Abstract
Purpose
To see the 30-day unplanned readmission rates in patients underdoing endo-urological surgeries for upper urinary tract calculi we conducted this retrospective study at King George's Medical University, Lucknow, India. Unplanned readmissions not only add to healthcare costs but also are bothersome for the patients. There are many studies on 30-day unplanned readmissions in general surgical patients. Although similar studies have been done in certain urological procedures, no study has reported readmission rates or its risk factors in patients undergoing surgeries for upper urinary tract calculi.
Materials and Methods
We retrospectively reviewed our prospectively maintained database from 1st January 2009 to 31st December 2017, for the patients who underwent endo-urological procedures for upper urinary tract calculi and identified the patients who were re-admitted within 30 days of discharge.
Results
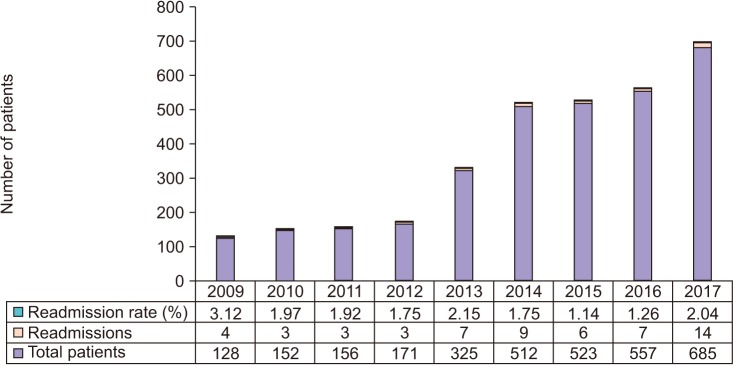
Out of the total 3,209 patients undergoing endo-urological procedures for upper urinary tract calculi 56 were re-admitted. The readmission rate was 1.74% over the study period. The most common etiology for readmission was sepsis followed by hematuria. The significant risk factors for readmission in bivariate analysis included male gender, age >65 years, current smoking, chronic obstructive pulmonary disease, diabetes mellitus, bleeding disorder, prior cardiac disease, and American Society of Anesthesiologists (ASA) class ≥3. In multivariate risk adjusted logistic regression analysis ASA class ≥3 was the only independent risk factor for readmission.
An important aspect for the healthcare system is financial burden on it and unplanned readmissions significantly add to this. The 30-day unplanned readmission rates have become an interesting area of study. Not only is this bothersome for the patients but adds to the cost of healthcare as well. Due to these reasons the health services in United States have increased the scrutiny into readmissions and in 2010 mandated to impose penalties for hospitals with higher readmission rates [12]. This is not limited to one country or region, the state run public healthcare facilities in India are already over burdened and unplanned readmissions add to that [3].
There have been various studies on unplanned readmissions in general surgical patients [456]. Recently studies have also been carried out to see readmission rates in patients undergoing urologic surgeries [789]. Among the various studies on 30-day unplanned readmissions across all fields, it has been observed that 9% to 59% of these readmissions are preventable [10]. There is no study till date focusing on 30-day readmission rates in patients undergoing endo-urological surgeries for upper urinary tract calculi. We thus conducted this study to see the readmission rates and the risk factors for readmission in these patients at King George's Medical University, Lucknow, India.
We retrospectively reviewed the records of our prospectively maintained database for all patients who underwent endo-urologic surgeries for upper urinary tract calculi at our center from 1st January 2009 to 31st December 2017. The institutional ethical committee exempted our study for requiring any formal ethical approval as it was retrospective and no procedures other than those regularly carried out were done. Informed consent was taken from the patient. The term ‘upper urinary tract calculi’ in our study was used for both ureteric and renal calculus. The procedures carried out were percutaneous nephrolithotomy (PCNL), semi-rigid ureterorenoscopy (URS) or retrograde intra-renal surgery (RIRS). The procedure done was based on the location of the stone and its size. Renal calculi at our institute are managed by PCNL and URS is done for ureteric calculi. RIRS was done either for proximal ureteric calculi or renal calculi (<1.5 cm). Because, ours is a state run institute there are issues with availability and cost of RIRS and hence the number of cases that underwent RIRS were less so for the purpose of analysis we combined URS and RIRS into one group.
We do all these procedures under spinal anesthesia at our institute. General anesthesia is only used if the patient prefers it, there is any contra-indication for spinal anesthesia or there is failure of spinal anesthesia. Urologists as well as urology residents in training perform the surgeries and we routinely place a ureteral stent after all the procedures. The ureteral stents are usually removed after 2 weeks.
PCNL is done in prone position at our institute. The urologist with the Bull's eye or the triangulation technique under fluoroscopic guidance does puncture. Tract dilation is done to a minimum of 24F and a pneumatic lithotripter is used as energy source for stone fragmentation. A nephrostomy tube is also routinely placed for minimum of 24 hours. URS is done in the lithotomy position with a 8/7.5F semi-rigid ureteroscope. A safety guide-wire is placed in all cases. If the patient is not pre-stented then the ureteric orifice is dilated with a balloon dilator. Holmium laser or pneumatic lithotripter is used for stone fragmentation. RIRS is done for either upper ureteric or renal calculi. We use ureteral access sheaths in all patients. If there is difficulty in passing ureteral access sheath then a stent is placed and the procedure is again attempted one week later. Holmium laser is used for stone fragmentation in these cases.
Out of the total 3,209 patients who underwent these procedures during the study period, we identified 56 patients who met our eligibility criteria that is unplanned readmission within 30 days of the principal surgery. Readmission is defined as a state when the patient is admitted to the same or a different hospital after being discharged from the applicable hospital to a non-acute setting, such as his home within a specified time period [6]. Only those patients who were re-admitted to our department were included in the study. The patients who were electively re-admitted, such as for surgery on contralateral side were not included. We recorded the demographic details, the interval between discharge and readmission, length of hospital stay during readmission, the cause for readmission and the management done in these patients. Along with this we recorded the potential risk factors for readmission in all 3,209 patients that included age, gender, diabetes mellitus (DM), hypertension, chronic kidney disease (CKD), cardiac illness, chronic liver disease, any bleeding disorders, chronic obstructive pulmonary disease (COPD), current smoking, and American Society of Anesthesiologist (ASA) class ≥3. We divided the patients into two groups, that is those with and without readmissions and then analyzed the risk factors statistically in a bivariate analysis model. In addition we did a sub group bivariate analysis for risk factors of readmission in patients undergoing PCNL and URS/RIRS separately. The categorical variables were analyzed using chi square test whereas the student t-test was used for continuous variables. A p-value of <0.05 was considered significant. Those factors that had a p-value of <0.2 and had 5 or more occurrences were combined and analyzed in a multivariate logistic regression model to look for independent risk factors of readmission. All statistical analysis was done using IBM SPSS Statistics ver. 21.0 software (IBM Co., Armonk, NY, USA).
Of the total 3,209 patients, 2,380 patients (74.2%) underwent PCNL and 829 patients (25.8%) underwent either URS or RIRS. The number of patients who underwent RIRS was only 132. The 30-day unplanned readmission rate over the study period was 1.74%. The 30-day unplanned readmission rates during each year are given in Fig. 1. Among the surgical procedures the readmission rates for PCNL was 1.59% and that for URS/RIRS was 2.17%. The difference in readmission rates between these procedures was statistically insignificant (p=0.277). The characteristics of readmitted patients are given in Table 1. The mean interval between the discharge f rom hospital and readmissions was 11.38±6.81 days and the mean hospital stay during readmission was 5.93±4.25 days. Sepsis was the most common etiology for readmission seen in 57.1% cases; the next most common etiology was hematuria (30.4%). Eight patients were admitted due to severe bladder spasm or other stent related symptoms. All 17 patients with hematuria had undergone PCNL. Of these 6 patients required evacuation of clots in the urinary bladder under anesthesia, 8 patients had a pseudo-aneurysm in the kidney following PCNL for which they underwent angio-embolization and rest of them were managed conservatively with bed rest and hydration. Out of the 56 re-admitted patients 2 patients required haemo-dialysis; one of these had aminoglycoside-induced nephrotoxicity. Table 2 depicts the characteristics of patients that underwent PCNL versus those who underwent URS/RIRS, it also depicts the stone location in these patients.
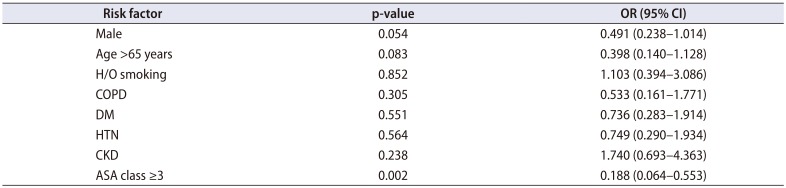
The mean age of the patients who were re-admitted was significantly higher than the non readmission group. On bivariate analysis male gender, age >65 years, current smoking, COPD, DM, bleeding disorder, prior cardiac disease, and ASA class ≥3 were significant risk factors for readmission (Table 3). The sub group bivariate analysis of patients undergoing PCNL and URS/RIRS separately for risk factors of readmission is depicted in Table 4. The significant factor common to both were DM and ASA class ≥3. On risk adjusted multivariable regression analysis ASA class ≥3 (odds ratio, 0.188; 95% confidence interval, 0.064–0.553; p=0.002), was the only significant independent risk factor for 30 days unplanned readmissions (Table 5).
Ours is a tertiary care referral center in Northern India and the bed occupancy rates are close to 100%. Unplanned readmissions are not only disturbing for the patients who are re-admitted but also for other patients who are awaiting elective surgical procedures. Readmission rates for major urological surgeries including radical cystectomy and prostatectomy were found to be 5.8% [8]. The patients who undergo surgeries for urological malignancies are usually older and have a lower performance status and probably it is expected that they will have a longer hospital stay with higher readmission rates. Endo-urological surgeries for upper urinary tract calculi, as shown in our study have a lower readmission rate (1.7%) that can be lowered even more by limiting the modifiable risk factors.
Advanced age has been associated with adverse outcomes in urological procedures [11]. In 2 previous studies on readmission in urological procedures as well as in our study age was significantly higher in re-admitted patients. The other factors that were significant contributors to readmission in our study as well as the 2 previous studies on 30-day readmissions for urological procedures included male gender, current smoking, COPD, DM, previous cardiac illness, bleeding disorders, and ASA class >3 [78]. The first study included only the five most common urological procedures: trans-urethral resection of bladder tumor, laser prostatectomy, trans-urethral resection of prostate, hydrocele excision, and sling surgery for urinary incontinence. The overall readmission rate in this study was 3.7% [7]. The second study included open and laparoscopic or robotic procedures with a readmission rate of 5.8% [8]. Both of the studies mentioned vide supra did not include endo-urological procedures for upper urinary tract calculi. In another study of 30-day unplanned readmission rates in urology patients, there were 7 cases that were readmitted after ureteroscopy but the authors did not mention the indication for the procedure or the readmission rates specifically for it [9].
In our study the most common etiology for readmission was sepsis. Sepsis post PCNL has been extensively studied. The risk factors for sepsis following PCNL include positive urine culture, stone size, infected stone, neurogenic bladder dysfunction, abnormal renal anatomy, long operative times, nephrostomy tube placement in females, and urethral catheter placement [12]. The American Urological Association and European Urological Association both recommend the use of prophylactic antibiotics in patients undergoing PCNL [1213]. Sepsis may even occur with sterile urine cultures preoperatively, because the fragmentation of stone containing bacteria in a high-pressure system during PCNL leads to dissemination of bacterial endotoxins and bacteria into the blood stream. The renal pelvic urine or stone culture is a better indicator for post PCNL sepsis than preoperative urine culture of urine from the urinary bladder [14]. The data about risk factors for sepsis after URS is comparatively scarce. They include prior ureteral stenting, bilateral calculi, calculus >10 mm, positive preoperative urine culture, and female gender [15]. The risk of sepsis is also related to high intra-pelvic pressure during ureteroscopy that can be reduced by placing an access sheath in patients that undergo RIRS. We however could not analyze this fact as the patients that underwent RIRS were less and only 2 among them were readmitted.
Hematuria is a known complication of PCNL with incidence ranging from 3% to 28%. The risk factors for post PCNL hematuria include larger stone burden, multiple punctures, superior calyceal puncture, solitary kidney, and CKD [1617]. Most of the times it is venous bleed that can be managed conservatively with hydration and putting a nephrostomy tube. When there is a high-pressure arterial bleed then there are chances of formation of pseudo-aneurysms or arterio-venous fistulas requiring angio-embolization [17]. When there is delayed post PCNL hematuria then most of the times conservative management is sufficient. If the patient is stable and conservative management fails then only angiography and angioembolization are required [18]. In our study only 8 of the 17 patients with readmission due to hematuria required angiography followed by angio-embolization.
It should be kept in mind that all of the studies regarding sepsis and hematuria post endo-urological surgeries for upper urinary tract calculi have mentioned risk factors for postoperative complications and not 30-day unplanned readmissions. But, because sepsis and hematuria were major etiologies for readmissions probably the results of these studies can be extrapolated to readmissions as well.
Recent literature reports that URS is on the rise and is being performed more commonly than PCNL [19]. In our study PCNL was the most common procedure performed, this may be because of our institute being a tertiary care referral center for the region. URS being simpler than PCNL is also being performed in numbers in peripheral centers whereas most cases suitable for PCNL are referred to us thus probably we do more PCNLs.
The only significant factor in multivariate logistic regression analysis was an ASA class ≥3. The ASA score provides a subjective assessment of overall health of the patient. It is divided into 6 classes ranging from ASA I for a healthy person and ASA VI for a brain dead person whose organs are being removed for donation [20]. An ASA class ≥3 has been consistently associated with 30-day unplanned readmissions across surgical specialties [467821]. Our study corroborated with these findings with ASA class ≥3 being the strongest independent predictor of 30-day unplanned readmissions.
There are certain limitations to our study. Firstly, it is retrospective in nature. Second, ours is a state-run hospital with no bed charges so patients usually stay longer as compared to institutes with bed-charges. Thirdly, we do not have data for those patients who were re-admitted in other hospitals after the index surgery. And finally, we could not analyze stone characteristics (size and location) in the risk factors for readmissions because we had combined renal and ureteric calculi into the readmission group, although we feel that those stone characteristics (such as stone size) that increase the likelihood of sepsis or hematuria should increase the likelihood of readmissions as well.
The strength of our study lies in the fact that we have studied the readmission rates in patients with stone disease that form a substantial proportion of patients admitted in any urology department, and probably this is the first study doing so.
The overall 30-day unplanned readmission rate in our study was 1.74%. On multivariate logistic regression analysis ASA class ≥3 was the only significant independent risk factor for readmission. These findings may benefit the patients undergoing endo-urological surgeries for upper urinary tract calculi. We feel that this data needs to be substantiated by prospective multicenter studies that probably analyze only renal or only ureteric stones.
References
1. Hockenberry JM, Burgess JF Jr, Glasgow J, Vaughan-Sarrazin M, Kaboli PJ. Cost of readmission: can the Veterans Health Administration (VHA) experience inform national payment policy? Med Care. 2013; 51:13–19. PMID: 22683595.
2. Orszag PR, Emanuel EJ. Health care reform and cost control. N Engl J Med. 2010; 363:601–603. PMID: 20554975.

3. Balarajan Y, Selvaraj S, Subramanian SV. Health care and equity in India. Lancet. 2011; 377:505–515. PMID: 21227492.

4. Kassin MT, Owen RM, Perez SD, Leeds I, Cox JC, Schnier K, et al. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg. 2012; 215:322–330. PMID: 22726893.

5. Amodu LI, Alexis J, Soleiman A, Akerman M, Addison P, Iurcotta T, et al. Predictors of 30-day readmission following pancreatic surgery: a retrospective review. Hepatobiliary Pancreat Dis Int. 2018; 17:269–274. PMID: 29716791.

6. Marwah S, Singla P, Singh M, Sharma H. Risk factors for 30-day unplanned readmission among patients undergoing laparotomy for perforation peritonitis. Int Surg J. 2017; 4:637–644.

7. Rambachan A, Matulewicz RS, Pilecki M, Kim JY, Kundu SD. Predictors of readmission following outpatient urological surgery. J Urol. 2014; 192:183–188. PMID: 24518788.

8. Stone BV, Cohn MR, Donin NM, Schulster M, Wysock JS, Makarov DV, et al. Evaluation of unplanned hospital readmissions after major urologic inpatient surgery in the era of accountable care. Urology. 2017; 109:94–100. PMID: 28801217.

9. Raslan M, Floyd M, Itam S, Mukherjee R, Irwin P, Maddineni S. Unplanned urology readmissions in a district general hospital: are we meeting the standard? J Clin Urol. 2013; 6:289–294.

10. Feigenbaum P, Neuwirth E, Trowbridge L, Teplitsky S, Barnes CA, Fireman E, et al. Factors contributing to all-cause 30-day readmissions: a structured case series across 18 hospitals. Med Care. 2012; 50:599–605. PMID: 22354212.
11. Sommer F, Ehsan A, Caspers HP, Klotz T, Engelmann U. Risk adjustment for evaluating the outcome of urological operative procedures. J Urol. 2001; 166:968–972. PMID: 11490257.

12. Lojanapiwat B. Infective complication following percutaneous nephrolithotomy. Urol Sci. 2016; 27:8–12.

13. Kreydin EI, Eisner BH. Risk factors for sepsis after percutaneous renal stone surgery. Nat Rev Urol. 2013; 10:598–605. PMID: 23999583.

14. Rashid AO, Fakhulddin SS. Risk factors for fever and sepsis after percutaneous nephrolithotomy. Asian J Urol. 2016; 3:82–87. PMID: 29264169.

15. Nevo A, Mano R, Baniel J, Lifshitz DA. Ureteric stent dwelling time: a risk factor for post-ureteroscopy sepsis. BJU Int. 2017; 120:117–122. PMID: 28145037.

16. Srivastava A, Singh KJ, Suri A, Dubey D, Kumar A, Kapoor R, et al. Vascular complications after percutaneous nephrolithotomy: are there any predictive factors? Urology. 2005; 66:38–40. PMID: 15992882.

17. El-Nahas AR, Shokeir AA, El-Assmy AM, Mohsen T, Shoma AM, Eraky I, et al. Post-percutaneous nephrolithotomy extensive hemorrhage: a study of risk factors. J Urol. 2007; 177:576–579. PMID: 17222636.

18. Nouralizadeh A, Ziaee SA, Hosseini Sharifi SH, Basiri A, Tabibi A, Sharifiaghdas F, et al. Delayed postpercutaneous nephrolithotomy hemorrhage: prevalence, predictive factors and management. Scand J Urol. 2014; 48:110–115. PMID: 24256570.

19. Perera M, Papa N, Kinnear N, Wetherell D, Lawrentschuk N, Webb D, et al. Urolithiasis treatment in australia: the age of ureteroscopic intervention. J Endourol. 2016; 30:1194–1199. PMID: 27629239.

20. Doyle DJ, Garmon EH. American Society of Anesthesiologists Classification (ASA Class). StatPearls. Treasure Island (FL): StatPearls Publishing;2018.
21. Ali AM, Gibbons CE. Predictors of 30-day hospital readmission after hip fracture: a systematic review. Injury. 2017; 48:243–252. PMID: 28063674.

Table 1
Characteristics of patients with 30 days unplanned readmissions
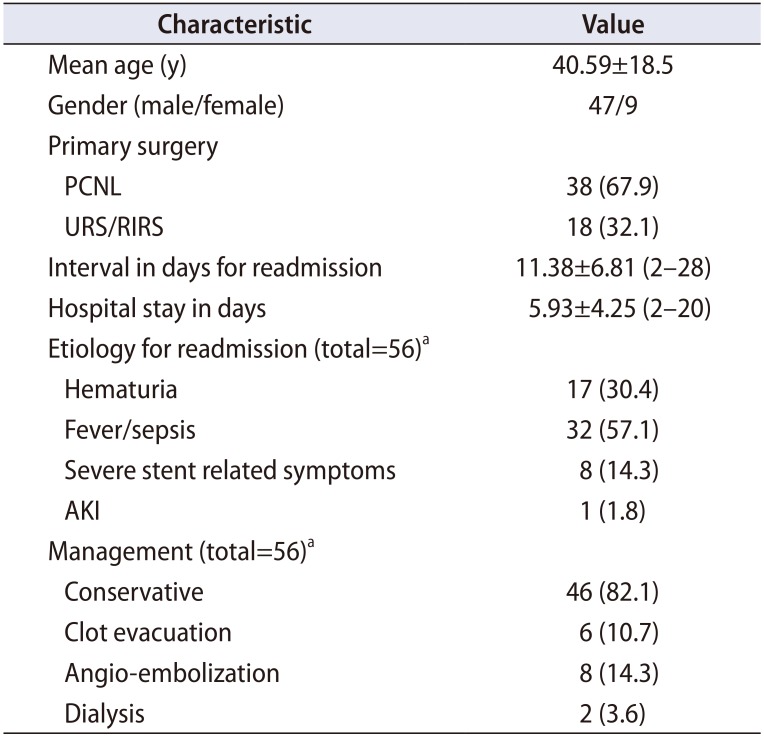
Table 2
Description of characteristics of patients who underwent PCNL versus URS/RIRS
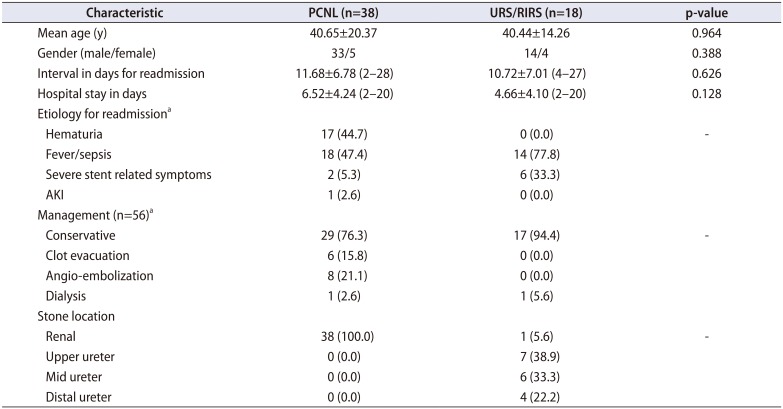
Table 3
Analysis of risk factors in patients with and without 30 day unplanned readmissions
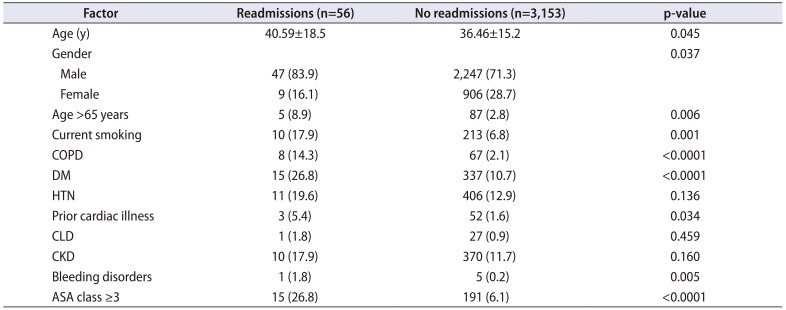
Table 4
Bivariate analysis of risk-factors for readmission separately for PCNL and URS/RIRS
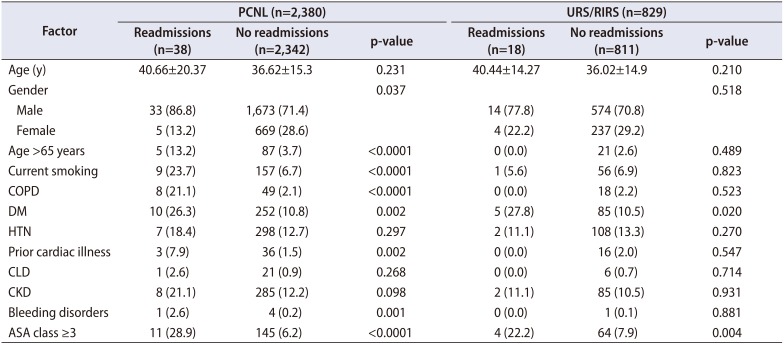
Values are presented as mean±standard deviation or number (%).
PCNL, percutaneous nephrolithotomy; URS, semi-rigid ureterorenoscopy; RIRS, retrograde intra-renal surgery; COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; HTN, hypertension; CLD, chronic liver disease; CKD, chronic kidney disease; ASA, American Society of Anesthesiologist.
Table 5
Multivariate risk adjusted logistic regression analysis of risk factors for unplanned 30 days readmissions




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download