Abstract
Early detection is a crucial milestone in the prevention and treatment of schizophrenia spectrum psychosis, which might alter the course of schizophrenia. Currently, there are two complementary approaches to characterizing the clinical-high risk state of psychosis : the ultra-high risk (UHR) and basic symptoms criteria. Individuals at UHR have two phase-specific problems : heightened risk for the potential pathology of schizophrenia spectrum psychosis and the symptoms, distress and psychosocial functional impairment, which make them seek help. The clinical characteristics of UHR are similar to those of overt psychotic disorders in terms of psychopathological symptoms dimensions, psychosocial disability, neurocognitive and socio-cognitive impairments, history of trauma and abuse experience, lack of protective factors and dysfunctional metacognitive beliefs, and the comorbidity of psychiatric illness. Regarding the risk, the pretest risk probability of a psychotic disorder in each high-risk clinic is considered an important factor for predicting the power of an early detection strategy. For the distress and psychosocial disability, the strategies of the therapeutic intervention will be a focus of clinical attention. On the follow-up, one of third of the UHR individuals have sufficient positive symptom to fulfil the at-risk criteria. Most of the UHR individuals have suffered from comorbid psychiatric illness at the times of both baseline and follow-up, and there is no improvement of psychosocial functioning. Currently, it is essential to optimize the early detection and intervention strategy according to the referring and recruitment characteristics of each high-risk clinic in Korean practice situations.
Figures and Tables
 | Fig. 2 |
 | Fig. 3Hypothetical early course of the schizophrenia spectrum psychosis (according to Schultze-Lutter and Schimmelmann23)). |
 | Fig. 4Hazard plots for basic symptoms based on the levels of physical anhedonia in individuals (n=77) at the ultra-high risk for psychosis at the Clinic FORYOU of the GRAPE project (according to Bang et al.34)). |
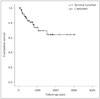 | Fig. 5Kaplan-Meier curve for the transition to schizophrenia spectrum psychosis in individuals (n=77) at the ultra-high risk for psychosis at the Clinic FORYOU of the Green Program of Recognition and Prevention of Early Psychosis project (Bang et al.34)). |
References
2. Lenzenweger MF. Schizotypy: an organizing framework for schizophrenia research. Curr Dir Psychol Sci. 2006; 15:162–166.
3. Chapman LJ, Chapman JP. The search for symptoms predictive of schizophrenia. Schizophr Bull. 1987; 13:497–503.

4. Kwapil TR. Social anhedonia as a predictor of the development of schizophrenia-spectrum disorders. J Abnorm Psychol. 1998; 107:558–565.

5. Chapman LJ, Chapman JP, Kwapil TR, Eckblad M, Zinser MC. Putatively psychosis-prone subjects 10 years later. J Abnorm Psychol. 1994; 103:171–183.

6. McGorry PD, Yung AR, Phillips LJ. The “close-in” or ultra high-risk model: a safe and effective strategy for research and clinical intervention in prepsychotic mental disorder. Schizophr Bull. 2003; 29:771–790.

7. Yung AR, Phillips LJ, Yuen HP, Francey SM, McFarlane CA, Hallgren M, et al. Psychosis prediction: 12-month follow up of a high-risk (“prodromal”) group. Schizophr Res. 2003; 60:21–32.

8. Huber G. Reine Defeksyndrome und basisstadien endogener psychosen. Fortschr Neurol Psychiat. 1966; 34:409–426.
9. Klosterkötter J, Hellmich M, Steinmeyer EM, Schultze-Lutter F. Diagnosing schizophrenia in the initial prodromal phase. Arch Gen Psychiatry. 2001; 58:158–164.

10. Schultze-Lutter F, Klosterkötter J, Picker H, Steinmeyer EM, Ruhrman S. Predicting first-episode psychosis by basic symptom criteria. Clinical Neuropsychiatry. 2007; 4:11–22.
11. Yoo SY, Lee KJ, Kang DH, Lee SJ, Ha TH, Wee W, et al. Characteristics of subjects at clinical high risk for schizophrenia: natural follow up study in ‘Seoul Youth Clinic’-pilot study. J Korean Neuropsychiatr Assoc. 2007; 46:19–28.
12. Schultze-Lutter F, Michel C, Schmidt SJ, Schimmelmann BG, Maric NP, Salokangas RK, et al. EPA guidance on the early detection of clinical high risk states of psychoses. Eur Psychiatry. 2015; 30:405–416.

13. McGlashan TH, Addington J, Cannon T, Heinimaa M, McGorry P, O'Brien M, et al. Recruitment and treatment practices for helpseeking “prodromal” patients. Schizophr Bull. 2007; 33:715–726.

14. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th ed. Washington, DC: American Psychiatric Publishing;2013.
15. Mrazek PJ, Haggerty RJ. Reducing risks for mental disorders: frontiers for preventive intervention research. Washington, DC: National Academies Press;1994. p. 19–29.
16. Bell RQ. Multiple-risk cohorts and segmenting risk as solutions to the problem of false positives in risk for the major psychoses. Psychiatry. 1992; 55:370–381.

17. Fusar-Poli P, Schultze-Lutter F, Cappucciati M, Rutigliano G, Bonoldi I, Stahl D, et al. The dark side of the moon: meta-analytical impact of recruitment strategies on risk enrichment in the clinical high risk state for psychosis. Schizophr Bull. 2016; 42:732–743.

18. Yung AR, Yuen HP, Berger G, Francey S, Hung TC, Nelson B, et al. Declining transition rate in ultra-high risk (prodromal) services: dilution or reduction of risk? Schizophr Bull. 2007; 33:673–681.

19. Nelson B, Thompson A, Yung AR. Basic self-disturbance predicts psychosis onset in the ultra high risk for psychosis “prodromal” population. Schizophr Bull. 2012; 38:1277–1287.

20. Schultze-Lutter F. Subjective symptoms of schizophrenia in research and the clinic: the basic symptom concept. Schizophr Bull. 2009; 35:5–8.

21. Klosterkötter J. The meaning of basic symptoms for the genesis of the schizophrenic nuclear syndrome. Jpn J Psychiatry Neurol. 1992; 46:609–630.

22. Debbané M, Eliez S, Badoud D, Conus P, Flückiger R, Schultze-Lutter F. Developing psychosis and its risk states through the lens of schizotypy. Schizophr Bull. 2015; 41:Suppl 2. S396–S407.
23. Schultze-Lutter F, Schimmelmann BG. Early detection and treatment of psychosis: the Bern child and adolescent psychiatric perspective. Adv Psychiatr. 2014; 2014:1–16.

24. Parnas J, Raballo A, Handest P, Jansson L, Vollmer-Larsen A, Saebye D. Self-experience in the early phases of schizophrenia: 5-year follow-up of the Copenhagen Prodromal Study. World Psychiatry. 2011; 10:200–204.

25. Parnas J, Møller P, Kircher T, Thalbitzer J, Jansson L, Handest P, et al. EASE: examination of anomalous self-experience. Psychopathology. 2005; 38:236–258.

26. Paek MJ, Kang UG. Phenomenological psychopathology. J Korean Neuropsychiatr Assoc. 2011; 50:97–115.
27. Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008; 65:28–37.

28. Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry. 2012; 69:220–229.
29. Van Os J, Delespaul P. Toward a world consensus on prevention of schizophrenia. Dialogues Clin Neurosci. 2005; 7:53–67.

30. Fusar-Poli P, Palombini E, Davies C, Oliver D, Bonoldi I, Ramella-Cravaro V, et al. Why transition risk to psychosis is not declining at the OASIS ultra high risk service: the hidden role of stable pretest risk enrichment. Schizophr Res. 2018; 192:385–390.

31. Fusar-Poli P. Why ultra high risk criteria for psychosis prediction do not work well outside clinical smaples and what to do about it. World Psychiatry. 2017; 16:212–213.

32. Schultze-Lutter F, Klosterkötter J, Ruhrmann S. Improving the clinical prediction of psychosis by combining ultra-high risk crietria and cognitive basic sympoms. Schizophr Res. 2014; 154:100–106.

33. Ruhrmann S, Schultze-Lutter F, Salokangas RK, Heinimaa M, Linszen D, Dingemans P, et al. Prediction of psychosis in adolescents and young adults at high risk: results from the prospective European prediction of psychosis study. Arch Gen Psychiatry. 2010; 67:241–251.

34. Bang M, Park JY, Kim KR, Lee SY, Song YY, Kang JI, et al. Psychotic conversion of individuals at ultra-high risk for psychosis: the potential roles of schizotypy and basic symptoms. Early Interv Psychiatry. 2017; In press.

35. Nelson B, Yuen K, Yung AR. Ultrahigh risk (UHR) for psychosis criteria: are there different levels of risk for transition to psychosis? Schizophr Res. 2011; 125:62–68.

36. Fusar-Poli P, Cappucciati M, Borgwardt S, Woods SW, Addington J, Nelson B, et al. Heterogeneity of psychosis risk within individuals at clinical high risk: a meta-analytical stratification. JAMA Psychiatry. 2016; 73:113–120.

37. Yang Z, Lim K, Lam M, Keefe R, Lee J. Factor structure of the positive and negative syndrome scale (PANSS) in people at ultra high risk (UHR) for psychosis. Schizophr Res. 2018; In press.

38. Fusar-Poli P, Nelson B, Valmaggia L, Yung AR, McGuire PK. Comorbid depressive and anxiety disorders in 509 individuals with an at-risk mental state: impact on psychopathology and transition to psychosis. Schizophr Bull. 2014; 40:120–131.

39. Pruessner M, Iyer SN, Faridi K, Joober R, Malla AK. Stress and protective factors in individuals at ultra-high risk for psychosis, first episode psychosis and healthy controls. Schizophr Res. 2011; 129:29–35.

40. Cornblatt BA, Auther AM, Niendam T, Smith CW, Zinberg J, Bearden CE, et al. Preliminary findings for two new measures of social and role functioning in the prodromal phase of schizophrenia. Schizophr Bull. 2007; 33:688–702.

41. Kim KR, Song YY, Park JY, Lee EH, Lee M, Lee SY, et al. The relationship between psychosocial functioning and resilience and negative symptoms in individuals at ultra-high risk for psychosis. Aust N Z J Psychiatry. 2013; 47:762–771.

42. Lee SJ, Kim KR, Lee SY, An SK. Impaired social and role function in ultra-high risk for psychosis and first-episode schizophrenia: its relations with negative symptoms. Psychiatry Investig. 2017; 14:186–192.

43. Corcoran CM, Kimhy D, Parrilla-Escobar MA, Cressman VL, Stanford AD, Thompson J, et al. The relationship of social function to depressive and negative symptoms in individuals at clinical high risk for psychosis. Psychol Med. 2011; 41:251–261.

44. Cotter J, Drake RJ, Bucci S, Firth J, Edge D, Yung AR. What drives poor functioning in the at-risk mental state? A systematic review. Schizophr Res. 2014; 159:267–277.

45. Cotter J, Bucci S, Drake RJ, Yung AR, Carney R, Edge D. Exploring functional impairment in young people at ultra-high risk for psychosis: a qualitative study. Early Interv Psychiatry. 2018; In press.

46. Dannevang AL, Randers L, Gondan M, Krakauer K, Nordholm D, Nordentoft M. Premorbid adjustment in individuals at ultra-high risk for developing psychosis: a case-control study. Early Interv Psychiatry. 2016; In press.

47. Brandizzi M, Valmaggia L, Byrne M, Jones C, Iwegbu N, Badger S, et al. Predictors of functional outcome in individuals at high clinical risk for psychosis at six years follow-up. J Psychiatr Res. 2015; 65:115–123.

48. Hauser M, Zhang JP, Sheridan EM, Burdick KE, Mogil R, Kane JM, et al. Neuropsychological test performance to enhance identification of subjects at clinical high risk for psychosis and to be most promising for predictive algorithms for conversion to psychosis: a meta-analysis. J Clin Psychiatry. 2017; 78:e28–e40.
49. de Paula AL, Hallak JE, Maia-de-Oliveira JP, Bressan RA, Machado-de-Sousa JP. Cognition in at-risk mental states for psychosis. Neurosci Biobehav Rev. 2015; 57:199–208.

50. Carrión RE, Walder DJ, Auther AM, McLaughlin D, Zyla HO, Adelsheim S, et al. From the psychosis prodrome to the first-episode of psychosis: no evidence of a cognitive decline. J Psychiatr Res. 2018; 96:231–238.

51. Bora E, Murray RM. Meta-analysis of cognitive deficits in ultra-high risk to psychosis and first-episode psychosis: do the cognitive deficits progress over, or after, the onset of psychosis? Schizophr Bull. 2014; 40:744–755.

52. Woods BT. Is schizophrenia a progressive neurodevelopmental disorder? Toward a unitary pathogenetic mechanism. Am J Psychiatry. 1998; 155:1661–1670.

53. Cannon TD. How schizophrenia develops: cognitive and brain mechanisms underlying onset of psychosis. Trends Cogn Sci. 2015; 19:744–756.

54. Kim HS, Shin NY, Jang JH, Kim E, Shim G, Park HY, et al. Social cognition and neurocognition as predictors of conversion to psychosis in individuals at ultra-high risk. Schizophr Res. 2011; 130:170–175.

55. Pukrop R, Ruhrmann S, Schultze-Lutter F, Bechdolf A, Brockhaus-Dumke A, Klosterkötter J. Neurocognitive indicators for a conversion to psychosis: comparison of patients in a potentially initial prodromal state who did or did not convert to a psychosis. Schizophr Res. 2007; 92:116–125.

56. Lencz T, Smith CW, McLaughlin D, Auther A, Nakayama E, Hovey L, et al. Generalized and specific neurocognitive deficits in prodromal schizophrenia. Biol Psychiatry. 2006; 59:863–871.

57. Bang M, Kim KR, Song YY, Baek S, Lee E, An SK. Neurocognitive impairments in individuals at ultra-high risk for psychosis: who will really convert. Aust N Z J Psychiatry. 2015; 49:462–470.

58. Seidman LJ, Giuliano AJ, Meyer EC, Addington J, Cadenhead KS, Cannon TD, et al. Neuropsychology of the prodrome to psychosis in the NAPLS consortium: relationship to family history and conversion to psychosis. Arch Gen Psychiatry. 2010; 67:578–588.

59. Pinkham AE, Penn DL, Green MF, Buck B, Healey K, Harvey PD. The social cognition psychometric evaluation study: results of the expert survey and RAND panel. Schizophr Bull. 2014; 40:813–823.

60. Lee TY, Hong SB, Shin NY, Kwon JS. Social cognitive functioning in prodromal psychosis: a meta-analysis. Schizophr Res. 2015; 164:28–34.

61. van Donkersgoed RJ, Wunderink L, Nieboer R, Aleman A, Pijnenborg GH. Social cognition in individuals at ultra-high risk for psychosis: a meta-analysis. PLoS One. 2015; 10:e0141075.

62. An SK, Kang JI, Park JY, Kim KR, Lee SY, Lee E. Attribution bias in ultra-high risk for psychosis and first-episode schizophrenia. Schizophr Res. 2010; 118:54–61.

63. Glenthøj LB, Fagerlund B, Hjorthøj C, Jepsen JRM, Bak N, Kristensen TD, et al. Social cognition in patients at ultra-high risk for psychosis: what is the relation to social skillsand functioning? Schizophr Res Cogn. 2016; 5:21–27.

64. Cotter J, Bartholomeusz C, Papas A, Allott K, Nelson B, Yung AR, et al. Examining the association between social cognition and functioning in individuals at ultra-high risk for psychosis. Aust N Z J Psychiatry. 2017; 51:83–92.

65. Lee SB, Koo SJ, Song YY, Lee MK, Jeong YJ, Kwon C, et al. Theory of mind as a mediator of reasoning and facial emotion recognition: findings from 200 healthy people. Psychiatry Investig. 2014; 11:105–111.

66. Lee SY, Bang M, Kim KR, Lee MK, Park JY, Song YY, et al. Impaired facial emotion recognition in individuals at ultra-high risk for psychosis and with first-episode schizophrenia, and their associations with neurocognitive deficits and self-reported schizotypy. Schizophr Res. 2015; 165:60–65.

67. Park HY, Bang M, Kim KR, Lee E, An SK. Fragile self and malevolent others: biased attribution styles in individuals at ultra-high risk for Psychosis. Psychiatry Investig. 2018; In press.

68. Cotter J, Yung AR, Carney R, Drake RJ. Metacognitive beliefs in the at-risk mental state: a systematic review and meta-analysis. Behav Res Ther. 2017; 90:25–31.

69. Morrison AP, Shryane N, Fowler D, Birchwood M, Gumley AI, Taylor HE, et al. Negative cognition, affect, metacognition and dimensions of paranoia in people at ultra-high riskof psychosis: a multi-level modelling analysis. Psychol Med. 2015; 45:2675–2684.

70. Bentall RP, Fernyhough C, Morrison AP, Lewis S, Corcoran R. Prospects for a cognitive-developmental account of psychotic experiences. Br J Clin Psychol. 2007; 46:155–173.

71. Cowan HR, McAdams DP, Mittal VA. Core beliefs in healthy youth and youth at ultra high-risk for psychosis: dimensionality and links to depression, anxiety, and attenuated psychotic symptoms. Dev Psychopathol. 2018; 6:1–14.

72. Rausch F, Eisenacher S, Elkin H, Englisch S, Kayser S, Striepens N, et al. Evaluation of the ‘Jumping to conclusions’ bias in different subgroups of the at-risk mental state: from cognitive basic symptoms to UHR criteria. Psychol Med. 2016; 46:2071–2081.

73. Kang M, Bang M, Lee SY, Lee E, Yoo SW, An SK. Coping styles in individuals at ultra-high risk for psychosis: associations with cognitive appraisals. Psychiatry Res. 2018; 264:162–168.

74. Mian L, Lattanzi GM, Tognin S. Coping strategies in individuals at ultra-high risk of psychosis: a systemic review. Early Interv Psychiatry. 2017; In press.
75. Kraan T, Velthorst E, Smit F, de Haan L, van der Gaag M. Trauma and recent life events in individuals at ultra-high risk for psychosis: review and meta-analysis. Schizophr Res. 2015; 161:143–149.

76. Kilcommons AM, Morrison AP. Relationships between trauma and psychosis: an exploration of cognitive and dissociative factors. Acta Psychiatr Scand. 2005; 112:351–359.

77. Walker EF, Diforio D. Schizophrenia: a neural diathesis-stress model. Psychol Rev. 1997; 104:667–685.

78. Kapur S. Psychosis as a state of aberrant salience: a framework linking biology, phenomenology, and pharmacology in schizophrenia. Am J Psychiatry. 2003; 160:13–23.

79. McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007; 87:873–904.

80. Thompson KN, Phillips LJ, Komesaroff P, Yuen HP, Wood SJ, Pantelis C, et al. Stress and HPA-axis functioning in young people at ultra high risk for psychosis. J Psychiatr Res. 2007; 41:561–569.

81. Brew B, Doris M, Shannon C, Mulholland C. What impact does trauma have on the at-risk mental state? A systematic literature review. Early Interv Psychiatry. 2018; 12:115–124.

82. Kraan TC, Velthorst E, Themmen M, Valmaggia L, Kempton MJ, McGuire P, et al. Child maltreatment and clinical outcome in individuals at ultra-high risk for psychosis in the EU-GEI high risk study. Schizophr Bull. 2018; 44:584–592.

83. Taylor PJ, Hutton P, Wood L. Are people at risk of psychosis also at risk of suicide and self-harm? A systematic review and meta-analysis. Psychol Med. 2015; 45:911–926.

84. Bang M, Park JY, Kim KR, Lee SY, Song YY, Kang JI, et al. Suicidal ideation in individuals at ultra-high risk for psychosis and its association with suspiciousness independent of depression. Early Interv Psychiatry. 2017; In press.

85. Schmidt SJ, Schultze-Lutter F, Bendall S, Groth N, Michel C, Inderbitzin N, et al. Mediators linking childhood adversities and trauma to suicidality in individuals at risk for psychosis. Front Psychiatry. 2017; 8:242.

86. Xu Z, Mayer B, Müller M, Heekeren K, Theodoridou A, Dvorsky D, et al. Stigma and suicidal ideation among young people at risk of psychosis after one year. Psychiatry Res. 2016; 243:219–224.

87. Kwon JS, Byun MS, Lee TY, An SK. Early intervention in psychosis: insights from Korea. Asian J Psychiatr. 2012; 5:98–105.

88. Lim J, Rekhi G, Rapisarda A, Lam M, Kraus M, Keefe RS, et al. Impact of psychiatric comorbidity in individuals at Ultra High Risk of psychosis - findings from the Longitudinal Youth at Risk Study (LYRIKS). Schizophr Res. 2015; 164:8–14.

89. Rutigliano G, Valmaggia L, Landi P, Frascarelli M, Cappucciati M, Sear V, et al. Persistence or recurrence of non-psychotic comorbid mental disorders associated with 6-year poor functional outcomes in patients at ultra high risk for psychosis. J Affect Disord. 2016; 203:101–110.

90. McGorry PD, Killackey E, Yung A. Early intervention in psychosis: concepts, evidence and future directions. World Psychiatry. 2008; 7:148–156.

91. Fusar-Poli P, Yung AR, McGorry P, van Os J. Lessons learned from the psychosis high-risk state: towards a general staging model of prodromal intervention. Psychol Med. 2014; 44:17–24.

92. Guloksuz S, van Os J. The slow death of the concept of schizophrenia and the painful birth of the psychosis spectrum. Psychol Med. 2018; 48:229–244.

93. Cordes J, Bechdolf A, Engelke C, Kahl KG, Balijepalli C, Lösch C, et al. Prevalence of metabolic syndrome in female and male patients at risk of psychosis. Schizophr Res. 2017; 181:38–42.

94. Carney R, Cotter J, Bradshaw T, Firth J, Yung AR. Cardiometabolic risk factors in young people at ultra-high risk for psychosis: a systematic review and metaanalysis. Schizophr Res. 2016; 170:290–300.

95. Carney R, Cotter J, Bradshaw T, Yung AR. Examining the physical health and lifestyle of young people at ultra-high risk for psychosis: a qualitative study involving service users, parents and clinicians. Psychiatry Res. 2017; 255:87–93.

96. Falkenberg I, Valmaggia L, Byrnes M, Frascarelli M, Jones C, Rocchetti M, et al. Why are help-seeking subjects at ultra-high risk for psychosis help-seeking? Psychiatry Res. 2015; 228:808–815.

97. van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009; 39:179–195.

98. Rapado-Castro M, McGorry PD, Yung A, Calvo A, Nelson B. Sources of clinical distress in young people at ultra high risk of psycosis. Schizophr Res. 2015; 165:15–21.

99. Chung YC, Jung HY, Kim SW, Lee SH, Shin SE, Shin YM, et al. What factors are related to delayed treatment in individuals at high risk for psychosis? Early Interv Psychiatry. 2010; 4:124–131.

100. Minzenberg MJ, Yoon JH, Carter CS. Schizophrenia. In : Hales RE, Yudofsky SC, Gabbard GO, editors. American psychiatric publishing textbook of psychiatry. 5th ed. Washington, DC: American Psychiatric Publishing, Inc.;2008. p. 407–449.
101. McGlashan T, Miller T, Woods S, Rosen J, Hoffman R, Davidson L. Structured interview for prodromal syndromes (version 4.0). New Haven, CT: PRIME Research Clinic, Yale School of Medicine;2003.
102. Elkind D, Bowen R. Imaginary audience behavior in children and adolescents. Dev Psychol. 1979; 15:38.

103. Carol EE, Mittal VA. Normative adolescent experience may confound assessment of positive symptoms in youth at ultra-high risk for psychosis. Schizophr Res. 2015; 166:358–359.

104. Fusar-Poli P, de Micheli A, Cappucciati M, Rutigliano G, Davies C, Ramella-Cravaro V, et al. Diagnostic and progronostic significance of DSM-5 attenuated psychosis syndrome in services for individuals at ultra high risk for psychosis. Schizophr Bull. 2018; 44:264–275.

105. Schultze-Lutter F, Addington J, Ruhrmann S, Klosterkötter J. Schizophrenia proneness instrument adult version (SPI-A). Rome: Giovanni Fioriti;2007.
106. Kaymaz N, Drukker M, Lieb R, Wittchen HU, Werbeloff N, Weiser M, et al. Dosub threshold psychotic experiences predict clinical outcomes in unselected non-help-seeking population-based samples? A systematic review and meta-analysis, enriched with new results. Psychol Med. 2012; 42:2239–2253.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download