Abstract
Purpose
Spontaneous gastrointestinal perforations (SGIPs; not associated with injury or disease) occur rarely in pediatric patients. This study aimed to define age-specific features associated with SGIPs in pediatric patients.
Methods
Retrospectively reviewed the clinical data of children (before adolescence) who received surgery due to a SGIP at a single institution. Thirty-nine patients were enrolled. Characteristics were compared between the 2 age groups: neonates (group A) and beyond neonates (group B).
Results
Group A included 24 patients (61.5%) an group B included 15 patients (38.5%). Thirteen perforations occurred in the stomach (33.3%), 12 in the small intestine (30.8%), and 14 in the large intestine (35.9%). A significantly higher proportion of perforations occurred in the stomach and small intestine in group A, while more perforations occurred in the large intestine in group B (P = 0.01). Several associated conditions during the preoperative period were identified in both groups. The overall mortality rate was 15.4% (6 of 39). Mortality was relatively high in group A (5 of 24, 20.8%) and for perforations of stomach (3 of 13, 23.1%) and small intestine (3 of 12, 25.0%); however, there were no significant differences with regard to age or perforation site (P = 0.244, P = 0.122, respectively).
Conclusion
SGIPs in pediatric patients had diverse clinical features and different perforation patterns according to age group. However, no significant group differences in mortality were found. Thus, favorable results regardless of age can be expected with prompt recognition, medical resuscitation, and adequate surgical management.
Gastrointestinal perforations (GIPs) usually occur in association with trauma or disease; however, GIPs may develop spontaneously without any predisposing clinicopathological factors (spontaneous GIPs, SGIPs). In pediatric patients, commonly known etiologic factors responsible for GIPs include congenital gastrointestinal anomalies, blunt trauma, intussusception, iatrogenic injury, foreign body ingestion, and other inflammatory conditions such as appendicitis, typhoid, tuberculosis, Crohn disease, and necrotizing enterocolitis [1234].
The frequency of SGIPs is uncertain, but the incidence appears to be low in the pediatric population. SGIPs are more common at the extremes of age, e specially in premature infants, and rarely occur in older infants and children. In contrast to neonatal GIPs, the literature regarding SGIPs in pediatric patients generally consists of sporadic case reports or small case series [56789]. On the other hand, it seems to imply that SGIPs could manifest age-specific clinical features.
In the present study, we analyzed clinical data from pediatric cases at a single institution, focusing on cases of SGIPs not related to traumatic injury or other inflammatory conditions. Then, compared the clinical features of 2 age groups; neonates and beyond neonates, and attempted to suggest its clinical implications by defining the different features.
We retrospectively reviewed the clinical data of children (before the age of adolescence) who received a treatment due to SGIP between January 2000 and December 2015 at Pusan National University Children's Hospital. Perforations secondary to trauma, intussusception, iatrogenic injury, foreign body ingestion, certain inflammatory conditions (perforated appendicitis, Crohn disease, typhoid, etc.), and necrotizing enterocolitis in premature infants, were excluded. There were 41 patients with SGIPs, but 2 cases had been associated with Hirshsprung disease. Thus, 39 patients were enrolled. This study was approved by Pusan National University Yangsan Hospital Institutional Review Board with informed consent exemption (approval number: 05-2016-165) and the data were managed with personal information protection.
Collected data included patient demographics, anatomical location of the perforation, treatment received, and postoperative outcomes. The data were compared between 2 postnatal age groups: neonates (group A) and beyond neonates (group B). In addition, age was further categorized into 4 classes: neonate (preterm and full-term), infant (age ≤ 24 months), preschool-aged (age ≤ 6 years) and school-aged (age ≤ 12 years) child.
Statistical analyses were performed using IBM SPSS Statistics ver. 23.0 (IBM Co., Armonk, NY, USA). A Fisher exact tests were performed to identify significant associations. A P-value < 0.05 was considered significant.
Of the 39 patients with a SGIP, 24 (61.5%) were in group A and 15 (38.5%) were in group B. Although preterm infants were enrolled in the present study, the other enrolled patients had no health problems before the surgery.
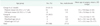
Group A included 16 preterm neonates (mean gestational age, 29.2 ± 3.7 weeks; a mean postnatal age at surgery, 14 ± 19.8 days) and 8 full-term neonates (mean gestational age, 39.2 ± 1.5 weeks; a mean postnatal age at surgery, 5.8 ± 5.0 days). Group B included 8 infants, 4 preschool-age children, and 3 school-age children with a mean age at surgery of 7.5 ± 6.4 months, 36.5 ± 10.1 months, and 117 ± 53.3 months, respectively. The sex ratio (male:female) was 2.25 : 1 (Table 1).
Perforation occurred at any site of gastrointestinal tract: 13 perforations occurred in the stomach (33.3%), 12 occurred in the small intestine (30.8%), and 14 occurred in the large intestine (35.9%). Moreover, the distribution significantly differed according to age; a significantly higher proportion of perforations occurred in the stomach and small intestine in group A compared to that in group B, while a higher proportion occurred in the large intestine in group B compared to that in group A (P = 0.01) (Table 2).
In neonates, especially in those who were preterm, premature rupture of membrane (PROM) was associated with an early birth in 4 patients (16.7%) and the management of a patent ductus arteriosus (PDA), including drug administration (indomethacin or ibuprofen) or ligation, was recognized in 9 patients (37.5%). Beyond the neonatal period, a medical history of admission for the management of a fever or upper respiratory tract infection, and viral gastroenteritis was common, particularly in cases of colon perforation (12 of 15, 80.0%). However, in cases of colon perforation, a serologic marker for bacteria (Salmonella and Clostridium) and virus (Cytomegalovirus and Rotavirus) showed no positive findings and pathology was confirmed as only inflammatory change without definite condition (Table 3).
Primary repair was mainly performed to manage stomach and colon perforations, while a segmental resection was common in the management of small intestinal perforations. In the management of colon perforations, a staged procedure was performed in 4 cases (Table 4).
Mortality occurred in 6 patients (5 in group A and 1 in group B), with an overall mortality rate of 15.4%. In group A, there were 4 mortality cases in preterm and 1 in full-term, they could not recover after operation due to progressively deteriorating clinical situations, such as respiratory distress syndrome (RDS) and septic condition. In group B, there was 1 mortality case due to gastric perforation of school-age boy. He showed a hemodynamically unstable condition with a disseminated intravascular coagulopathy before operation and could not recover after. With regard to perforation site, 3 cases involved perforations in the stomach and 3 involved in the small intestine, but no mortality cases involved in the colon. However, there were no significant differences in mortality between anatomical sites (P = 0.122). With regard to age group, 4 mortality cases were preterm neonates, 1 case was a full-term neonate, and 1 case was a school-age child. There were no significant differences in mortality between age groups (P = 0.244) (Table 5).
GIP is a major medical problem requiring a prompt surgical procedure and occurs in all age groups; however, it is relatively uncommon in infants and children.
GIPs have been well recognized to occur in premature infants with necrotizing enterocolitis or in older infants and children with traumatic injury or inflammatory conditions. The main causes of GIP in pediatric patients include meconium ileus, atresia, volvulus, Meckel diverticulum, necrotizing enterocolitis, appendicitis, intussusception, inflammatory bowel disease, peptic ulcer, other gastrointestinal diseases causing obstruction, foreign body ingestion, iatrogenic injury and trauma [1234]. Moreover, the pattern of causes changed from obstruction, trauma, peptic ulcer to necrotizing enterocolitis, iatrogenic injury, perinatal asphyxia events, and others [10]. However, SGIPs are not associated with these conditions and are usually only described in sporadic case reports.
Distinctive findings in the present study include followings: (1) SGIPs occurred at all age groups of pediatric patients with a higher incidence in neonates and a tendency to decrease in frequency with age. (2) SGIPs occurred at any site of the gastrointestinal tract with a significant difference in the distribution of perforation site according to age; a higher proportion of colon perforation occurred in pediatric patients beyond the neonate. (3) SGIPs did not differ in mortality according to age group or perforation site.
GIPs can occur at any age, but are most common in the neonatal period as a complication of necrotizing enterocolitis [71112]. It may occur in older children as a result of trauma, other inflammatory gastrointestinal problems, or iatrogenic events, etc. [1314]. Similarly, we found that SGIPs occurred at any age, and were more common in neonates (61.5%) than in age groups beyond the neonate (38.5%). Although SGIPs appeared to gradually decrease with age, we could not determine whether age affected the occurrence of a SGIP.
Previous studies have reported that GIPs in infants had been more common in the distal small intestine (especially the ileum) and colon than in the stomach [6715]. However, in the present study SGIPs occurred more frequently in the colon (35.9%) and stomach (33.3%) than in the small intestine (30.8%). Moreover, the SGIP site significantly differed according to age with a higher proportion occurring in the stomach in neonates and a higher proportion occurring in the colon in older infants and children. This difference between age groups cannot be full explained; however, some perioperative conditions may be related to the occurrence of SGIPs. The present study could not demonstrate definite causes leading to perforation. However, preoperative medical conditions could be identified in many cases in both groups (neonates, 57.7%; beyond neonates, 80.0%). Considering associated conditions in the perioperative period, there may have been multiple factors affecting perforations; perinatal stressors such as PROM or PDA management in the neonatal group while febrile disease requiring admission for management beyond the neonatal period. In neonates, certain perinatal conditions causing a hypoxia or a reduced intestinal blood flow likely induced by indomethacin could be related to the development of SGIPs [161718]. In the patient beyond neonate, we speculate that an association existed between colon perforation and the administration of nonsteroidal antiinflammatory drugs (NSAIDs) for fever management. Several studies have reported NSAID-induced colon perforations in pediatric patients and have suggested that increased permeability of the intestine, bacterial-mediated production of toxic free acids, and drug synergism with ischemia of the intestinal wall may be related to colon perforation [192021]. Although determining their relevance in the development of the perforation is difficult, these factors are presumed to affect the occurrence of SGIPs.
A surgical approach is essential in the management of a GIP, and depends on the perforation site and the time of diagnosis. With regard to surgical procedures, there was a tendency to perform simple procedures in the present study. However, this approach was not proper in all cases, and a staged procedure was required in several cases of colon perforation. Nevertheless, when the perforation is recognized earlier, simple procedures are feasible regardless of perforation site. We could not find any severe problems directly associated with the surgical procedure. Therefore, an early diagnosis and prompt surgical management appears to be necessary for favorable clinical courses.
Mortality occurred in 6 cases (15.4%) in the present study, including 5 cases of group A and 1 case of group B. Specifically, mortality cases involved an ileal perforation in 3 preterm neonates, and a gastric perforation in 1 preterm, full-term, school-age child, respectively. A mortality was slightly higher in preterm neonates (25.0%) compared to that in full term neonates (12.5%) and older children beyond neonates (6.7%), whereas the difference were not significant. Similarly, previous studies have reported higher GIP-related mortality in the youngest patients (especially, preterm infants), with no significant differences in mortality for infants older than 2 months of age [67]. In the present study, a mortality was higher in preterm neonates, but the lack of significant differences with regard to age groups may be related to advancements in neonatal intensive care. With regard to the site of perforation, there were again no significant differences in mortality. There are few reports about the comparison on mortality of SGIP with regard to the perforated site, however some studies showed a higher mortality of perforation associated necrotizing enterocolitis and gastric perforation [472223]. Such perforations were associated with generalized sepsis and multiorgan dysfunction, resulting in a high mortality. Although significant improvements in neonatal management have recently occurred, mortality for the preterm infant with a GIP remains relatively high, particularly for those with extremely low birth weight.
The present study has some limitations. One limitation concerns the observational and retrospective nature of the study, which reflected a single center's experience in a restricted region. In addition, this study included premature neonates with isolated intestinal perforations (IIPs) as subjects. Although IIPs have distinct clinical features from necrotizing enterocolitis, some controversy exists. However, considering the rarity of SGIPs in pediatric patients, the present results may help in the management of SGIPs in pediatric patients, despite these limitations. In conclusion, a SGIP, not associated with inflammatory disease or trauma, has diverse clinical features differing according to age group in pediatric patients. Approximately two-thirds of cases occurred during the neonatal period. Moreover, gastric perforations were more frequent in neonates while colon perforations were more frequent in older infant and children. However, no age-related and perforation site-related differences in mortality were found. Therefore, favorable results can be expected regardless of age with prompt recognition, medical resuscitation, and adequate surgical management.
Figures and Tables
References
1. Emanuel B, Zlotnik P, Raffensperger JG. Perforation of the gastrointestinal tract in infancy and childhood. Surg Gynecol Obstet. 1978; 146:926–928.
3. Cruze K, Snyder WH Jr. Acute perforation of the alimentary tract in infancy and childhood. Ann Surg. 1961; 154:93–99.

4. Freeark RJ, Raffensper Ger JG, Condon JB. Pneumoperitoneum in infancy. Surg Gynecol Obstet. 1961; 113:623–630.
5. Chen JC, Chen CC, Liang JT, Huang SF. Spontaneous bowel perforation in infants and young children: a clinicopathologic analysis of pathogenesis. J Pediatr Gastroenterol Nutr. 2000; 30:432–435.

6. Grosfeld JL, Molinari F, Chaet M, Engum SA, West KW, Rescorla FJ, et al. Gastrointestinal perforation and peritonitis in infants and children: experience with 179 cases over ten years. Surgery. 1996; 120:650–655.

8. Yang B, Ni HK. Diagnosis and treatment of spontaneous colonic perforation: analysis of 10 cases. World J Gastroenterol. 2008; 14:4569–4572.

9. Leone RJ Jr, Krasna IH. ‘Spontaneous’ neonatal gastric perforation: is it really spontaneous? J Pediatr Surg. 2000; 35:1066–1069.

10. Saliakellis E, Borrelli O, Thapar N. Paediatric GI emergencies. Best Pract Res Clin Gastroenterol. 2013; 27:799–817.

11. Sakellaris G, Partalis N, Dede O, Alegakis A, Seremeti C, Korakaki E, et al. Gastrointestinal perforations in neonatal period: experience over 10 years. Pediatr Emerg Care. 2012; 28:886–888.
12. Tan CE, Kiely EM, Agrawal M, Brereton RJ, Spitz L. Neonatal gastrointestinal perforation. J Pediatr Surg. 1989; 24:888–892.

13. Fischerauer EE, Zötsch S, Capito C, Bonnard A, Sárközy S, Berndt J, et al. Paediatric and adolescent traumatic gastrointestinal injuries: results of a European multicentre analysis. Acta Paediatr. 2013; 102:977–981.

14. Arslan S, Okur MH, Arslan MS, Aydogdu B, Zeytun H, Basuguy E, et al. Management of gastrointestinal perforation from blunt and penetrating abdominal trauma in children: analysis of 96 patients. Pediatr Surg Int. 2016; 32:1067–1073.

15. Abadir J, Emil S, Nguyen N. Abdominal foregut perforations in children: a 10-year experience. J Pediatr Surg. 2005; 40:1903–1907.

16. Young CM, Kingma SD, Neu J. Ischemia-reperfusion and neonatal intestinal injury. J Pediatr. 2011; 158:2 Suppl. e25–e28.

17. Attridge JT, Clark R, Walker MW, Gordon PV. New insights into spontaneous intestinal perforation using a national data set: (1) SIP is associated with early indomethacin exposure. J Perinatol. 2006; 26:93–99.

18. Sharma R, Hudak ML, Tepas JJ 3rd, Wludyka PS, Teng RJ, Hastings LK, et al. Prenatal or postnatal indomethacin exposure and neonatal gut injury associated with isolated intestinal perforation and necrotizing enterocolitis. J Perinatol. 2010; 30:786–793.

19. Gordon PV, Herman AC, Marcinkiewicz M, Gaston BM, Laubach VE, Aschner JL. A neonatal mouse model of intestinal perforation: investigating the harmful synergism between glucocorticoids and indomethacin. J Pediatr Gastroenterol Nutr. 2007; 45:509–519.

20. Davies NM. Toxicity of nonsteroidal anti-inflammatory drugs in the large intestine. Dis Colon Rectum. 1995; 38:1311–1321.

21. Bjarnason I, Takeuchi K. Intestinal permeability in the pathogenesis of NSAIDinduced enteropathy. J Gastroenterol. 2009; 44:Suppl 19. 23–29.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download