Abstract
Objectives
The number of patients with medication-related osteonecrosis of the jaw (MRONJ) is increasing, but treatment remains controversial. Published papers and systematic reviews have suggested that surgical treatment is effective in patients with MRONJ. The purpose of this study was to determine whether preoperative University of Connecticut Osteonecrosis Numerical Scale (UCONNS), other serologic biomarkers, and size of necrosis are prognostic factors for outcome of surgical treatment in MRONJ.
Materials and Methods
From January 2008 to December 2016, 65 patients diagnosed with MRONJ at the Department of Oral and Maxillofacial Surgery in College of Dentistry, Dankook University who required hospitalization and surgical treatment were investigated. Patient information, systemic factors, and UCONNS were investigated. In addition, several serologic values were examined through blood tests one week before surgery. The size of osteolysis was measured by panoramic view and cone-beam computed tomography in all patients. With this information, multivariate logistic regression analysis with backward elimination was used to examine factors affecting postoperative outcome.
Results
In multivariate logistic analysis, higher UCONNS, higher C-reactive protein (CRP), larger size of osteolysis, and lower serum alkaline phosphate were associated with higher incidence of incomplete recovery after operation. This shows that UCONNS, CRP, serum alkaline phosphate, and size of osteolysis were statistically significant as factors for predicting postoperative prognosis.
Conclusion
This study demonstrated that CRP, UCONNS, serum alkaline phosphate, and size of osteolysis were statistically significant factors in predicting the prognosis of surgical outcome of MRONJ. Among these factors, UCONNS can predict the prognosis of MRONJ surgery as a scale that includes various influencing factors, and UCONNS should be used first as a predictor. More aggressive surgical treatment and more definite surgical margins are needed when the prognosis is poor.
Bisphosphonates (BPs) are used to treat steroid-induced osteoporosis, Paget's disease of bone, hypercalcemia of malignancy, multiple myeloma, and bone metastases associated with breast, prostate, lung, and other soft tissue tumors1. BP 1-hydroxy ethylidene-1,1 bisphosphonic acid was successfully synthesized for the first time in 1897 by Von Baeyer and Hoffmann and contributed to tremendous development in medicine2. Bisphosphonate-related osteonecrosis of the jaw (BRONJ) was introduced for the first time by Marx3 in 2003. Since then, case reports of BRONJ have gradually increased. Denosumab (Dmab) has also been shown to increase the risk of osteonecrosis4. Thus, the term BRONJ was replaced by “medication-related osteonecrosis of the jaw” (MRONJ) by the American Association of Oral and Maxillofacial Surgeons (AAOMS) position paper in 20145. The following are definitions of MRONJ: (1) current or previous treatment with antiresorptive or antiangiogenic agents; (2) exposed bone or bone that can be probed through an intraoral or extraoral fistula in the maxillofacial region that has persisted for longer than 8 weeks; and (3) no history of radiation therapy to the jaw or obvious metastatic disease to the jaw.
Treatment for MRONJ remains controversial. No agreement has been reached on whether to choose conservative or surgical treatment for MRONJ. Many papers have pointed out limitations of surgical treatment and advocated conservative treatment678. Japan's 2010 position paper recommended non-surgical treatment, and most patients with MRONJ in Japan have received conservative treatment9. Likewise, the 2014 AAOMS position paper also recommended conservative treatment5. However, the disadvantage of conservative treatment is that necrotic bone does not spontaneously resolve, and patient quality of life deteriorates with continued drug treatment10. Recently published papers and systematic reviews have suggested that surgical treatment is more effective in patients with MRONJ1112. In addition, early surgical intervention with adequate resection of necrotic areas and primary closure has also been recommended because it can result in more successful outcomes1112. In other papers, surgical treatment in patients who were taking either a small or large amount of antiresorptive agent showed higher percentages of complete healing than those who received conservative treatment10.
Although studies have suggested that surgical treatment is a more effective treatment for MRONJ than conservative treatment, some patients still have relapses or failures that require continuous treatment. To date, most studies of prognostic factors have been conducted on systemic diseases (such as diabetes mellitus and malignant tumors), BP dosage, route of administration, duration of discontinuation, and bone response factors (such as C-terminal telopeptide and bone-specific alkaline phosphatase)10131415. However, few studies have been conducted on serologic factors commonly performed in surgical patients. Recently, University of Connecticut Osteonecrosis Numerical Scale (UCONNS) has been suggested as a possible prognostic factor in patients with MRONJ16. Therefore, the objective of this study was to determine whether preoperative UCONNS, other serologic biomarkers, and size of osteolysis are prognostic factors for outcome of surgical treatment in MRONJ.
From January 2008 to December 2016, 65 patients diagnosed with MRONJ at the Department of Oral and Maxillofacial Surgery in College of Dentistry, Dankook University (Cheonan, Korea) who required hospitalization and surgical treatment were investigated. A total of 52 patients were investigated after excluding 13 patients with follow-up time less than three months, no blood test or medication, or history of radiotherapy.
1) Patient information including age, sex, site of MRONJ (maxilla, mandible), size of osteolysis, triggering event of MRONJ (tooth extraction, denture, etc.), administration method (intravenous [IV]/per os), type of medicine (BP or Dmab), dosage (low-dose, high dose), duration of administration, surgery method, preoperative stage of MRONJ, and postoperative stage of MRONJ were investigated5. Based on this information, UCONNS score was measured as a prognostic score16. High-dose administration was defined as IV BP used to treat malignant diseases, while low-dose administration was defined as oral BP for osteoporosis or other diseases.
2) General factors including medical history (hypertension, diabetes mellitus, rheumatic arthritis, malignancy, etc.) co-medication (steroids), BP treatment, smoking, and serum biomarkers such as C-reactive protein (CRP), white blood cell (WBC), serum albumin (ALB), serum alkaline phosphate (ALP), platelet (PT), hemoglobin (Hb), and total cholesterol (CHL) were investigated.
3) Radiologic features: All patients underwent orthopantomography (panoramic view) and computed tomography (CT).
4) Histopathologic features: All patients underwent histopathologic analysis. Results were obtained for the following:
Surgery was performed under general anesthesia (curettage, saucerization, sequestrectomy, maxillectomy, marginal mandibulectomy). Preoperative and postoperative AAOMS staging were compared. Results were divided into four groups as follows16:
(1) Absent osteonecrosis of the jaw (ONJ) lesion (postoperative stage 0): intact mucosa, no pain, no inflammation after surgery for at least 3 months;
(2) Reduced ONJ lesion (preoperative stage > postoperative stage): partially exposed bone without inflammation for at least 3 months;
(3) Unchanged ONJ lesion (preoperative stage > postoperative stage): no significant improvement in local findings at follow-up;
(4) Increased ONJ lesion (preoperative stage > postoperative stage): disease progression despite surgical intervention.
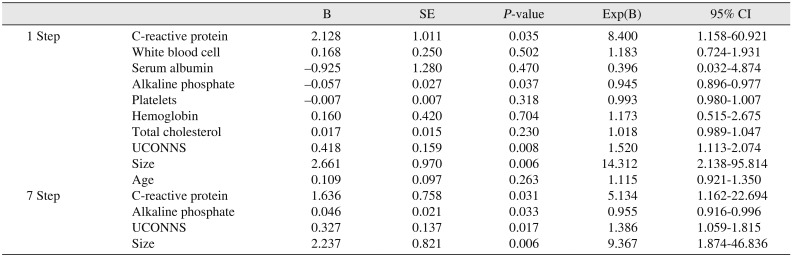
Among these four groups, those without ONJ lesions were classified as the complete healing group. The remaining cases (reduced ONJ, unchanged ONJ, and increased ONJ lesions) were then classified as the incomplete healing group. After assigning patients into one of two groups, serum biomarkers (CRP, WBC, serum ALB, serum ALP, PT, Hb, and total CHL), UCONNS1 (Table 1)1, and extent of osteolysis were evaluated as possible prognostic factors for outcome of surgical treatment for MRONJ by multivariate logistic regression analysis. After multivariate logistic regression analysis, Student's t-test was used to determine difference in mean value between the complete healing group and incomplete healing group.
Statistical analysis was performed using IBM SPSS Statistics ver. 21 (IBM Co., Armonk, NY, USA). First, multivariate logistic regression analysis with backward elimination was used to find significant independent variables. Hosmer-Lemeshow test method and the full model coefficient test were then used to confirm the significance of the chosen independent variables. Student's t-test was used to determine the statistical significance of mean values for each of the significant variants. In all analyses except the Hosmer-Lemeshow test method, statistical significance was considered at P<0.05. In the Hosmer-Lemeshow test, P>0.05 indicated good calibration.
Patients with MRONJ underwent periodic screening for at least three months and up to 90 months after surgery (mean, 19.34 months). The mean duration of BP administration was 51 months (range, 1 to 20 years). In cases with comorbidity and co-medication, most patients suffered from one to three general diseases, including cardiovascular disease and metabolic disease. Regarding patients with underlining malignant disease, three patients (5.8%) had breast cancer and three patients (5.8%) had prostate cancer. The other 46 patients were taking BPs for osteoporosis.
The most common local factor causing MRONJ was tooth extraction (n=41, 78.8%), followed by denture-pressure ulcer (n=3, 5.8%), dental implant (n=3, 5.8%), odontogenic infection (n=4, 7.7%), and periodontal treatment (n=1, 1.9%).
All patients underwent orthopantomogram and CT. The extent of osteolysis was confirmed by CT. A total of 32 patients showed osteolysis in less than 1/3 of the jawbone, while 20 patients showed osteolysis in more than 1/3 but less than 1/2 of the jawbone.
The most common MRONJ location was mandible only (n=34, 65.4%), followed by maxilla only (n=16, 30.8%) and then both mandible and maxilla (n=2, 3.8%).
Treatment results for 52 patients are shown in Table 2. There were 33 patients (63.5%) with absent ONJ lesion, 12 patients (23.1%) with reduced ONJ lesion, 4 patients (7.7%) with unchanged ONJ lesion, and 3 patients (5.8%) with increased ONJ lesion. Total healing occurred in 33 patients (63.5%), while incomplete healing occurred in 19 patients (36.5%).
The mean value±standard deviation (SD) of UCONNS used as a predictor of MRONJ was 13.15±3.17, which was categorized as the moderate ONJ risk group of UCONNS. The minimum value of UCONNS was 10, while the maximum value was 23. In patients with benign disease (n=45), the mean±SD value of UCONNS at 12.29±1.80476) indicated moderate ONJ risk. In patients with malignant disease undergoing IV therapy (n=5), the mean±SD UCONNS value of 18.57±4.42 indicated significant ONJ risk.
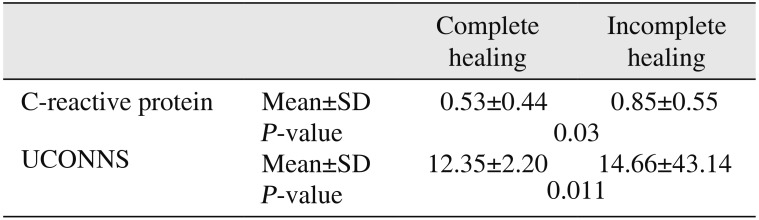
CRP, WBC, serum ALB, serum ALP, PTs, Hb, total CHL, UCONNS, and size of osteolysis were used as variables in multivariate logistic regression analysis with backward elimination, where independent variables were removed at each step. With the full model coefficient test (Table 3) and Hosmer-Lemeshow test (Table 4), the 7th step showed the most appropriate and significant model. This model also showed a predictive power of 82.7%. In the 7th step, the following variables remained statistically significant (P<0.05): CRP, UCONNS, ALP, and size of osteolysis.(Table 5) After multivariate logistic analysis, Student's t-test showed that mean differences in CRP and UCONNS were statistically significant between the complete healing group and incomplete healing group.(Table 6)
The incidence of MRONJ is increasing due to the high risk of infection by resident bacteria in the oral cavity and frequent surgical operations such as extraction. However, treatment for MRONJ remains controversial7171819. In recent years, many papers have demonstrated the effectiveness of surgical methods for MRONJ. Some systemic review papers have compared surgical methods with non-surgical methods and showed better outcomes after surgical treatment202122. In addition, early surgery with single radical treatment has been shown to be better than several less invasive surgical interventions12. Although many published papers have demonstrated the effectiveness of surgical methods, there is still a lack of research on factors that predict postoperative outcomes for MRONJ.
Many studies have shown that more complications (such as diabetes and steroids)152324, longer BP administration period62526, and higher BP dose2728 are associated with MRONJ. However, few studies have determined factors that predict postoperative outcomes for MRONJ. In this study, UCONNS and all possible factors were evaluated by multivariate logistic regression analysis. Serum biomarkers and size of osteolysis were also evaluated.
In this study, 33 of 52 patients with MRONJ showed complete healing. Multivariate logistic regression analysis showed that higher CRP, lower ALP, higher UCONNS value, and larger size of osteolysis were associated with higher chance of incomplete healing.
UCONNS is a numerical scale that includes all conditions related to MRONJ, including systemic diseases, dose, method, duration, applied trauma, and oral status1. The present study is the first to perform multivariate logistic regression analysis of UCONNS with other independent variables.
CRP, ALP, and size of osteolysis also showed statistical significance as factors predicting postoperative outcomes for MRONJ (P-values of 0.031, 0.033, and 0.006, respectively). The odds ratios of CRP, ALP, UCONNS, and size of osteolysis were 5.134, 0.955, 1.386, and 9.367, respectively. This indicates that, as CRP increases by one, the probability of incomplete recovery increases by 5.134 times. The probability of incomplete recovery is 9.367 times higher when the size of osteolysis operation ranges from 1/3 to 1/2 of the jaw compared to 1/3 of the jaw or less.
Among WBC and CRP evaluated for inflammation, only CRP was statistically significant. A previous report has shown that CRP is significantly higher in patients with MRONJ than in control patients29. Among patients with MRONJ in this study, there were statistically significant differences of CRP in postoperative results. This is related to a previous study showing that increased inflammatory markers can indicate the degree of infection at the site of osteonecrosis30. According to Coxon et al.31, bacterial infections appear at sites where soft tissues are opened due to soft tissue toxicity caused by BP, which can increase the level of inflammatory markers.
The size of osteolysis used to evaluate the extent of surgery also showed statistical significance, similar to results of a previous study12. However, there was a limitation in that the size of osteolysis was classified into just two categories. Therefore, more systematic classification is needed in the future.
ALP used to assess bone activity was statistically significant (P=0.033). Serum ALB, total CHL, PTs, or Hb used to evaluate the reduced blood supply caused by BP showed no significant differences.
Student's t-test showed that mean differences in CRP and UCONNS were significantly different between the complete healing group and the incomplete healing group. The mean CRP of the complete healing group was 0.53 mg/dL, which is nearly the normal value of CRP (0–0.5 mg/dL). Mean CRP was 0.85 mg/dL in the incomplete healing group. The mean UCONNS value of the complete recovery group was 12.35, which is categorized as moderate. In the incomplete healing group, the mean UCONNS value was 14.66, which is also categorized as moderate.(Table 1)1
In this study, the incidence of MRONJ (n=34, 65.4% in the mandible; n=16, 30.8% in the maxilla; and n=2, 3.8% in both mandible and maxilla) was similar to that reported in other papers. This might be because the soft tissue is thinner and there is less vascular distribution in the mandible than in the maxilla.
The success rate of complete healing was 63.46%, lower than that reported in other papers (50%–76.7%)10122632. This might be due to the definition of complete healing. In the present study, cases with postoperative infection, bone exposure, or abnormal reactions were excluded. In addition, since the surgical treatment used in this study was mostly saucerization and sequestrectomy, it is possible that the safety margin was not sufficient to include MRONJ. In some papers, major surgery has been reported as more effective for patients with MRONJ than minimally invasive surgery10. In this study, necrotic bone was removed during surgical treatment, and the surgical range was set until fresh blood emerged from the surrounding bone. However, the extent of this surgery is still controversial. Pautke et al.33 have advocated fluorescenceguided resection. Carlson and Basile34 have asserted that a safety margin of 1 cm should be established.
This study has several limitations. First, the sample size is relatively small because this is a retrospective study conducted at a single institution. Furthermore, this is the first study to use UCONNS as a factor for multivariate logistic analysis. Therefore, more studies of UCONNS are needed. These preliminary data are promising, but larger, long-term studies are needed to better define the role of UCONNS and other factors as prognostic factors for MRONJ.
This study demonstrated that CRP, UCONNS, serum ALP, and size of osteolysis were statistically significant factors in predicting the prognosis of 52 patients with MRONJ who underwent surgery. Among these factors, UCONNS can help to predict the prognosis of MRONJ surgery with a scale including various influencing factors, and it should be used as a predictor first. Multivariate logistic regression analysis showed that higher CRP was associated with lower serum alkaline phosphate, higher UCONNS, larger size of osteolysis, and higher chance of incomplete healing. These variables indicate poor prognosis, and more aggressive surgical treatment and a definite surgical margin are needed.
Notes
References
1. Landesberg R, Woo V, Cremers S, Cozin M, Marolt D, Vunjak-Novakovic G, et al. Potential pathophysiological mechanisms in osteonecrosis of the jaw. Ann N Y Acad Sci. 2011; 1218:62–79. PMID: 21291478.

2. Francis MD, Valent DJ. Historical perspectives on the clinical development of bisphosphonates in the treatment of bone diseases. J Musculoskelet Neuronal Interact. 2007; 7:2–8. PMID: 17396000.
3. Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003; 61:1115–1117. PMID: 12966493.

4. Taylor KH, Middlefell LS, Mizen KD. Osteonecrosis of the jaws induced by anti-RANK ligand therapy. Br J Oral Maxillofac Surg. 2010; 48:221–223. PMID: 19836866.

5. Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw--2014 update. J Oral Maxillofac Surg. 2014; 72:1938–1956. PMID: 25234529.

6. Badros A, Weikel D, Salama A, Goloubeva O, Schneider A, Rapoport A, et al. Osteonecrosis of the jaw in multiple myeloma patients: clinical features and risk factors. J Clin Oncol. 2006; 24:945–952. PMID: 16484704.

7. Marx RE, Sawatari Y, Fortin M, Broumand V. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg. 2005; 63:1567–1575. PMID: 16243172.

8. Migliorati CA, Schubert MM, Peterson DE, Seneda LM. Bisphosphonate-associated osteonecrosis of mandibular and maxillary bone: an emerging oral complication of supportive cancer therapy. Cancer. 2005; 104:83–93. PMID: 15929121.
9. Yoneda T, Hagino H, Sugimoto T, Ohta H, Takahashi S, Soen S, et al. Bisphosphonate-related osteonecrosis of the jaw: position paper from the allied task force committee of Japanese Society for Bone and Mineral Research, Japan Osteoporosis Society, Japanese Society of Periodontology, Japanese Society for Oral and Maxillofacial Radiology, and Japanese Society of Oral and Maxillofacial Surgeons. J Bone Miner Metab. 2010; 28:365–383. PMID: 20333419.

10. Hayashida S, Soutome S, Yanamoto S, Fujita S, Hasegawa T, Komori T, et al. Evaluation of the treatment strategies for medication-related osteonecrosis of the jaws (MRONJ) and the factors affecting treatment outcome: a multicenter retrospective study with propensity score matching analysis. J Bone Miner Res. 2017; 32:2022–2029. PMID: 28585700.

11. Allen MR, Ruggiero SL. A review of pharmaceutical agents and oral bone health: how osteonecrosis of the jaw has affected the field. Int J Oral Maxillofac Implants. 2014; 29:e45–e57. PMID: 24451887.

12. Mücke T, Koschinski J, Deppe H, Wagenpfeil S, Pautke C, Mitchell DA, et al. Outcome of treatment and parameters influencing recurrence in patients with bisphosphonate-related osteonecrosis of the jaws. J Cancer Res Clin Oncol. 2011; 137:907–913. PMID: 20927569.

13. Watters AL, Hansen HJ, Williams T, Chou JF, Riedel E, Halpern J, et al. Intravenous bisphosphonate-related osteonecrosis of the jaw: long-term follow-up of 109 patients. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 115:192–200. PMID: 23036797.

14. Kim JW, Kong KA, Kim SJ, Choi SK, Cha IH, Kim MR. Prospective biomarker evaluation in patients with osteonecrosis of the jaw who received bisphosphonates. Bone. 2013; 57:201–205. PMID: 23954759.

15. Molcho S, Peer A, Berg T, Futerman B, Khamaisi M. Diabetes microvascular disease and the risk for bisphosphonate-related osteonecrosis of the jaw: a single center study. J Clin Endocrinol Metab. 2013; 98:E1807–E1812. PMID: 24037883.

16. Reich W, Bilkenroth U, Schubert J, Wickenhauser C, Eckert AW. Surgical treatment of bisphosphonate-associated osteonecrosis: prognostic score and long-term results. J Craniomaxillofac Surg. 2015; 43:1809–1822. PMID: 26321065.

17. Lerman MA, Xie W, Treister NS, Richardson PG, Weller EA, Woo SB. Conservative management of bisphosphonate-related osteonecrosis of the jaws: staging and treatment outcomes. Oral Oncol. 2013; 49:977–983. PMID: 23830962.

18. Lazarovici TS, Yahalom R, Taicher S, Elad S, Hardan I, Yarom N. Bisphosphonate-related osteonecrosis of the jaws: a single-center study of 101 patients. J Oral Maxillofac Surg. 2009; 67:850–855. PMID: 19304045.

19. Kim HY, Lee SJ, Kim SM, Myoung H, Hwang SJ, Choi JY, et al. Extensive surgical procedures result in better treatment outcomes for bisphosphonate-related osteonecrosis of the jaw in patients with osteoporosis. J Oral Maxillofac Surg. 2017; 75:1404–1413. PMID: 28039736.

20. Rupel K, Ottaviani G, Gobbo M, Contardo L, Tirelli G, Vescovi P, et al. A systematic review of therapeutical approaches in bisphosphonates-related osteonecrosis of the jaw (BRONJ). Oral Oncol. 2014; 50:1049–1057. PMID: 25240948.

21. Fliefel R, Tröltzsch M, Kühnisch J, Ehrenfeld M, Otto S. Treatment strategies and outcomes of bisphosphonate-related osteonecrosis of the jaw (BRONJ) with characterization of patients: a systematic review. Int J Oral Maxillofac Surg. 2015; 44:568–585. PMID: 25726090.

22. Khan AA, Morrison A, Hanley DA, Felsenberg D, McCauley LK, O'Ryan F, et al. Diagnosis and management of osteonecrosis of the jaw: a systematic review and international consensus. J Bone Miner Res. 2015; 30:3–23. PMID: 25414052.

23. Jang HW, Kim JW, Cha IH. Development of animal model for bisphosphonates-related osteonecrosis of the jaw (BRONJ). Maxillofac Plast Reconstr Surg. 2015; 37:18. PMID: 26217648.

24. Wutzl A, Eisenmenger G, Hoffmann M, Czerny C, Moser D, Pietschmann P, et al. Osteonecrosis of the jaws and bisphosphonate treatment in cancer patients. Wien Klin Wochenschr. 2006; 118:473–478. PMID: 16957978.

25. Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 2004; 62:527–534. PMID: 15122554.

26. Abu-Id MH, Açil Y, Gottschalk J, Kreusch T. [Bisphosphonateassociated osteonecrosis of the jaw]. Mund Kiefer Gesichtschir. 2006; 10:73–81. German. PMID: 16456688.
27. Vahtsevanos K, Kyrgidis A, Verrou E, Katodritou E, Triaridis S, Andreadis CG, et al. Longitudinal cohort study of risk factors in cancer patients of bisphosphonate-related osteonecrosis of the jaw. J Clin Oncol. 2009; 27:5356–5362. PMID: 19805682.

28. Choi WS, Lee JI, Yoon HJ, Min CK, Lee SH. Medication-related osteonecrosis of the jaw: a preliminary retrospective study of 130 patients with multiple myeloma. Maxillofac Plast Reconstr Surg. 2017; 39:1. PMID: 28101496.

29. Choi SY, An CH, Kim SY, Kwon TG. Bone turnover and inflammatory markers of bisphosphonate-related osteonecrosis of the jaw in female osteoporosis patients. J Oral Maxillofac Surg Med Pathol. 2013; 25:123–128.

30. Lesclous P, Abi Najm S, Carrel JP, Baroukh B, Lombardi T, Willi JP, et al. Bisphosphonate-associated osteonecrosis of the jaw: a key role of inflammation? Bone. 2009; 45:843–852. PMID: 19631301.

31. Coxon FP, Thompson K, Roelofs AJ, Ebetino FH, Rogers MJ. Visualizing mineral binding and uptake of bisphosphonate by osteoclasts and non-resorbing cells. Bone. 2008; 42:848–860. PMID: 18325866.

32. Boonyapakorn T, Schirmer I, Reichart PA, Sturm I, Massenkeil G. Bisphosphonate-induced osteonecrosis of the jaws: prospective study of 80 patients with multiple myeloma and other malignancies. Oral Oncol. 2008; 44:857–869. PMID: 18282788.

33. Pautke C, Bauer F, Otto S, Tischer T, Steiner T, Weitz J, et al. Fluorescence-guided bone resection in bisphosphonate-related osteonecrosis of the jaws: first clinical results of a prospective pilot study. J Oral Maxillofac Surg. 2011; 69:84–91. PMID: 20971542.

34. Carlson ER, Basile JD. The role of surgical resection in the management of bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg. 2009; 67(5 Suppl):85–95. PMID: 19371819.

Table 1
University of Connecticut Osteonecrosis Numerical Scale1
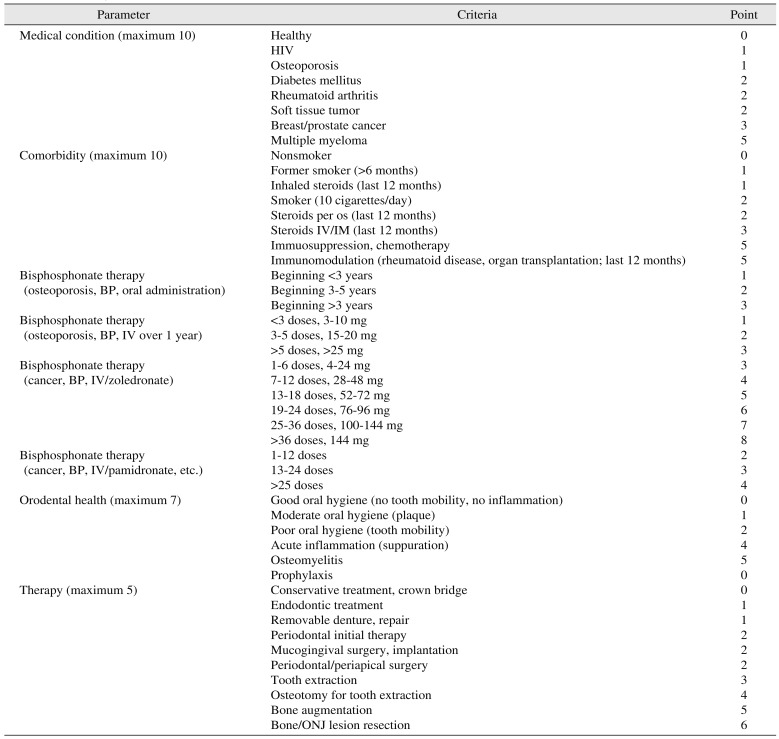
(HIV: human immunodeficiency virus, IV: intravenous, IM: intramuscular, BP: bisphosphonate, ONJ: osteonecrosis of the jaw)
Risk assessment: minimal ONJ risk, <10; moderate ONJ risk, 10–15; significant ONJ risk, >15.
Revised from the article of Landesberg et al. (Ann N Y Acad Sci 2011;1218:62-79)1.
Table 2
Treatment outcomes of medication-related ONJ
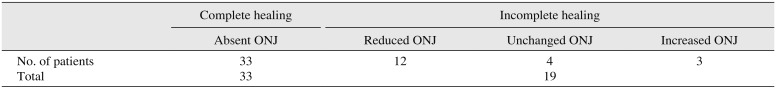
| Complete healing | Incomplete healing | |||
|---|---|---|---|---|
| Absent ONJ | Reduced ONJ | Unchanged ONJ | Increased ONJ | |
| No. of patients | 33 | 12 | 4 | 3 |
| Total | 33 | 19 | ||
Table 3
Full model coefficient test
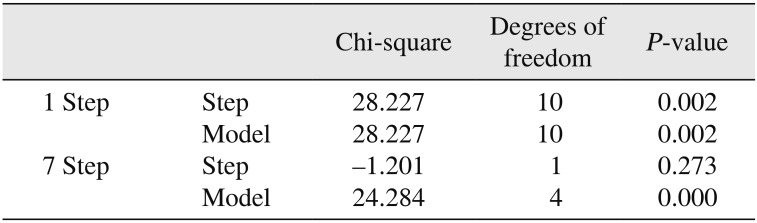
| Chi-square | Degrees of freedom | P-value | ||
|---|---|---|---|---|
| 1 Step | Step | 28.227 | 10 | 0.002 |
| Model | 28.227 | 10 | 0.002 | |
| 7 Step | Step | −1.201 | 1 | 0.273 |
| Model | 24.284 | 4 | 0.000 | |
Table 4
Hosmer-Lemeshow test method
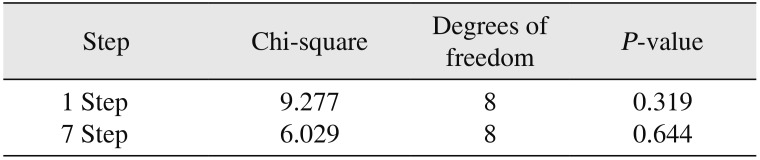
| Step | Chi-square | Degrees of freedom | P-value |
|---|---|---|---|
| 1 Step | 9.277 | 8 | 0.319 |
| 7 Step | 6.029 | 8 | 0.644 |
Table 5
Multivariate analysis of variables relating to incomplete healing in 55 original patients




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download