Abstract
A ‘collision’ tumor refers to the existence of two different neoplasms within the same tumor. Sometimes, the term ‘biphasic tumor’ is also used. However, a ‘collision’ tumor is defined as the occurrence of two neoplasms within proximity of each other yet maintaining distinctly defined, separate boundaries. In contrast, a ‘biphasic’ tumor demonstrates two or more phenotypically distinct neoplastic cell populations merging within the same space. Here, we report a case of collision tumor associated with sarcomatoid eccrine porocarcinoma and basal cell carcinoma arising in a 57-year-old male patient.
Cutaneous biphasic sarcomatoid carcinoma is a rare malignancy that shows both an epithelial and a mesenchymal component. The epithelial component may include basal cell carcinoma, squamous cell carcinoma, and malignant adnexal tumor, whereas the mesenchymal component may comprise poorly differentiated spindle cells, along with heterologous elements, such as chondroblastic and osteoblastic differentiation123. To the best of our knowledge, this is the sixth report of sarcomatoid eccrine porocarcinoma (SEP) in the skin234 and the first report of collision tumor associated with SEP and basal cell carcinoma. We present a case of a 57-year-old male patient with characteristic features of SEP, combined with basal cell carcinoma, which was successfully managed through performing a wide local excision and a split-thickness skin graft.
A 57-year-old male presented at our hospital with an ulcerated, beefy red nodule, with adjacent pinhead to bean-sized multiple nevi in the right zygoma (Fig. 1A). The pruritic, erythematous lesion had been present for a long time and the lesion was reported to have rapidly increased in size over the previous four weeks, prior to the hospital visit. Further examination revealed an ill-defined, rice grain-sized, eroding deep brown patch in the superior portion of the nasal bridge, between the eyes (Fig. 1B). The patient worked as a street vendor, and a history of high skin-sun exposure was noted. Clinically, the lesion in the zygoma was suspected to be a squamous cell carcinoma and the lesion between the eyes suspected to be a basal cell carcinoma. Local biopsy, with provisional diagnosis and subsequent wide local excision and split-thickness skin graft, was performed. In the right zygoma, a relatively well circumscribed hypercellular tumor, which occupied the dermis down to the subcutaneous fat layer, with surface ulceration was seen (Fig. 2A). There was no benign eccrine poromatous lesions. Glandular architecture similar to eccrine glands was merged with poorly differentiated, haphazardly arranged spindle cells (Fig. 2B) showing moderate nuclear pleomorphism and numerous mitoses, including atypical mitoses (Fig. 2C). Nests of basaloid cells with peripheral nuclear palisading were noted in the upper dermis (Fig. 2D). Poorly differentiated tumor cells from the SEP diffusely expressed cytokeratin (Fig. 3A), p63 (Fig. 3B), and vimentin (Fig. 3C). Carcinoembryonic antigen (CEA) (Fig. 3D) and epithelial membrane antigen (EMA) (Fig. 3E) were positive in gland forming cells, which were negative for vimentin. Ductal cells are highlighted by special stain periodic acid-Schiff (PAS)/diastase-resistant PAS (Fig. 3F). Basaloid cells expressed cytokeratin and p63, and were negative for vimentin and CEA. The study was approved by the Institutional Review Board of the Inje University Busan Paik Hospital (IRB no. 17-0029). We received the patient's consent form about publishing all photographic materials.
Eccrine porocarcinomas (EP) may arise de novo or resulting from a malignant transformation of long-standing benign counterparts including poroma, hydroacanthoma simplex, or in association with sebaceous nevi1. It is recognized that eccrine porocarcinoma can possibly have various histologic features, such as mature duct formation, intracytoplasmic lumina, benign components, necrosis, a Bowenoid pattern, clear cell change, squamous differentiation, spindle cell change, and mucin-containing cells2. Prior to a direct description of SEP, Perna et al.2 reported 3 cases of EPs that showed only focal spindle cell differentiation, with nuclear morphology appearing similar to that of the adjacent epithelioid tumor cells. In 2007, Goh et al.3 reported two cases of sarcomatoid carcinomas, which were undifferentiated, with pseudo-angiosarcomatous change to the morphologic spectrum of eccrine porocarcinoma. In one of them, the tumor was composed predominantly of compact fascicles of malignant spindle cells and of focal malignant ductal differentiation. They coined the term ‘sarcomatoid eccrine porocarcinoma’ (SEP). It is an extremely rare tumor, and to the best of our knowledge, this is the sixth report of SEP in the skin234.
SEP is a sweat gland tumor, which is characterized by predominant spindle cells with ductal differentiation. Unfortunately, when the tumor is poorly differentiated, malignant tumors may not show obvious duct formation and that makes it difficult to distinguish SEP from spindle cell squamous cell carcinoma or carcinosarcoma. However, spindle cell squamous cell carcinomas are commonly composed entirely of pleomorphic spindle cells without epidermal components or squamous differentiation. Furthermore, actinic keratosis, or an epithelial-to-spindle cell transitional area, or an intercellular bridge could be helpful to distinguish them from SEPs. Identifying the glandular components among the spindle cell lesion is the most important factor in diagnosing SEP. Sometimes using immunohistochemical markers can be helpful to confirm diagnosis with a high index of certainty.
Owing to the biphasic nature of both epithelial and mesenchymal components, it is necessary to differentiate SEPs from carcinosarcomas, which are frequently reported in the female genital tract among diverse anatomical sites. Kwan and Satter5 reported that primary cutaneous carcinosarcoma has both malignant mesenchymal and epithelial components, in varying proportions, with no transition between them. Unlike spindle cells that show strongly positive reactions for cytokeratin and vimentin in SEP, carcinosarcoma usually shows distinctive patterns that display cytokeratin-positive epithelial components and vimentin-positive mesenchymal components. Strictly, SEP is not in the spectrum of carcinosarcomas. However, there are some differences of view among authors concerning the concept of primary cutaneous carcinosarcoma3678. Koh et al.3 reported that carcinosarcomas encompass tumors with transitioning elements, showing overlapping morphologic and immunohistochemical features. We assume that because of the peculiar nature of the eccrine gland, primary cutaneous carcinosarcomas may have varying pathogenesis or differentiation, showing more variable expressions of immunohistochemical markers, different from conventional carcinosarcomas at other anatomical sites. Previous authors have emphasized the importance of identifying the duct-like lumina in SEP. Mehregan et al.9 focused on the outstanding features of well-formed ducts and insisted that to confirm SEP, it is crucial to recognize the glandular structure in the sarcomatous components. However, in poorly differentiated EPs, malignant tumors may not show obvious duct formation in routine hematoxylin and eosin slides. Sometimes, performing electron microscopy and immunohistochemistry may help in finding ducts or intracytoplasmic lumina10. In our case, the duct-like lesion was positive for EMA and CEA, which provides further evidence of a possible eccrine gland origin.
In the most recent report of SEP, Le et al.11 used the term ‘biphasic sarcomatoid porocarcinoma’, in which they described epithelial malignancies, with a spindle-cell component demonstrating some mesenchymal markers. On the other hand, monophasic sarcomatoid carcinomas were pure spindle cell tumors expressing markers of both epithelial and mesenchymal tumors. Either a monophasic or a biphasic sarcomatoid carcinoma diagnosis could be applied in our case, causing confusion through the presence of both epithelial and mesenchymal markers evident. To classify SEP from among these continuously emerging medical terms, we should prioritize through a focus on characteristic histopathologic findings, additional support from immunohistochemical staining, and consideration of previous references. Finally, we should consider the clinical impressions of dermatologists, because SEPs can be found in basal cell carcinoma, squamous cell carcinoma, and nevoid lesion settings. Although SEP is uncommon, it is important for pathologists to be aware of this disease entity, which has aggressive characteristic features including a high recurrence rate, frequent lympho-vascular invasion, peri-neural invasion, and very poor prognosis. Total removal of the tumor and close follow-up is necessary.
Figures and Tables
 | Fig. 1Large protruding ulcerated beefy red nodule with adjacent pinhead to bean-sized multiple nevi are present in the right zygoma (A). A flat, ill-defined, rice grain-sized, eroded, dark brown-colored patch in the superior portion of nasal bridge, between the eyes (B). |
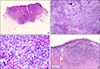 | Fig. 2A relatively well circumscribed, hypercellular tumor occupying the dermis downward to the subcutaneous fat layer, with surface ulceration (A: H&E, ×10). Glandular architecture (arrow) is mixed with haphazardly arranged spindle cells (B: H&E, ×100) showing moderate nuclear pleomorphism with numerous mitoses (C: H&E, ×400). Nests of basaloid cells with peripheral nuclear palisading in the upper dermis (D: H&E, ×40). |
 | Fig. 3Poorly differentiated tumor cells diffusely express cytokeratin (A), p63 (B) and vimentin (C). Carcinoembryonic antigen (D) and epithelial membrane antigen (E) is positive in gland forming cells, which are negative for vimentin. Ductal cells highlighted by special stain, periodic acid-Schiff (PAS)/diastase-resistant PAS (F) (A~F: H&E, ×400). |
References
1. LeBoit PE. World Health Organization. International Agency for Research on Cancer. International Academy of Pathology. European Organization for Research on Treatment of Cancer. Pathology and genetics of skin tumours. Lyon: IARC Press;2006. p. 128–130.
2. Perna C, Cuevas J, Jiménez-Heffernan JA, Hardisson D, Contreras F. Eccrine porocarcinoma (malignant eccrine poroma). Am J Surg Pathol. 2002; 26:272–274.

3. Goh SG, Dayrit JF, Calonje E. Sarcomatoid eccrine porocarcinoma: report of two cases and a review of the literature. J Cutan Pathol. 2007; 34:55–60.

4. Jeong NJ, Shi G, Im M, Seo YJ, Lee JH, Lee Y. Sarcomatoid eccrine porocarcinoma. Korean Dermatol Assoc Program Book;2011. 63:p. 215.
5. Kwan JM, Satter EK. Carcinosarcoma: a primary cutaneous tumor with biphasic differentiation. Cutis. 2013; 92:247–249.
6. Balercia G, Bhan AK, Dickersin GR. Sarcomatoid carcinoma: an ultrastructural study with light microscopic and immunohistochemical correlation of 10 cases from various anatomic sites. Ultrastruct Pathol. 1995; 19:249–263.

7. McKee P, Calonje E, Brenn T. McKee's pathology of the skin with clinical correlations. 4th ed. Philadelphia, PA: Elsevier Saunders;2012. p. 1535–1539.
8. Patterson JW. Practical skin pathology: a diagnostic approach. Philadelphia, PA: Elsevier/Saunders;2013. p. 343–344.
9. Mehregan AH, Hashimoto K, Rahbari H. Eccrine adenocarcinoma. A clinicopathologic study of 35 cases. Arch Dermatol. 1983; 119:104–114.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download