Abstract
Purpose
To evaluate longitudinal changes in health-related quality of life and satisfaction after radical prostatectomy for the treatment of prostate cancer in Korean men.
Materials and Methods
Data from patients with localized prostate cancer who underwent radical prostatectomy between January 2012 and December 2013 were analyzed. Patients completed the Expanded Prostate Cancer Index Composite questionnaire at scheduled clinic visits (baseline and 1, 3, 6, and 12 months post-surgery).
Results
Data from 211 men were evaluated. Urinary domain summary scores decreased postoperatively but improved over the 12-month follow-up period. Urinary function and incontinence had not recovered to baseline values at 12 months, whereas urinary bother and irritation/obstruction scores showed no differences from baseline at 12 months. Sexual function improved at each timepoint to 12 months but did not recover to baseline values; sexual bother was approximately 50% of baseline values at 12 months. Recovery of sexual function was significantly greater in patients who underwent robotic surgery versus those who underwent open surgery. At the end of the study period, 66.3% of patients were satisfied with the treatment they had received; multivariate analysis showed that only urinary function recovery was significantly associated with overall satisfaction.
Conclusions
Urinary outcomes and sexual outcomes had not returned to baseline at 12 months. Recovery of sexual function was significantly greater in patients who underwent robotic surgery. Only recovery of urinary function was significantly associated with overall satisfaction 12 months after radical prostatectomy in this cohort of Korean men.
Radical prostatectomy is a key approach to the treatment of localized prostate cancer. The procedure is associated with favorable survival, highlighting the importance of health-related quality of life (HRQOL) and functional outcomes after surgery [123]. Urinary incontinence and erectile dysfunction are common adverse events and may have a profound impact on HRQOL in patients with prostate cancer. Patients with clinically localized prostate cancer have multiple treatment options and the risk:benefit balance is an important aspect in treatment decision-making [4]. Two recent population-based prospective cohort studies have evaluated HRQOL after contemporary treatments for localized prostate cancer, showing a distinct pattern of adverse effects associated with each treatment strategy [56].
The incidence of prostate cancer has increased steadily over the last decade in East Asia, most significantly in Korea [7]. Although a number of studies have examined HRQOL after radical prostatectomy in Western and Japanese populations [8], to date, none have evaluated Korean prostate cancer patients. The heterogeneity of prostate cancer has been documented in patients from different geographical and ethnic populations [9]. Race and ethnicity are also important factors in HRQOL assessment as they are known to impact on satisfaction with care [10].
In this study, we have prospectively evaluated longitudinal changes in HRQOL in Korean prostate cancer patients after radical prostatectomy. In addition, we have attempted to identify factors that may impact on overall satisfaction after treatment.
Data from patients who underwent radical prostatectomy at Asan Medical Center between January 2012 and December 2013 were reviewed. All surgery was conducted by a single, highly experienced surgeon. Patients were required to complete the Expanded Prostate Cancer Index Composite (EPIC) questionnaire at baseline and post-surgery. Patients who received neoadjuvant or adjuvant therapy and those with inadequate clinical data or incomplete questionnaires were excluded. The study protocol was approved by the Institutional Review Board of Asan Medical Center (approval number: 2012-0036) and informed consent was obtained from each patient.
Patients were routinely scheduled to visit the clinic at baseline and at 1, 3, 6, and 12 months post-surgery. At each visit, patients were asked to complete the Korean version of the EPIC [11] questionnaire on paper in the waiting room before meeting the urologist.
The EPIC questionnaire consists of 50 questions and is divided into four domains: bowel, urinary, sexual, and hormonal. The four domain summary scores and subscale scores were calculated on a scale of 0–100, with higher scores representing better HRQOL [12].
Overall satisfaction was determined based on a single question ‘Overall, how satisfied are you with the treatment you received for your prostate cancer?’ Patients who responded that they were ‘extremely satisfied’ or ‘satisfied’ were classified as the ‘satisfied’ group.
Paired t-tests were used to assess differences in subscale scores at each timepoint and at different timepoints along the same domain or subscale. Repeated-measures ANOVA was used to compare HRQOL changes over time between patients undergoing robot-assisted laparoscopic prostatectomy (RALP) and those undergoing retropubic radical prostatectomy (RRP). Multivariate analysis with a stepwise backwards elimination approach was performed to identify significant influencing factors for overall satisfaction after treatment. All statistical tests were two-tailed with a significance level of 0.05; analyses were performed using IBM SPSS Statistics ver. 21.0 software (IBM Co., Armonk, NY, USA).
Data from a total of 211 patients were included in the analyses. Each patient was evaluated at five visits; therefore, a total of 1,055 EPIC questionnaires and medical records were analyzed. Patient characteristics are summarized in Table 1; the mean patient age was 64.7 years, mean prostate-specific antigen level was 10.5 ng/mL, and mean prostate volume was 35.0 mL. Of the 211 patients, 136 (64.4%) had organ-confined prostate cancer and 168 (79.6%) underwent robot-assisted radical prostatectomy.
Urinary domain summary scores are shown in Fig. 1A. Prior to surgery, mean urinary function scores were higher than urinary bother scores. However, at 1 month, urinary function had decreased to a greater extent than urinary bother. Urinary function improved at 3 months and reached a new baseline at 6 months. Urinary function had not recovered fully at 12 months, whereas urinary bother showed no difference from baseline at 12 months.
In the EPIC questionnaire, the urinary domain is separated into two distinct subscales, incontinence and irritation/obstructive (Fig. 1B). At 1 month post-surgery, mean urinary incontinence had decreased by a greater degree than mean irritation/obstruction. Although mean urinary incontinence had improved at 12 months, values did not return to baseline. By contrast, following a slight decrease at 1 month, mean urinary irritation/obstruction returned to baseline at 3 months and then rose above baseline from 6 months onwards. Medical records showed that 14.2% of patients were incontinent at 12 months post-surgery in this study cohort.
Post-surgery sexual domain scores showed the greatest reduction of all four domains. At baseline, mean sexual function was lower than mean sexual bother (Fig. 1C). At 1 month, the mean sexual function score had decreased greatly from baseline. Gradual improvement was seen at each time point but scores had not recovered by 12 months. The mean sexual bother score had decreased by >50% at 1 month post-surgery and remained low at 12 months.
Mean bowel function decreased slightly at 1 month post-surgery and returned to baseline levels at 3 months (Fig. 1D). Mean bowel function and mean bowel bother showed no significant differences from baseline at any postoperative timepoint.
After a slight decrease at 1 month, mean hormone function increased above baseline at 3 months (Fig. 1E). Mean hormone bother also decreased at 1 month but returned to baseline at 3 months post-surgery. No statistically significant differences in mean hormone function and mean hormone were seen at any postoperative timepoint.
At baseline, there were no significant differences in age, urinary function, urinary bother, sexual function, and sexual bother between the RALP and RRP groups. Repeated-measures ANOVA showed no significant changes over time in terms of urinary function (p=0.078; Fig. 2A), urinary bother (p=0.060; Fig. 2B), or sexual bother (p=0.235; Fig. 2D). However, changes in sexual function over time were significantly different between the two groups (p=0.020; Fig. 2C) and recovery of sexual function was significantly better in the RALP group compared with the RRP group from 3–12 months post-surgery.
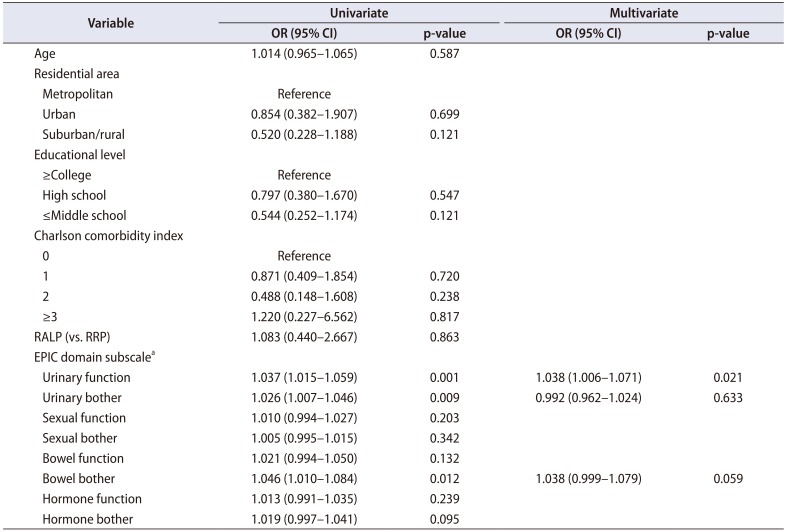
At 1, 3, 6, and 12 months after radical prostatectomy, 68.7%, 65.0%, 64.5%, and 66.3% of patients indicated that they were satisfied with the treatment they had received (Table 2). Multivariate analysis showed that only recovery of urinary function was significantly associated with overall satisfaction 12 months after radical prostatectomy (Table 3).
In this study, Korean patients with prostate cancer reported a more pronounced decline in sexual function and bother after radical prostatectomy, compared with other HRQOL outcomes. However, sexual outcome was not associated with overall satisfaction and an association was seen only with the recovery of urinary function.
Overall, the pattern of change related to each HRQOL domain in this cohort of Korean men was similar to that reported in previous studies [21314151617]. However, some differences were apparent. In comparison with a study of American men with prostate cancer [14], the EPIC sexual function score was approximately twice as high as in our study, recovering to half of the baseline values at 12 months post-surgery. However, in our study, the sexual function score was lower at baseline and recovered to approximately one third of baseline values at 12 months post-surgery, which is similar to Japanese study results [1617].
The most likely cause of the observed differences in sexual outcomes versus Western studies is ethnicity. Namiki et al. [10] investigated sexual function following radical prostatectomy in a prospective longitudinal study of Japanese and American men. In the Namiki et al.'s study [10], Japanese men reported lower sexual function scores at baseline and American men were more likely than Japanese men to regain their baseline sexual function. In this study, the mean baseline sexual function score was lower than that of Western studies [1314]. In a primary care study of Korean men [18], the prevalence of erectile dysfunction was 32.5%, 52.4%, and 68.5% in men aged 40–49, 50–59, and ≥60 years, respectively, which is higher than that seen in other countries, including Japan [1019]. In a sub-analysis of preoperatively potent patients in this study cohort, sexual function and bother increased from 6 months after surgery and reached approximately 80% of baseline at 12 months, a result similar to that seen in the American study (Supplementary Fig). In these preoperatively potent patients, the potency rate at 12 months post-surgery was 53.5%. Moreira et al. [20] reported that only 2% of men in Korea had consulted a doctor about their sexual problems. This is largely due to the belief that the problem is not sufficiently serious and therefore not of significant concern. In Korean men, such perception of sexual problems may have affected their sexual function and recovery after surgery.
HRQOL can be dependent on treatment modality. Because of the difficulties associated with conducting randomized trials, comparing outcomes related to RALP and RRP is challenging and studies have shown mixed results [21222324]. A Cochrane review [25], which is the most recent study on this issue, found no evidence supporting the effectiveness of RALP (in terms of oncological and functional outcome) over RRP. However, men undergoing RALP had shorter hospital stays and lower rates of blood transfusion. Consistent with this, we observed that the mean hospital stay was shorter (8.3 days vs. 11.9 days, p<0.001) and blood transfusion rates lower (2.4% vs. 9.3%, p<0.001) after RALP than after RRP. Although the uptake of RALP in East Asia has been somewhat slower and less widespread than in Western countries, the use of RALP has been steadily increasing over the past decade in East Asia, including Korea [726]. However, to our knowledge, there have been no published studies comparing postoperative longitudinal HRQOL changes in Asian men (including Korean patients) with prostate cancer undergoing RALP and RRP. Our results showed that recovery of sexual function was greater in the RALP group than the RRP group, an observation that is consistent with some previous reports [232427].
Previous studies have shown that 16% to 19% of patients with localized prostate cancer regret their treatment choice [2829]. In these studies, sociodemographic factors and HRQOL outcomes impacted on satisfaction and regret after treatment. Notably, the overall satisfaction rate 12 months after radical prostatectomy in Korean men was 66.2%, which is considerably lower than that reported in the American population [282930]. In the current study, we found that recovery of urinary function was the only influencing factor for overall satisfaction and the notable decline in sexual domain score, sexual function, and bother did not significantly affect overall satisfaction. As described above, perception of sexual problems may have contributed to these results.
We acknowledge several limitations in this study. First, the duration of follow-up was not sufficient to evaluate long-term results and functional outcomes have been reported to change after 2 or more years in several studies [3141516]. In our study cohort, we found that the potency rates of preoperatively potent patients continuously increased from 53.5% at 1 year to 61.8% at 4 years after surgery. Secondly, treatment selection was not randomized and the study population may not be representative of all Korean men undergoing radical prostatectomy. Thirdly, although there were no preoperative differences in age and HRQOL domain scores in the RALP and RRP groups, baseline characteristics could not be fully adjusted. Fourthly, sociodemographic variables were not considered in the analysis of overall satisfaction after surgery. However, we believe the present study to be of value as a prospectively designed, single-surgeon, single-institution series of consecutive cases. Despite the short follow-up period, these data can be considered to be meaningful because changes in HRQOL are most marked during the first year post-surgery. The findings are also valuable in terms of the consistency and quality of the data because the study included only those patients who completed the questionnaire at all timepoints. In addition, to our knowledge, this is the first study to prospectively compare patient-reported HRQOL changes between RALP and RRP in Asian men. Nonetheless, additional multicenter, randomized studies are required to confirm our observations.
In this cohort of Korean men undergoing radical prostatectomy, urinary function and incontinence had not recovered to baseline values at 12 months, whereas urinary bother and irritation/obstruction recovered fully by the end of the study period. Sexual outcomes declined significantly after surgery and did not fully recover.
Recovery of sexual function was significantly better in the patient group who underwent robotic surgery compared with those who underwent open surgery. Only urinary function recovery was significantly associated with overall satisfaction 12 months after radical prostatectomy.
ACKNOWLEDGMENTS
This study is supported by research grants from Astellas Pharma Inc. The authors wish to thank Min-Ju Kim (Department of Clinical Epidemiology and Biostatistics, Asan Medical Center, University of Ulsan College of Medicine) for assistance in statistical evaluation.
References
1. Sanda MG, Dunn RL, Michalski J, Sandler HM, Northouse L, Hembroff L, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med. 2008; 358:1250–1261. PMID: 18354103.

2. Huang GJ, Sadetsky N, Penson DF. Health related quality of life for men treated for localized prostate cancer with long-term followup. J Urol. 2010; 183:2206–2212. PMID: 20399462.

3. Resnick MJ, Koyama T, Fan KH, Albertsen PC, Goodman M, Hamilton AS, et al. Long-term functional outcomes after treatment for localized prostate cancer. N Engl J Med. 2013; 368:436–445. PMID: 23363497.

4. Hamdy FC, Donovan JL. Patient-reported outcomes following treatment for localized prostate cancer: helping decision making for patients and their physicians. JAMA. 2017; 317:1121–1123. PMID: 28324073.
5. Chen RC, Basak R, Meyer AM, Kuo TM, Carpenter WR, Agans RP, et al. Association between choice of radical prostatectomy, external beam radiotherapy, brachytherapy, or active surveillance and patient-reported quality of life among men with localized prostate cancer. JAMA. 2017; 317:1141–1150. PMID: 28324092.

6. Barocas DA, Alvarez J, Resnick MJ, Koyama T, Hoffman KE, Tyson MD, et al. Association between radiation therapy, surgery, or observation for localized prostate cancer and patient-reported outcomes after 3 years. JAMA. 2017; 317:1126–1140. PMID: 28324093.

7. Zhu Y, Wang HK, Qu YY, Ye DW. Prostate cancer in East Asia: evolving trend over the last decade. Asian J Androl. 2015; 17:48–57. PMID: 25080928.

8. Whiting PF, Moore TH, Jameson CM, Davies P, Rowlands MA, Burke M, et al. Symptomatic and quality-of-life outcomes after treatment for clinically localised prostate cancer: a systematic review. BJU Int. 2016; 118:193–204. PMID: 27087414.

9. Boyd LK, Mao X, Lu YJ. The complexity of prostate cancer: genomic alterations and heterogeneity. Nat Rev Urol. 2012; 9:652–664. PMID: 23132303.

10. Namiki S, Kwan L, Kagawa-Singer M, Tochigi T, Ioritani N, Terai A, et al. Sexual function following radical prostatectomy: a prospective longitudinal study of cultural differences between Japanese and American men. Prostate Cancer Prostatic Dis. 2008; 11:298–302. PMID: 17909566.

11. Chung KJ, Kim JJ, Lim SH, Kim TH, Han DH, Lee SW. Development and validation of the Korean version of expanded prostate cancer index composite: questionnaire assessing health-related quality of life after prostate cancer treatment. Korean J Urol. 2010; 51:601–612. PMID: 20856644.

12. Wei JT, Dunn RL, Litwin MS, Sandler HM, Sanda MG. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000; 56:899–905. PMID: 11113727.

13. Wagner AA, Cheng PJ, Carneiro A, Dovirak O, Khosla A, Taylor KN, et al. Clinical use of expanded prostate cancer index composite for clinical practice to assess patient reported prostate cancer quality of life following robot-assisted radical prostatectomy. J Urol. 2017; 197:109–114. PMID: 27475967.

14. Parker WR, Wang R, He C, Wood DP Jr. Five year expanded prostate cancer index composite-based quality of life outcomes after prostatectomy for localized prostate cancer. BJU Int. 2011; 107:585–590. PMID: 20804482.

15. Penson DF, McLerran D, Feng Z, Li L, Albertsen PC, Gilliland FD, et al. 5-year urinary and sexual outcomes after radical prostatectomy: results from the prostate cancer outcomes study. J Urol. 2005; 173:1701–1705. PMID: 15821561.

16. Namiki S, Ishidoya S, Ito A, Kawamura S, Tochigi T, Saito S, et al. Quality of life after radical prostatectomy in Japanese men: a 5-Year follow up study. Int J Urol. 2009; 16:75–81. PMID: 19054169.

17. Namiki S, Kaiho Y, Mitsuzuka K, Saito H, Yamada S, Nakagawa H, et al. Long-term quality of life after radical prostatectomy: 8-year longitudinal study in Japan. Int J Urol. 2014; 21:1220–1226. PMID: 25143229.

18. Cho BL, Kim YS, Choi YS, Hong MH, Seo HG, Lee SY, et al. Prevalence and risk factors for erectile dysfunction in primary care: results of a Korean study. Int J Impot Res. 2003; 15:323–328. PMID: 14562132.
19. Prins J, Blanker MH, Bohnen AM, Thomas S, Bosch JL. Prevalence of erectile dysfunction: a systematic review of population-based studies. Int J Impot Res. 2002; 14:422–432. PMID: 12494273.

20. Moreira ED Jr, Kim SC, Glasser D, Gingell C. Sexual activity, prevalence of sexual problems, and associated help-seeking patterns in men and women aged 40–80 years in Korea: data from the Global Study of Sexual Attitudes and Behaviors (GSSAB). J Sex Med. 2006; 3:201–211. PMID: 16490013.
21. Malcolm JB, Fabrizio MD, Barone BB, Given RW, Lance RS, Lynch DF, et al. Quality of life after open or robotic prostatectomy, cryoablation or brachytherapy for localized prostate cancer. J Urol. 2010; 183:1822–1828. PMID: 20303100.

22. Yaxley JW, Coughlin GD, Chambers SK, Occhipinti S, Samaratunga H, Zajdlewicz L, et al. Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: early outcomes from a randomised controlled phase 3 study. Lancet. 2016; 388:1057–1066. PMID: 27474375.

23. Haglind E, Carlsson S, Stranne J, Wallerstedt A, Wilderäng U, Thorsteinsdottir T, et al. Urinary incontinence and erectile dysfunction after robotic versus open radical prostatectomy: a prospective, controlled, nonrandomised trial. Eur Urol. 2015; 68:216–225. PMID: 25770484.

24. Thompson JE, Egger S, Böhm M, Haynes AM, Matthews J, Rasiah K, et al. Superior quality of life and improved surgical margins are achievable with robotic radical prostatectomy after a long learning curve: a prospective single-surgeon study of 1552 consecutive cases. Eur Urol. 2014; 65:521–531. PMID: 24287319.

25. Ilic D, Evans SM, Allan CA, Jung JH, Murphy D, Frydenberg M. Laparoscopic and robot-assisted vs open radical prostatectomy for the treatment of localized prostate cancer: a Cochrane systematic review. BJU Int. 2018; 121:845–853. PMID: 29063728.

26. Seo HJ, Lee NR, Son SK, Kim DK, Rha KH, Lee SH. Comparison of robot-assisted radical prostatectomy and open radical prostatectomy outcomes: a systematic review and meta-analysis. Yonsei Med J. 2016; 57:1165–1177. PMID: 27401648.

27. Ficarra V, Novara G, Ahlering TE, Costello A, Eastham JA, Graefen M, et al. Systematic review and meta-analysis of studies reporting potency rates after robot-assisted radical prostatectomy. Eur Urol. 2012; 62:418–430. PMID: 22749850.

28. Schroeck FR, Krupski TL, Sun L, Albala DM, Price MM, Polascik TJ, et al. Satisfaction and regret after open retropubic or robot-assisted laparoscopic radical prostatectomy. Eur Urol. 2008; 54:785–793. PMID: 18585849.

29. Kim JH, Ha YS, Jeong SJ, Kim S, Kim WJ, Jang TL, et al. Factors related to patient-perceived satisfaction after robot-assisted radical prostatectomy based on the expanded prostate cancer index composite survey. Prostate Cancer Prostatic Dis. 2013; 16:341–345. PMID: 23917307.

30. Abraham NE, Makarov DV, Laze J, Stefanovics E, Desai R, Lepor H. Patient centered outcomes in prostate cancer treatment: predictors of satisfaction up to 2 years after open radical retropubic prostatectomy. J Urol. 2010; 184:1977–1981. PMID: 20850836.

SUPPLEMENTARY MATERIAL
Scan this QR code to see the supplementary material, or visit https://www.icurology.org/src/sm/icurology-59-313-s001.pdf.

Supplementary Fig
Longitudinal sexual domain scores in preoperatively potent patients.
Fig. 1
Longitudinal health-related quality of life domain scores. (A) Urinary function and bother score. (B) Urinary incontinence and irritation/obstruction score. (C) Sexual function and bother score. (D) Bowel function and bother score. (E) Hormone function and bother score.
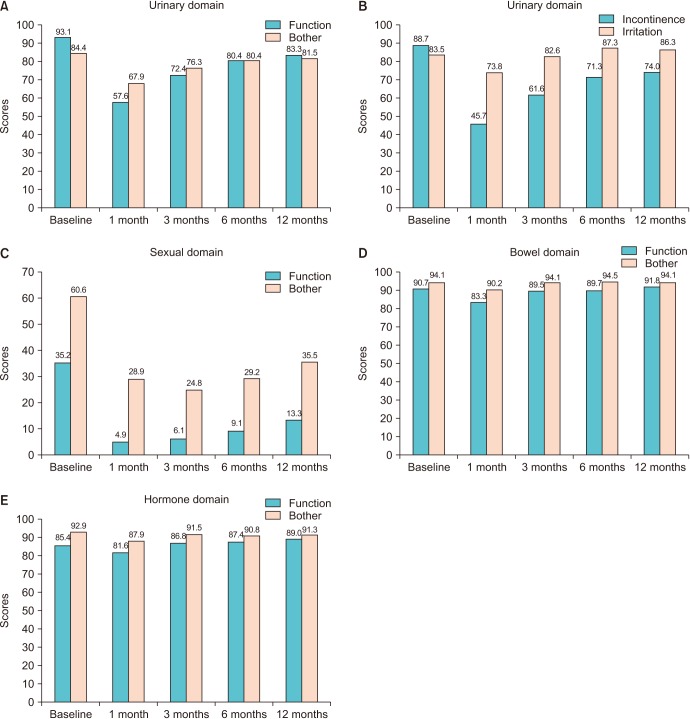
Fig. 2
Comparison of urinary and sexual outcomes between robot-assisted and open radical prostatectomy groups. (A) Urinary function. (B) Urinary bother. (C) Sexual function. (D) Sexual bother. Based on repeated-measures ANOVA. Statistical tests for interaction of surgery group and time. RALP, robot-assisted laparoscopic prostatectomy; RRP, retropubic radical prostatectomy.
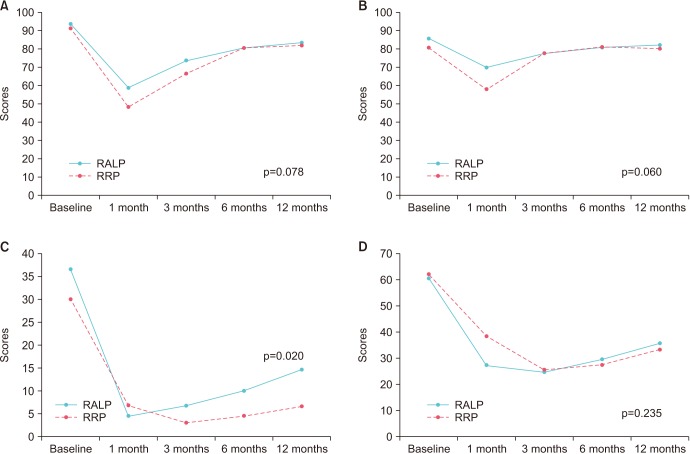
Table 1
Patient characteristics (n=211)
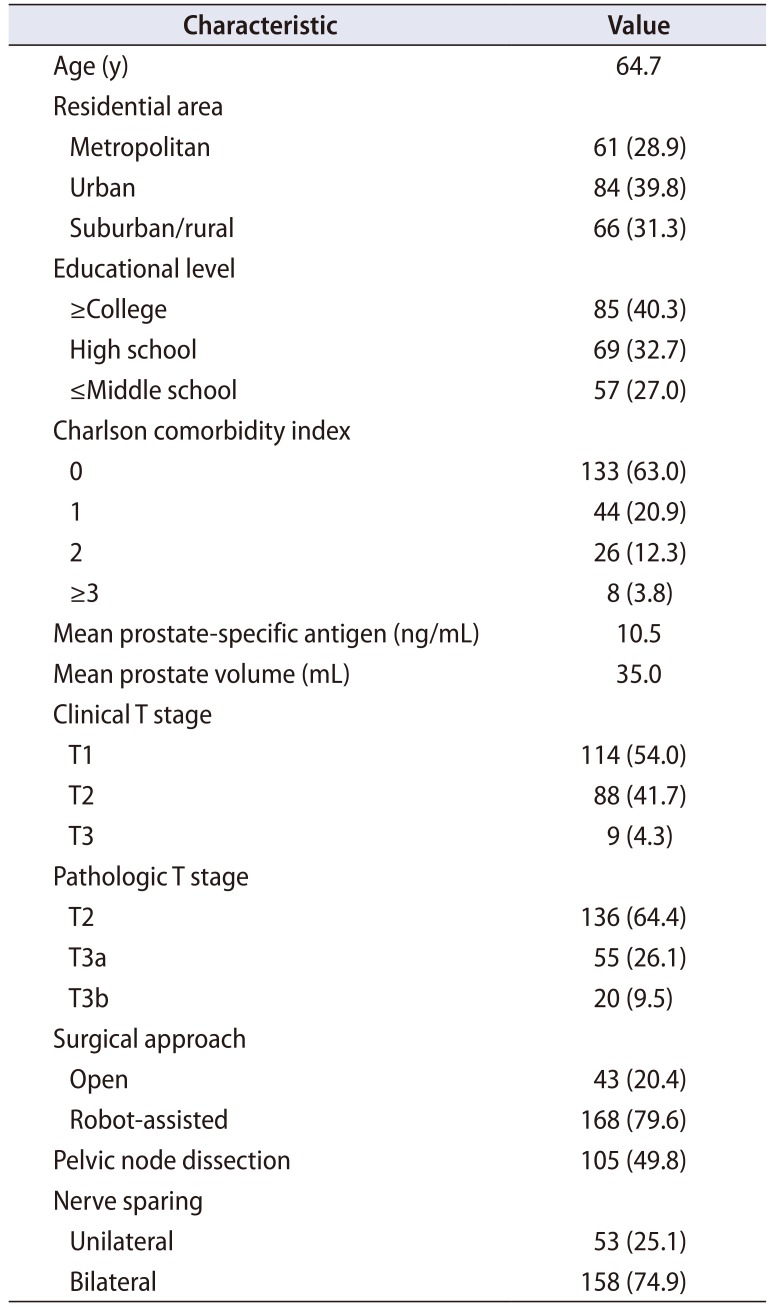
Table 2
Overall satisfaction 12 months after radical prostatectomy
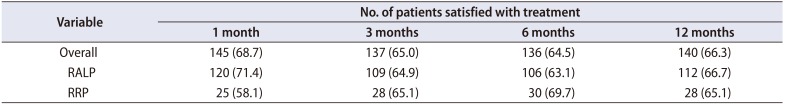
Table 3
Univariable and multivariable logistic regression analyses to identify which EPIC domain subscale changes are associated with overall satisfaction 12 months post-surgery




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download