related complications.
Conclusions
Although we observed that two of the three performance parameters of the novel ureteroscope ‘HF-EH’ were inferior to those of the conventional ureteroscope, we successfully used HF-EH to perform retrograde intrarenal surgeries in patients. Further studies on performance and durability are warranted for making HF-EH commercially available.
Go to :

Keywords: Lithotripsy, Nephrolithiasis, Ureteroscopes
INTRODUCTION
The first passive defecting flexible ureteroscope (fURS) was introduced by Marshall in 1964 [
1]. Since then, fURSs have improved with active deflection, incorporation of working and irrigation channels, secondary passive deflection, and better optical quality [
2]. Accessory requisites, such as guidewire, ureteral access sheaths, flexible stone baskets, stone forceps, and laser lithotripsy systems, have also been developed. These technological advancements have enabled urologists to better diagnose and manage urothelial malignances and urolithiasis of the upper urinary tract [
3].
Retrograde intrarenal surgery (RIRS) involves surgical management of upper urinary tract pathologies using a retrograde ureteroscope. RIRS is less invasive than percutaneous nephrolithotomy (PNL) for treating urolithiasis; it compensates for disadvantages of extracorporeal shockwave lithotripsy (ESWL). In 2011, only 301 RIRSs had been performed in Korea; however, by 2016, the number increased to 3,442 (approximately 11.5-fold in a 5-year-period) [
4]. The importance and efficiency of fURSs has also rapidly increased worldwide [
567].
However, currently available fURSs are highly expensive and completely dependent on imported parts. In addition, they easily get damaged and become nonfunctional during sterilizations and manipulations; repairing them in the manufacturing countries takes several months and is costly. These drawbacks limit the active utilization of RIRS to some degree. Consequently, the need for convenient and domestic fURSs was discussed in public and in the Ministry of Trade, Industry and Energy, Korea, has supported this project since 2015. Hyunjoo In-Tech, a domestic endoscopy company established in 1998, is the managing department for this study. Asan Medical Center collaborated with the company to develop a local fURS. This study aimed to perform, in vitro, in vivo, and clinical testing to evaluate the safety, stability, equivalence, usefulness, and performance of this newly developed domestic fURS.
Go to :

MATERIALS AND METHODS
Here, we compared the novel device ‘HF-EH’ (Hyunjoo In-Tech, Seoul, Korea) with the ‘URF-P6’ (Olympus, Tokyo, Japan) and ‘COBRA’ (Richard Wolf, Knittlingen, Germany) ureteroscopes.
1. In vitro testing
First, we compared the deflection angles of the distal ends between the HF-EH and URF-P6. We measured the maximum bending angles thrice while maintaining the maximum bending state and also calculated the average value for each instrument.
Next, we compared the flow rate of irrigation fluid between each fURS by measuring the amount of physiological saline solution that could pass through the scope for 1 minute at a pressure maintained at 100 mmHg. We measured the maximum bending angles and irrigation flow rates using three different states of the working channels: empty, using a 200-µm laser, and using a 1.9-Fr basket. We defined the degree of angle reduction as the absolute and relative values.
Finally, we compared the image quality of each instrument using a Chrome/Glass Distortion Target and a 3″×3″ Positive, 1951 USAF Resolution Target (Edmund Optics, Barrington, NJ, USA) [
8]. We captured three images from a 1-cm distance from the object and compared the best images obtained from each instrument.
2. In vivo testing
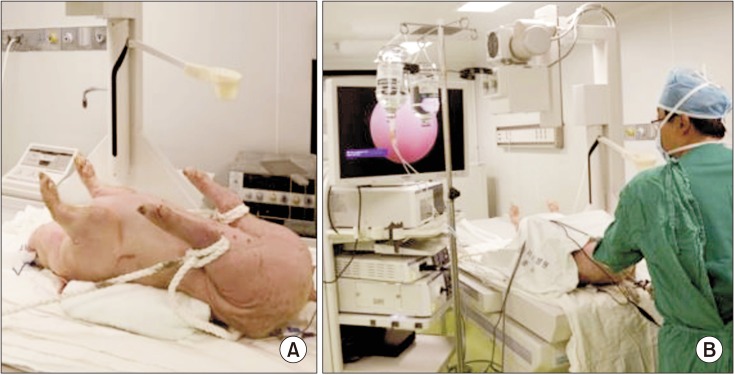
Five female pigs (Yorkshire; weight, 35–40 kg) were used for our
in vivo study. All procedures were performed under general anesthesia with endotracheal intubation. The anesthetized pigs were placed in the dorsal lithotomy position (
Fig. 1). We performed cystoscopies using a 19-Fr cystoscope, and inserted a 0.038-inch hydrophilic guidewire into the renal pelvis. After successful dilation of the ureter using a coaxial dilator, we inserted a ureteral access sheath (9.5/11.5 Fr; Cook Medical, Bloomington, IN, USA) to provide optimal visualization. We used an 8.5-Fr (HF-EH; Hyunjoo In-Tech) and 7.95-Fr fURS (URF-P6; Olympus) to inspect the renal collecting system. Two experienced endourologists who were familiar with COBRA not URF-P6 evaluated each instrument's performance. Each urologist provided subjective opinions regarding the following five parameters: insertion, control, maneuverability, rigidity, and image using a 10-point visual analogue scale [
9].
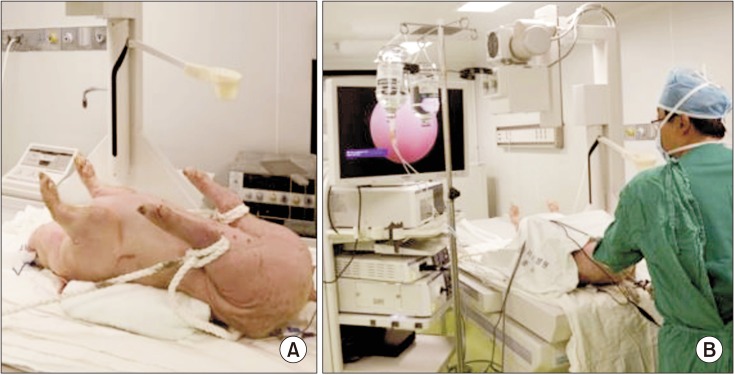 | Fig. 1
In vivo study model of retrograde intrarenal surgery. (A) Pig in dorsal lithotomy position. (B) Practicing on porcine model under the guidance of an experienced endourologist.
|
3. Clinical testing
After confirming the safety and efficacy in the animal model, we performed RIRS using HF-EH in four patients to confirm its stability and effectiveness in the actual clinical setting. Patients were prospectively enrolled after a thorough explanation about the study. The inclusion criteria were as follows: patients aged between 20 and 80 years; patients having renal stones comprising a maximum diameter of ≥1 cm as revealed by computed tomography (CT); patients with increasing stone sizes; patients with stones unsuitable for conservative therapy, medication, or ESWL; and patients with the presence of urinary tract infection, urinary obstruction, pain, and/or hematuria. The exclusion criteria were as follows: patients with active urinary tract infections, bleeding tendency, metabolic disorders, co-existing ureteric stones, or anatomical abnormalities of the urinary tract (single kidney, horseshoe kidney, ureteropelvic junction obstruction, etc.).
We placed all the patients in the lithotomy position under general anesthesia. We subsequently obtained a retrograde pyelogram to rule out ureteral stricture and downward migration of the stone. We used two stiff guidewires with a one-side floppy tip (Teflon 0.035″; Boston Scientific, Marlborough, MA, USA): one to introduce the device into the renal collecting system, and the second as a safety wire. All procedures were performed through an access sheath 11/13 Flexor TM (Boston Scientific) and Stone Light Ho; we used a YAG laser (PowerSuite; Lumenis, Yokneam, Israel) for lithotripsies. We introduced YAG laser fibers from Lumenis (200 µm) and nitinol baskets (Zero Tip 1.9 Fr; Boston Scientific) through the working channel (3.6 Fr) of the HF-EH to conduct the procedure. We inserted a double-J catheter at the end of the procedure and removed it at the outpatient clinic after surgery. Residual stones were detected using a kidney–ureter–bladder and a 3-mm-cut non-enhances CT scan one month later.
We used the same set of HF-EH throughout the study. During the operation, the surgeon (a skilled endourologist) himself scored three parameters of performance (irrigation, convenience, and maneuverability) on a five-point-scale. The ratings were as follows: 5, much better; 4, a little better; 3, no difference; 2, a little worse; and 1, much worse. We used the performance parameters of the COBRA, which is the fURS currently used at our center, as the control (point 3).
4. Statistical analysis
We used the IBM SPSS Statistics ver. 20.0 software (IBM Co., Armonk, NY, USA) for all statistical analyses. We used the chi-square or Fisher's exact test for categorical variables and the Wilcoxon signed-ranks and Mann–Whitney U-test for comparisons, owing to the small number of subjects in our groups. The p<0.05 was considered statistically significant.
5. Ethics statement
The Institutional Animal Care and Use Committee of the University of Ulsan approved the porcine model usage protocol (approval number: 2016-12-009). The Institutional Review Board of the Asan Medical Center, University of Ulsan College of Medicine, reviewed and approved the study protocol (approval number: 2017-0331). Informed consent was obtained from all subjects.
Go to :

RESULTS
1. Detailed information of HF-EH
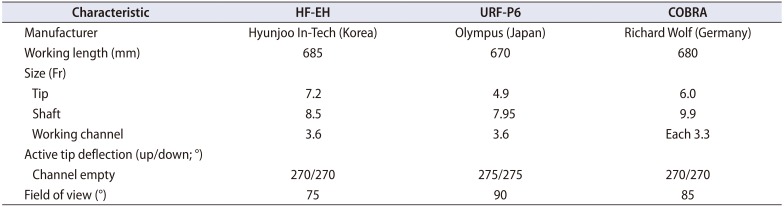
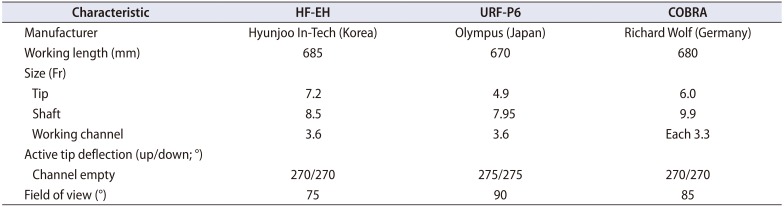
The technical specifications of the novel fURS ‘HF-EH’ in comparison with those of the two conventional fURSs ‘URF-P6’ and ‘COBRA’ are outlined in
Table 1. HF-EH has the longest working channel (685 mm) with the largest distal tip with an outer diameter of 7.2 Fr. Its shaft diameter was 8.5 Fr, larger than that of the URF-P6 (7.95 Fr), but smaller that of the COBRA (9.9 Fr). Both the HF-EH and URF-P6 have a single working channel sized 3.6 Fr; the COBRA has a dual working channel sized 3.3 Fr each.
Table 1
Baseline characteristics of flexible ureteroscopes
|
Characteristic |
HF-EH |
URF-P6 |
COBRA |
|
Manufacturer |
Hyunjoo In-Tech (Korea) |
Olympus (Japan) |
Richard Wolf (Germany) |
|
Working length (mm) |
685 |
670 |
680 |
|
Size (Fr) |
|
|
|
|
Tip |
7.2 |
4.9 |
6.0 |
|
Shaft |
8.5 |
7.95 |
9.9 |
|
Working channel |
3.6 |
3.6 |
Each 3.3 |
|
Active tip deflection (up/down; °) |
|
|
|
|
Channel empty |
270/270 |
275/275 |
270/270 |
|
Field of view (°) |
75 |
90 |
85 |

2. In vitro testing
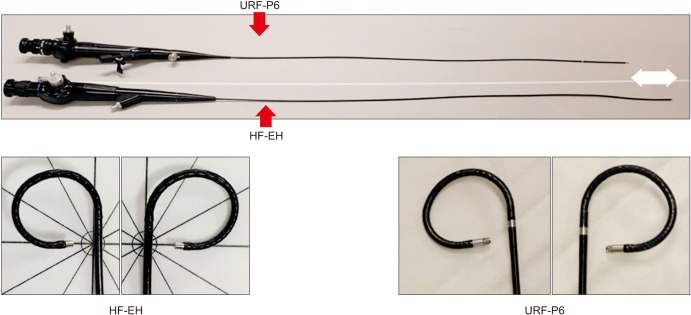
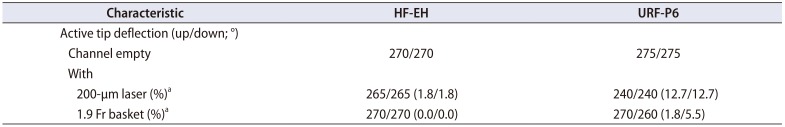
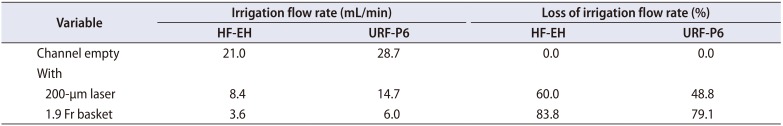
HF-EH is longer, but has a slightly smaller deflection angle than URF-P6 with an empty channel (
Fig. 2). However, the deflection angle of the HF-EH was better in the inserted instruments. Maximum reduction in the deflection angles of both fURSs was observed when using a 200-µm laser fiber (
Table 2). Compared with URF-P6, HF-EH displayed a worse flow rate in an empty working channel. The differences in irrigation flow rate between the two devices increased with instrument insertion. The 200-µm laser fiber reduced the flow rate of HF-EH and URF-P6 by 60.0% and 48.8%, respectively. Similarly, the 1.9-Fr stone removal basket reduced the flow rates of HF-EH and URF-P6 by 83.8% and 79.1%, respectively (
Table 3). Finally, under most conditions, compared with URF-P6, HF-EH had a worse resolution on the USAF test chart (1.59 line pairs/mm vs. 3.17 line pairs/mm;
Fig. 3). Both HF-EF and URF-P6 exhibited similar color presentations.
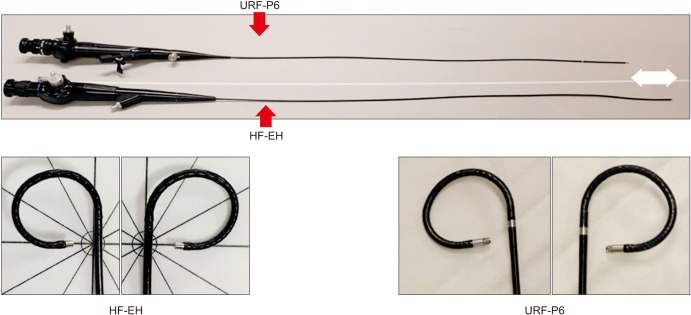 | Fig. 2Total length and maximal deflection of flexible ureteroscopes.
|
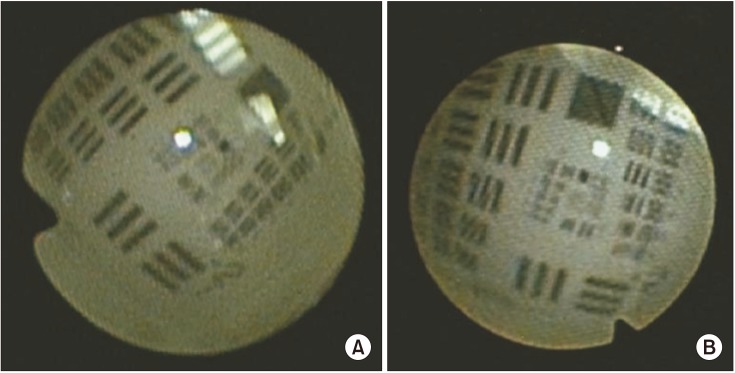
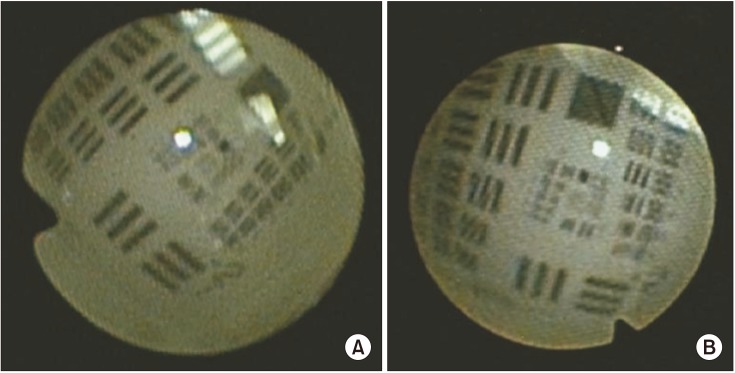 | Fig. 3USAF 1951 resolution target (A) HF-EH (1.59 line pairs/mm). (B) URF-P6 (3.17 line pairs/mm).
|
Table 2
Comparison between HF-EH and URF-P6 (deflection angle)
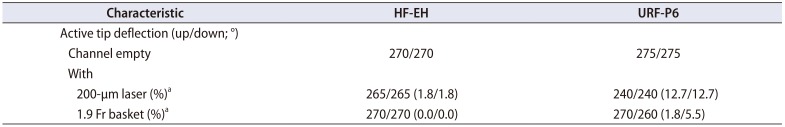
|
Characteristic |
HF-EH |
URF-P6 |
|
Active tip deflection (up/down; °) |
|
|
|
Channel empty |
270/270 |
275/275 |
|
With |
|
|
|
200-µm laser (%)a
|
265/265 (1.8/1.8) |
240/240 (12.7/12.7) |
|
1.9 Fr basket (%)a
|
270/270 (0.0/0.0) |
270/260 (1.8/5.5) |

Table 3
Comparison between HF-EH and URF-P6 (irrigation flow rate)
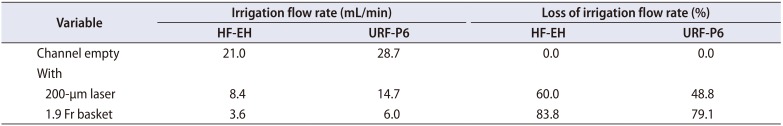
|
Variable |
Irrigation flow rate (mL/min) |
Loss of irrigation flow rate (%) |
|
HF-EH |
URF-P6 |
HF-EH |
URF-P6 |
|
Channel empty |
21.0 |
28.7 |
0.0 |
0.0 |
|
With |
|
|
|
|
|
200-µm laser |
8.4 |
14.7 |
60.0 |
48.8 |
|
1.9 Fr basket |
3.6 |
6.0 |
83.8 |
79.1 |

3. In vivo testing
Two endourologists independently documented the performance of each instrument in the animal model. The average scores were compared using the Wilcoxon signed-rank test, and the results have been presented as median values (
Fig. 4). HF-EH was significantly inferior to URF-P6 in terms of all parameters (except for rigidity). The observers particularly commented that HF-EH was inferior in terms of illumination and visualization in either clear or bloody fields.
 | Fig. 4Comparison of performance of flexible ureteroscopes in the porcine model. *p-values <0.05.
|
4. Clinical testing
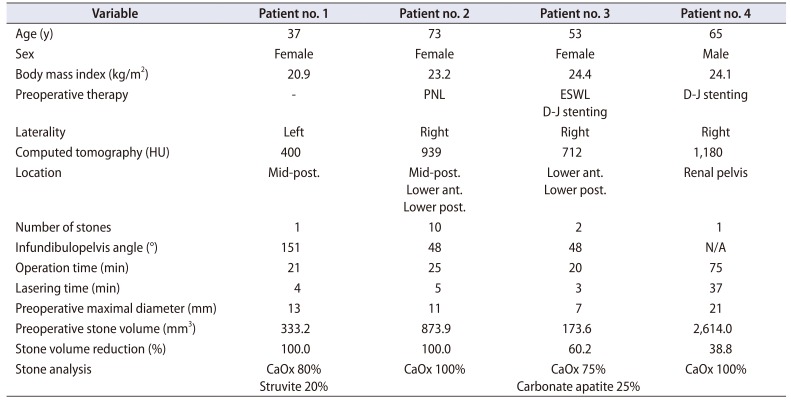
Four patients (three females and one male; mean age, 59.0±15.7 years) were enrolled in the study. Baseline demographics of the patients are presented in
Table 4. Patient no. 2 underwent PNL at a different hospital and visited Asan Medical Center for a second opinion about residual stones. Patient no. 3 had a right proximal ureter stone refractory to ESWL and had been scheduled for double-J stenting; however, the stone migrated to the kidney during the procedure. The location of the treated stone was heterogeneous. We found no significant differences in perioperative hemoglobin or serum creatinine levels among the patients. None of the patients exhibited any procedure-related complications after RIRS; stone-free statuses were achieved in two patients (50.0%). All stones were calcium oxalate-complex stones.
Table 4
Clinical characteristics of patients
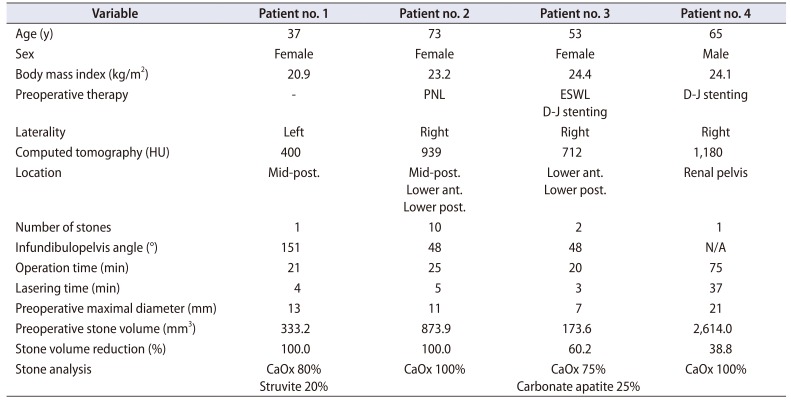
|
Variable |
Patient no. 1 |
Patient no. 2 |
Patient no. 3 |
Patient no. 4 |
|
Age (y) |
37 |
73 |
53 |
65 |
|
Sex |
Female |
Female |
Female |
Male |
|
Body mass index (kg/m2) |
20.9 |
23.2 |
24.4 |
24.1 |
|
Preoperative therapy |
- |
PNL |
ESWL |
D-J stenting |
|
D-J stenting |
|
Laterality |
Left |
Right |
Right |
Right |
|
Computed tomography (HU) |
400 |
939 |
712 |
1,180 |
|
Location |
Mid-post. |
Mid-post. |
Lower ant. |
Renal pelvis |
|
Lower ant. |
Lower post. |
|
Lower post. |
|
Number of stones |
1 |
10 |
2 |
1 |
|
Infundibulopelvis angle (°) |
151 |
48 |
48 |
N/A |
|
Operation time (min) |
21 |
25 |
20 |
75 |
|
Lasering time (min) |
4 |
5 |
3 |
37 |
|
Preoperative maximal diameter (mm) |
13 |
11 |
7 |
21 |
|
Preoperative stone volume (mm3) |
333.2 |
873.9 |
173.6 |
2,614.0 |
|
Stone volume reduction (%) |
100.0 |
100.0 |
60.2 |
38.8 |
|
Stone analysis |
CaOx 80% |
CaOx 100% |
CaOx 75% |
CaOx 100% |
|
Struvite 20% |
Carbonate apatite 25% |

The HF-EH deflection angles were measured before and after the operation, and they were 270/270 degrees in all cases. No abnormalities were observed in the leak test.
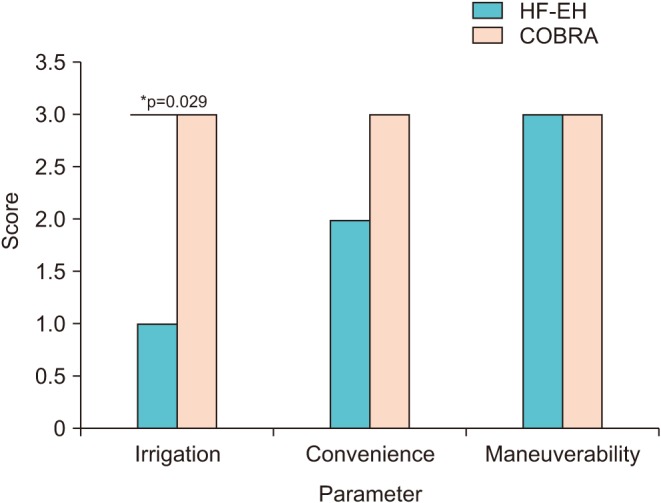
With regard to performance evaluation, for all parameters, HF-EH had equal or lower scores than those for COBRA. The variables in
Fig. 5 are presented as medians based on the Mann-Whitney U-test.
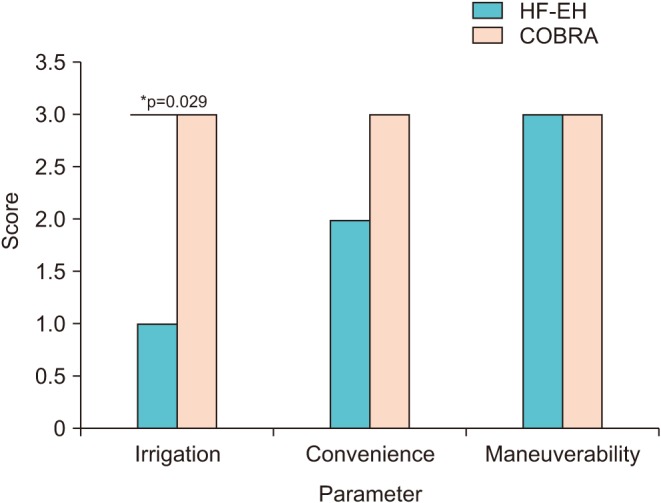 | Fig. 5Comparison of performance of flexible ureteroscopes in the clinical test. *p-values <0.05.
|
Go to :

DISCUSSION
The use of initial fURSs was initially limited to diagnosing upper urinary tract diseases. However, evolving technologies enabled scopes to become smaller, lighter, and easier to handle. RIRS cases with fURSs are steadily increasing worldwide, and the treatment guidelines for urolithiasis have been recently updated. The European Association of Urology guidelines 2016 recommend RIRS (endoscopic surgery) as the first-line treatment option for renal stones sized <20 mm, regardless of their location [
10]. In Korea, the main disadvantage of the current fURS system is its high cost, its reliance on imported parts, and frequent breakdowns, which require high-end technology and long repair times. The average fURS is used only 6–15 times before repair [
11]. However, our new domestic device (HFEH) would be able decrease the overall repair time and cost for RIRS performance, thereby making RIRS in Korea more available in the future.
Our in vitro study results revealed that the initial deflection angle of HF-EH was comparable with that of the conventional instrument (URF-P6). Further, the loss of deflection upon the insertion of the instrument was relatively low. Because RIRS requires frequent insertion and removal of auxiliary instruments, such as the laser fiber or basket, a minimal loss in the deflection angle is a crucial factor.
The irrigation fluid flow rate also considerably contributes to stone visualizations, which is critical for successful RIRSs [
12]. However, our current model showed deterioration of visual fields with worse irrigation. This phenomenon is probably caused by an irregular lumen of the working channels. In addition, due to our lack of experience in fiberoptic technology, the HF-EH had a worse resolution than the conventional ureteroscope did. This inferiority in clear visualizations may have resulted in the remnant stone in Patient no. 3 who had the smallest preoperative renal stone. However, a multistage approach is necessary for patients with larger renal stones. Patient no. 4 had an initial stone sized >2 cm (21×17×14 mm). The presence of remnant stones after performing the primary RIRS for a large renal stone makes it difficult to determine surgical failure [
13].
In summary, we were able to demonstrate that HF-EH is safe and effective and that it offers the possibility of achieving successful RIRS in clinical settings. One important advantage of this novel device is its sustained deflection angle, regardless of additional instrument insertion. However, it has two major disadvantages, which require improvement. First, we need to develop a better optic system for higher resolution. Second, we need to revise the current configuration of working channels for better irrigation flow rates.
The present study also has several limitations. First, the number of patients enrolled in the clinical testing was only four. Because this is the first test appliance of the device in real practice, the enrollment number was limited and the criteria had to be very strict. Second, we used different kinds of fURSs for comparison of each test; this made our results less reliable. Because COBRA is currently used at our center, it would have been much better to use COBRA for both in vivo and in vitro testing for more reliable comparisons. However, we decided to make comparisons with different scopes for the following two reasons: 1) because of its shaft size, COBRA is too tight for the access sheath used in our animal model; 2) the high cost of COBRA to be used only for animal experiments (it was impossible to sterilize and reuse COBRA after its use in animals); and 3) our study did provide long-term data regarding the durability of the new system. Further studies involving not only urologists but also generalists and video specialist after performance improvements and long-term use are mandatory for successful commercialization of this novel device.
Go to :

CONCLUSIONS
HF-EH is the first domestic fURS developed in Korea. Although HF-EH lacks capabilities compared with those of conventional fURSs, we were able to perform RIRS with a 50.0% stone-free rate and without complications. Further assessments regarding efficacy, safety, and durability are necessary; however, our results indicate that with proper upgrades and modifications, this novel ureteroscope may become commercially available within a short period of time.
Go to :

ACKNOWLEDGMENTS
This work was supported by the Ministry of Trade, Industry and Energy of Korea. The grant was funded by the Korean government (10054662).
Go to :

Notes
Go to :

References
1. Marshall VF. Fiber optics in urology. J Urol. 1964; 91:110–114. PMID:
14106571.

2. Abdelshehid C, Ahlering MT, Chou D, Park HK, Basillote J, Lee D, et al. Comparison of flexible ureteroscopes: deflection, irrigant flow and optical characteristics. J Urol. 2005; 173:2017–2021. PMID:
15879808.

3. Cho SY. Current status of flexible ureteroscopy in urology. Korean J Urol. 2015; 56:680–688. PMID:
26495068.

5. Lee MC, Bariol SV. Evolution of stone management in Australia. BJU Int. 2011; 108(Suppl 2):29–33. PMID:
22085123.

6. Raheem OA, Mirheydar HS, Miller DL, Palazzi KL, Chang DC, Sur RL. Contemporary trends in the ambulatory surgical treatment of urolithiasis: population-based analysis. J Endourol. 2015; 29:1189–1192. PMID:
25849858.

7. Ordon M, Urbach D, Mamdani M, Saskin R, D'A Honey RJ, Pace KT. The surgical management of kidney stone disease: a population based time series analysis. J Urol. 2014; 192:1450–1456. PMID:
24866599.

8. Lusch A, Abdelshehid C, Hidas G, Osann KE, Okhunov Z, Mc-Dougall E, et al. In vitro and in vivo comparison of optics and performance of a distal sensor ureteroscope versus a standard fiberoptic ureteroscope. J Endourol. 2013; 27:896–902. PMID:
23402369.

9. Parkin J, Keeley FX Jr, Timoney AG. Flexible ureteroscopes: a user's guide. BJU Int. 2002; 90:640–643. PMID:
12410739.

10. Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, et al. EAU guidelines on interventional treatment for urolithiasis. Eur Urol. 2016; 69:475–482. PMID:
26344917.

11. Tom WR, Wollin DA, Jiang R, Radvak D, Simmons WN, Preminger GM, et al. Next-generation single-use ureteroscopes: an in vitro comparison. J Endourol. 2017; 31:1301–1306. PMID:
28978227.

12. Haberman K, Ortiz-Alvarado O, Chotikawanich E, Monga M. A dual-channel flexible ureteroscope: evaluation of deflection, flow, illumination, and optics. J Endourol. 2011; 25:1411–1414. PMID:
21797758.

13. Gao X, Peng Y, Shi X, Li L, Zhou T, Xu B, et al. Safety and efficacy of retrograde intrarenal surgery for renal stones in patients with a solitary kidney: a single-center experience. J Endourol. 2014; 28:1290–1294. PMID:
24892920.

Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download