Journal List > J Dent Anesth Pain Med > v.18(4) > 1100259
Rett syndrome (RS) is a neurodevelopmental disorder characterized by loss of cognitive, motor, and social skills, epilepsy, autistic behavior, abnormal airway patterns, gastroesophageal reflux, nutritional problems, and severe scoliosis. Although girls with RS show normal or near-normal growth until 6–8 months, they lose their skills after that. The anesthetic management of these patients requires care because of all these clinical features. Especially in the postoperative period, prolonged apnea is common and extubation is delayed. In this case report, the effect of using sugammadex was presented in a 16-year-old girl with RS. The patient's all bimaxillary teeth and 4 wisdom teeth were extracted under general anesthesia in one session with minimal surgical trauma and moderate bleeding. Sugammadex can be a rapid and reliable agent for the reversal of the neuromuscular block in neurodegenerative patients.
Rett syndrome (RS) is a neurodevelopmental disorder of the gray matter in the brain. It is caused by mutations in the genes encoding the methyl-cytosine-guanine binding protein 2 (MECP2) located genetically on chromosome X. The loss of MECP2 alters the function of cells in the locus coeruleus and thus affects the noradrenergic innervation of the cerebral cortex and hippocampus [1]. Being a progressive genetic disorder, the syndrome influences women and its prevalence is 1/10000 [2].
The diagnosis of RS is established through observation of classical signs and symptoms that develop during early stages [3]. In addition to loss of cognitive, motor, and social skills, RS is characterized by epilepsy, stereotypical hand movements, autistic behavior, abnormal breathing patterns, gastroesophageal reflux, nutrition problems, and severe scoliosis [4]. The complexity of the end-organ involvement and especially the progressive nature of respiratory and cardiac disease make the anesthetic care of these patients difficult.
Therefore, this paper aimed to report the anesthetic approach for a 16-year-old girl, diagnosed with RS, during multiple tooth extraction, and present a literature review.
A 16-year-old female patient weighing 45 kg was preoperatively evaluated in the anesthesiology outpatient clinic for tooth extraction.
Her medical background revealed that she was born with a birth weight of 3,500 g via normal spontaneous vaginal delivery as the 5th living child from the 6th pregnancy of a 28-year-old mother. When she was 4 months old, the abnormalities that were recognized by her mother started with inattention for the environment. While she had motor skills in the beginning, motormental retardation also followed. She was diagnosed with RS in a university hospital when she was about 12 months old.
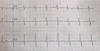
In her physical examination, she had mental retardation as well as spasticity and contractures in the extremities. No cooperation and orientation were observed. She had been having awake apnea seizures. She could not talk and walk (Fig. 1). Mallampati score was 3. Mouth opening was normal, but her dental structure was abnormal. Neck joint movements were normal. Further, she had epileptic seizures. She was taking levetiracetam, sodium valproate, and baclofen. She had neuromotor retardation for the last 3 years. Family members had kinship. No abnormality was observed in her laboratory values. In the electrocardiogram, she had borderline QT prolongation (Fig. 2).
After completing preparations for the likelihood of preoperative difficult intubation, she was transferred to the operation room. She was monitored for electrocardiogram, peripheral oxygen saturation and non invasive blood pressure. Axillary thermometer was placed in terms of malignant hyperthermia. Her preoperative saturation was 96%, heart rate was 96 beats/min, and blood pressure was 110/70 mmHg. Neuromuscular transmission monitoring was conducted through train-of-four stimuli (TOF Guard Organon Teknika B.V, Boxtel, The Netherlands) repeated every 12 s on the adductor pollicis muscle. Preoperative bispectral index (BIS) was measured as 92. She experienced awake apnea seizures lasting for approximately 15 s on the table. She was preoxygenated with O2 at 8 L/min. Premedication was not administered. After providing induction with 1 mg/kg propofol, muscle relaxation was ensured with 0.5 mg/kg rocuronium and ventilation was provided with 50% O2 – 50% air until TOF ratio reached 1%. Approximately 3 min later, when TOF reached 1%, nasotracheal intubation with spiral tube no 5 was performed. Contractures of the patient were relaxed by administering a neuromuscular blocker. With regard to hemodynamics after induction, blood pressure was 99/67 mmHg, saturation was 100%, heart rate was 89 beat/min, and BIS was 43. The stomach was aspirated using nasogastric tube. Anesthesia of patient was maintained with total intravenous anesthesia (propofol + remifentanil infusion). Infusion doses were titrated to maintain BIS at 40–60 interval. No volatile anesthetic was used. Tramadol 100 mg was administered for analgesia. Intense vital follow-up was performed during the operation. Body temperature was not elevated. Carbon dioxide (CO2) values were maintained at the range of 25–30. TOF was 1% in 60th min, 11% in the 70th min, and 25% in the 80th min after the beginning of operation. The operation took approximately 120 min. Infusions were stopped 15 min before the completion of the operation. She started to breath manually. Sugammadex 2 mg/kg (BRIDION®, Schering Plough, Turkey) was administered at this TOF ratio. TOF was 72% 1 min after the administration of sugammadex and 95% 5 min later. The patient was extubated. The patient was transferred to the intensive care unit for close follow-up. She had normal general condition and vital signs, was monitored in the intensive care for 1 day, and was referred to the service.
When considering the significant morbidities associated with RS, several specific perioperative conditions may significantly affect the risk of perioperative morbidity and mortality. Therefore, preanesthetic preparation and administration of anesthesia require care and sensitivity.
RS may be extremely susceptible to sedative agents, opioids, and volatile anesthetics, and thus, the risk of perioperative respiratory complications from delayed awakening to apnea may increase [35]. In a retrospective case-controlled study by Tofil et al., postoperative prolonged apnea was observed in 7 of 21 patients with RS [6]. In light of this preliminary information, our patient was not administered premedication.
The main concern for anesthesiologists is the likelihood of difficult airway control due to limited mouth opening, micrognathia, and limited neck movement. Although rocuronium is a good option, its effect should be expected to become prolonged in patients with hypotonic central nervous system disorders. Succinylcholine may induce hyperkalemia in neurodegenerative patients [23]. We preferred using rocuronium for this reason. TOF monitoring, used while administering neuromuscular blocking agents, enabled us to use a minimal dose of neuromuscular blocking agents and perform on time extubation without any complication, and no postoperative residual block was observed.
Succinylcholine was reported to increase QT interval that may make the patient prone to fatal arrhythmias [3]. Intubation was planned for this patient to prevent aspiration of blood when operating inside the mouth for extracting 31 teeth. For this purpose, nasotracheal intubation was performed with a single dose of rocuronium 0.5 mg/kg, and propofol and remifentanil infusion was also administered for the maintenance of anesthesia [3], provided that BİS was maintained at 40–60 interval.
Given the progressive deterioration of the central nervous system function, seizures are a frequent comorbid condition in patients with RS. Routine anticonvulsants should be administered the morning of the procedure. Most of these agents, such as barbiturates, propofol, and volatile agents, have been successfully used for the treatment of status epilepticus that is resistant to conventional therapy [3]. However, Gibert et al. recently reported that the median concentration of sevoflurane causing major epileptiform activity on EEG recordings was 4.3%, or 1.75 minimum alveolar concentration, and suggested these doses as “epileptic threshold” [7]. Because of the contradictory information regarding this issue, we did not use volatile anesthetics in this patient. The incidence of sudden death reported in RS is 22–25% [3]. Patients with RS have a prolonged QT interval. Anesthesia should be carefully performed for patients with prolonged QT interval as it may further prolong the QT interval, which increases the sympathetic tonus. Previous studies showed that volatile anesthetic agents including isoflurane, desflurane, and sevoflurane, as well as ondansetron with antiemetic properties, prolonged the QT interval; however, propofol and remifentanil were ineffective [38]. Because prolonged QT interval is associated with increased sympathetic tonus, a sufficient anesthetic depth should be provided during these procedures in order to minimize that response. Thus, BIS monitoring should be used during both the induction stage and operation.
The antagonism of neuromuscular blockade and rapid post-anesthesia recovery should be planned according to circumstances. In their study, Saarnivarra and Simola examined the effects of four anticholinesterase-anticholinergic combinations on the QT interval and determined its significant increase in approximately one minute after the administration of any drug combination and immediately after extubation [9]. Sugammadex is a cyclodextrin that consisted of 8 glucose monomers arranged in a cylindrical shape. A sugammadex molecule mechanically binds to a rocuronium or a vecuronium molecule in the plasma and results in decreased plasma concentrations of these agents. A rocuronium/vecuronium transfer takes place from all extravascular areas to the blood with the resultant gradient. Therefore, swift excretion and decurarization are ensured. Recurarization and muscarinic side effects are not expected in the decurarization created with this mechanism. Kawasaki et al. reported that they provided an event-free recovery using sugammadex with 30–50 BIS value in a patient with RS [10]. We performed a successful and rapid extubation using sugammadex in our case. No postoperative respiratory or cardiac distress was observed.
The preparation of this case was properly completed by coordinating with the family starting from the polyclinic interview to making a detailed and careful examination in the perioperative and postoperative periods. Successful anesthetic management was provided by avoiding opioids, by careful observation for the occurrence of apnea, infusion of propofol and remifentanil, and choosing sugammadex to provide neuromuscular antagonism.
In this case, we performed a successful and rapid extubation using sugammadex. We believe that sugammadex may be a reliable agent that produces a rapid reversal effect of the neuromuscular block in neurodegenerative patients. We agree with the opinion that preoperative examination, assessment of end-organ impairment based on the primary disease process, and close postoperative follow-up are mandatory for effective perioperative care.
1. Berridge CW, Waterhouse BD. The locus coeruleusnoradrenergic system: modulation of behavioral state and state-dependent cognitive processes. Brain Res Rev. 2003; 42:33–84.

2. Karaca O, Pinar HU, Ekmekcioglu SE, Dogan R. Rett syndrome and anaesthetic management: a case report. Med Science. 2017; 6:122–124.

3. Kako H, Martin DP, Cartabuke R, Beebe A, Klamar J, Tobias JD. Perioperative management of a patient with Rett syndrome. Int J Clin Exp Med. 2013; 6:393–403.
4. Huppke P, Laccone F, Kramer N, Engel W, Hanefeld F. Rett Syndrome: Analysis of MECPP2 and clinical characterization of 31 patients. Hum Mol Genet. 2000; 9:1369–1375.

5. Nho JS, Shin DS, Moon JY, Yi JW, Kang JM, Lee BJ, et al. Anesthetic management of an adult patient with Rett syndrome and limited mouth opening - a case report. Korean J Anesthesiol. 2011; 61:428–430.

6. Tofil NM, Buckmaster MA, Winkler MK, Callans BH, Islam MP, Percy AK. Deep sedation with propofol in patients with Rett syndrome. J Child Neurol. 2006; 21:210–213.

7. Gibert S, Sabourdin N, Louvet N, Moutard ML, Piat V, Guye ML, et al. Epileptogenic effect of sevoflurane: determination of the minimal alveolar concentration of sevoflurane associated with major epileptoid signs in children. Anesthesiology. 2012; 117:1253–1261.
8. Cafiero T, DiMinno RM, DiIorio C. QT interval and QT dispersion during the induction of anesthesia and tracheal intubation: a comparison of remifentanil and fentanyl. Minerva Anestesiol. 2011; 77:160–165.
9. Saarnivaara L, Simola M. Effects of four anticholinesterase-anticholinergic combination and tracheal extubation on QTc interval of the ECG, heart rate and arterial pressure. Acta Anaesth Scand. 1998; 42:460–463.

10. Kawasaki E, Mishima Y, Ito T, Ito A, Takaseya H, Kameyama N, et al. Anesthetic management of a patient with Rett syndrome associated with trismus and apnea attacks. Masui. 2012; 61:96–99.
- TOOLS
- ORCID iDs
-
Ilke Kupeli

https://orcid.org/0000-0003-3518-7365Emine Tepe

https://orcid.org/0000-0002-5238-9586Ufuk Kuyrukluyıldız

https://orcid.org/0000-0001-6820-0699 - Similar articles




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download