This article has been
cited by other articles in ScienceCentral.
Abstract
Background and Objectives
Stress echocardiography is the current standard for cardiac risk stratification of patients undergoing orthotopic liver transplantation (OLT). We aim to evaluate the role of dobutamine stress echocardiography (DSE) in predicting perioperative major adverse cardiac event (MACE) in patients undergoing OLT.
Methods
This was a single-center retrospective study including 144 OLT patients. Of 144 patients, 118 had DSE. MACE included myocardial infarction (MI), heart failure (HF), cardiovascular and all-cause death 1 year after OLT.
Results
Our study cohort included 118 patients. The mean age was 57.3±8.2 years (range, 25–72 years). There were 85 men and 33 women, male to female ratio being 2.6:1. Of 118, 15 (13%) had positive DSE and 103 (87%) had negative DSE. Perioperative MACE incidence was 5.9% (95% confidence interval [CI], 2.6–12.3%). In predicting MACE, DSE had sensitivity of 5.6% (95% CI, 0.2–29.4%), specificity 86% (95% CI, 77.3–91.9%), positive predictive value 6.7% (95% CI, 0.3–33.4%), and negative predictive value (NPV) 83.5% (95% CI, 74.6–89.8%). Eighteen patients had MACE in first year post OLT (15%, 95% CI, 9.5–23.3%). Adverse events included cardiogenic shock (2/18), systolic HF (2/18), non-ST-elevated MI (7/18), cardiac mortality (3/18), and all-cause mortality (7/18). The overall complication rate of DSE was 17% (20/118).
Conclusions
In our cohort, DSE had a low sensitivity but high NPV in predicting perioperative MACE post OLT. A similar trend was noted for DSE in predicting 1-year MACE post OLT. We reiterate the need of a better screening and risk stratification tool for OLT.
Keywords: Dobutamine stress echocardiography, Liver transplantation, Major adverse cardiac event, Coronary artery disease
INTRODUCTION
Liver transplantation has revolutionized the management of end-stage liver disease (ESLD), and is an established therapeutic option for diverse causes of ESLD.
1) Because of the extensive risk of hemodynamic instability with liver transplant surgery,
2) patients considered for orthotopic liver transplantation (OLT) undergo comprehensive preoperative evaluation including cardiac risk stratification.
Dobutamine stress echocardiography (DSE) is a commonly used modality for cardiac evaluation prior to OLT. According to the 2013 Practice Guidelines by the American Association for the Study of Liver Disease and the American Society of Transplantation, stress echocardiography receives class 1-B evidence as an initial screening test, with subsequent cardiac catheterization as clinically indicated.
3) American College of Cardiology (ACC) and American Heart Association recommend considering noninvasive stress testing for patients undergoing liver transplant with no active cardiac conditions on the basis of multiple coronary artery disease (CAD) risk factors. The specific number of risk factors that should be used to prompt testing remains to be determined, but the committee considered 3 or more to be reasonable (class IIb: level of evidence C).
4)
There is limited data for DSE as a screening modality for significant CAD and major adverse cardiac event (MACE) in ESLD population undergoing OLT evaluation. We hypothesize that DSE is not a sensitive screening test for perioperative MACE amongst patients undergoing OLT. Our study aimed at calculating sensitivity, specificity, negative predictive value (NPV), positive predictive value (PPV) of DSE in predicting perioperative MACE for patients undergoing OLT. We also report 1-year MACE rate for these patients.
METHODS
A retrospective chart review of 144 patients who underwent OLT at Albert Einstein Medical Center between 2011 and 2015 was performed. Pre- and post-transplant (1-year follow-up) clinical, laboratory and imaging data including transthoracic echocardiogram, DSE and left heart catheterization (LHC) were reviewed. A written permission was granted by the Ethics committee of the Institutional Research Board to access the patient's data (approval number: 4843). The reviewers were licensed internal medicine residents practicing in the same hospital. The population was divided as shown in
Figure 1 based on whether the DSE was performed or not. Twenty-six patients did not undergo DSE due to either low cardiac risk (22/26) or high risk (4/26), who were deemed appropriate for LHC as the initial step.
Figure 1
Flowchart depicting the number of patients who underwent DSE and LHC.
DSE = dobutamine stress echocardiography; LHC = left heart catheterization; OLT = orthotopic liver transplantation.

Before transplantation, most patients (n=118) underwent DSE as per the following protocol. A 12-lead electrocardiogram (ECG), baseline blood pressure and pulse oximetry was obtained at rest. Dobutamine was initiated at 10 mcg/kg/min and infused for approximately 3 minutes. It was titrated at 10 mcg increments to a maximum dose of 40 mcg/kg/min. Atropine in divided doses of 0.25 and 0.5 mg to a total of 2.0 mg was given as an adjunct to the dobutamine to achieve target heart rate. Target heart rate was defined as 85% of the age predicted maximum heart rate. Continuous ECG monitoring was done, blood pressure monitored during each stage and patients' symptoms were recorded. Echocardiography exam was used to obtain baseline images, low-dose images and peak-dose images and regional and global left ventricular function at rest and stress was assessed. The procedure was terminated if patient developed moderate to severe dyspnea, angina, unresponsiveness, dysrhythmia, ST changes, abnormal blood pressure response or technical problems. The study was interpreted by certified cardiologists and was referred to as positive and negative on the basis of electrocardiographic and echocardiographic criteria. DSE was considered positive if myocardial ischemia was identified as new wall motion abnormalities or worsening wall motion abnormalities in at least 2 segments, greater than 2 mV down sloping ST-segment depression measured 80 ms after J point as compared with baseline or both. Complications of the study included arrhythmia like new onset atrial fibrillation and non-sustained ventricular tachycardia which required termination of the study. Premature atrial contraction (PAC) and premature ventricular contractions (PVC) were noted, but not included as a complication of the study. Persistent hypotension with systolic blood pressure <90 mmHg or diastolic blood pressure <60 mmHg was another complication of the procedure which required early termination of the procedure. The clinical decision whether to undergo cardiac catheterization after a positive DSE was made by the consulting cardiologist. The charts of patients with positive DSE who underwent LHC (10/118) were reviewed. Significant CAD was defined as 50% or greater occlusion in the left main vessel or 70% or greater in other major coronary vessels.
Medical record of all patients was reviewed for MACE including myocardial infarction (MI), heart failure (HF), cardiogenic shock, cardiovascular death, and all-cause death within a year of transplant. MACE was further categorized into 3 groups: 1) group 1, perioperative (including intraoperative and 7 days' post OLT); 2) group 2, MACE >7 days, ≤30 days' post OLT; and 3) group 3, MACE >30 days up to 1-year post OLT. HF was defined as a new onset of systolic dysfunction with ejection fraction <50% and clinical signs of HF. MI was defined by the presence of chest pain or angina equivalents with rise in troponin with or without significant ST segment elevation in the ECG.
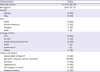
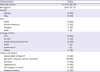
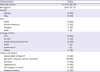
Baseline characteristics of the study cohort have been summarized in
Table 1. Sensitivity, specificity, PPV, and NPV along with their respective 95% confidence intervals (CIs) were calculated. The CAD risk factors for patients with and without MACE has been summarized in
Table 2. The χ
2 was used to calculate statistical significance (p value <0.05) for categorical variables and Mann-Whitney unpaired t-test was used for ordinal variables (
Table 2).
Table 1
Demographic characteristics of study population
|
Characteristics |
Values |
|
Mean age (years) |
57.3±8.2 (25–72) |
|
BMI (kg/m2) |
28.49 (17–51) |
|
Gender |
|
|
Female |
33 (28) |
|
Male |
85 (72) |
|
Race |
|
|
White |
73 (62) |
|
African-American |
27 (23) |
|
Hispanic |
14 (12) |
|
Asian |
4 (3) |
|
Etiology of ESLD |
|
|
HCV |
46 (39) |
|
Alcohol |
21 (18) |
|
Combined alcohol and HCV |
28 (24) |
|
NASH |
7 (6) |
|
Autoimmune |
1 (1) |
|
Others |
14 (12) |
|
Cardiac risk factors |
|
|
Obesity (BMI ≥30 kg/m2) |
42 (36) |
|
Age (men >45 years, women >55 years) |
100 (85) |
|
Smoking |
57 (48) |
|
Hypertension |
53 (45) |
|
CKD (stage 3 or more) |
45 (38) |
|
Diabetes mellitus |
35 (30) |
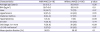
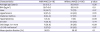
Table 2
Efficacy of DSE in predicting MACEs post-liver transplantation

|
MACE present |
MACE absent |
|
|
DSE positive |
1 |
14 |
PPV=6.7% |
|
DSE negative |
17 |
86 |
NPV=83.5% |
|
Sensitivity=5.6% |
Specificity=86% |
|
RESULTS
Twenty-six patients (18%) out of total population of 144 did not have a stress test prior to OLT. These patients either were considered low cardiac risk (22/26) and proceeded with OLT without stress test or high risk (4/26), who were deemed appropriate for LHC as the initial step by the consulting cardiologist. Two of these 4 patients did not have significant CAD in their LHC and had no MACE in the following year. One patient had chronic total occlusion of right coronary artery with left to right collateral on LHC and hence no intervention was performed. This patient subsequently developed cardiogenic shock 30 days' post-transplant leading to mortality. The fourth patient had significant CAD, underwent intervention and had no MACE in subsequent year.
A total of 118 patients underwent DSE prior to OLT for cardiac risk stratification. The mean age was 57.3±8.2 years (range, 25–72 years). There were 85 men and 33 women, male to female ratio being 2.6:1. The racial distribution, demographic characteristics, etiology of ESLD and cardiac risk factors of the study population are depicted in
Table 1.
Of 118 patients who underwent DSE, 15 (13%) had positive DSE and 103 (87%) had negative DSE. Patients with positive DSE were re-evaluated by the consulting cardiologist, and on the basis of the cardiac risk factors, 6 underwent LHC. None of them (0/6) had significant CAD on their LHC.
Eighteen patients had MACE within first year post OLT (15%, 95% CI, 9.5–23.3%). There were 7 MACE in group 1, 6 in group 2, and 5 in group 3. Group 1 included Non-ST-elevated myocardial Infarction (NSTEMI; 5/7), cardiogenic shock (1/7), and non-cardiac mortality (1/7). Group 2 included new onset CHF (2/6), NSTEMI (1/6), cardiogenic shock (1/6), cardiac mortality (1/6), and non-cardiac mortality (1/6). Group 3 included cardiac mortality (3/5), NSTEMI (1/5), and non-cardiac mortality (1/5). The distribution of MACE across time is depicted in
Figure 2. In predicting MACE, DSE had sensitivity of 5.6% (95% CI, 0.2–29.4%), specificity 86% (95% CI, 77.3–91.9%), PPV 6.7% (95% CI, 0.3–33.4%), and NPV 83.5% (95% CI, 74.6–89.8%) (
Table 2). In predicting perioperative MACE (group 1 only), DSE had sensitivity of 0% (95% CI, 0–43.9%), specificity 86.5% (95% CI 78.4–91.9%), PPV 0% (95% CI, 0–25.3%) and NPV 93.2% (95% CI, 86–96.9%). There was no statistically significant difference in the CAD risk factors of patients with and without MACE as depicted in
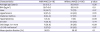
Table 3.
Figure 2
Distribution of MACE across time.
CHF = congestive heart failure; MACE = major adverse cardiac event; NSTEMI = non-ST-elevated myocardial Infarction; POD = post-operative day.

Table 3
Comparing CAD risk factors in patients with and without MACE who underwent DSE
|
Characteristics |
With MACE (n=18) |
Without MACE (n=100) |
p value |
|
Average age (years) |
59.3±5.3 |
56.9±8.6 |
0.26 |
|
BMI (kg/m2) |
28.7±5.6 |
28.5±5.8 |
0.9 |
|
Male |
12 (66.7) |
73 (73) |
0.57 |
|
Hypertension |
9 (47.4) |
44 (44) |
0.79 |
|
Diabetes mellitus |
8 (44.4) |
27 (27) |
0.16 |
|
Hyperlipidemia |
1 (5.6) |
9 (9) |
>0.99 |
|
Smoker |
7 (38.9) |
50 (50) |
0.44 |
|
CKD Stage 3 or more |
7 (38.9) |
38 (38) |
>0.99 |
|
≥3 CAD risk factors*
|
5 (27.8) |
26 (26) |
0.87 |
|
Mean ejection fraction (%) |
56.30 |
59.30 |
0.1 |
The overall complication rate of DSE including hypotension (10%) and arrhythmia (7%) was 17%. Amongst the less significant clinical arrhythmia, PVC was reported in 18 patients (15%) and PAC in 9 patients (8%).
DISCUSSION
DSE is commonly used for cardiac risk stratification among patients undergoing OLT. The purpose of cardiac evaluation before liver transplant is to assess perioperative risk and to exclude concomitant cardiac disorders that would preclude a good long-term outcome.
5) Advanced liver disease typically results in hemodynamic states that are characterized by systemic hypotension due to peripheral vasodilatation. Nevertheless, CAD is at least as frequent in OLT candidates as in the general population.
6) Therefore, noninvasive testing with echocardiography is indicated for all adult OLT candidates.
7) A crucial component of risk stratification is prediction of MACEs after surgery. The systematic review by Nguyen et al.
8) had a total incidence rate of 11% for perioperative cardiac events after OLT, with sensitivity of DSE in predicting ‘hard cardiac event’ including MI, cardiac death, and cardiac arrest to be 20%.
The composite incidence of MACE in our population was 15% over 1-year period post OLT. The MACE rate for group 1 was 5.9%, higher than group 2 (5%) and 3 (4.2%). This suggests a decreasing risk of MACE over time post transplant. All the MACE events in group 1 patients had negative DSE during the pre OLT work up. Thus, the calculated sensitivity of DSE for perioperative MACE was 0% (0/7). There might be perioperative events like excessive blood loss, fluid overload or procedural complications which predispose a patient with negative DSE to develop MACE in post OLT. A negative DSE was successful in predicting non-occurrence of MACE in 86% of our study cohort. At the same time, none of the patients with positive DSE (15/118) had perioperative MACE suggestive of poor PPV (0%). Of these 15 patients with positive DSE, 6 had LHC (non-significant CAD) and the rest 9 were deemed appropriate for OLT without the need for further cardiac work up by the consulting cardiologist. We thereby, reiterate the need of a better screening and risk stratification tool in liver transplant patients.
In general population, overall sensitivity of DSE in predicting future cardiac events is shown to be around 85%.
9) Nicolau-Raducu et al.
10) observed the sensitivity of DSE in predicting long-term MACE (median follow-up time of 3.4 years) for patients with OLT to be 9%. In our study, 11 out of 118 patients (9.3%, 95% CI, 4.9–16.4%) had MACE 1-year after OLT (excluding the first 7 days postoperative). All except one had negative DSE in pre OLT work up. In our cohort, in predicting long-term MACE, DSE had sensitivity of 9% (95% CI, 0.4–4.2%) and specificity of 86.9% (95% CI, 78.6–92.4%). Multiple factors contribute to higher cardiovascular complications after OLT. These include pre-existing metabolic factors and immunosuppressive therapy due to their metabolic effects.
11) Knowing this, we currently lack a surveillance protocol for cardiovascular disease post OLT. Among patients with OLT, cardiovascular disease continues to be the second most important cause for morbidity and mortality after malignancy.
11) Efforts to improve cardiovascular outcomes among OLT patients is an ongoing challenge and more research is needed to guide physicians achieve this goal.
Complications, such as arrhythmias and hypotension, are known to occur after administration of dobutamine. There have been reports in smaller populations showing 10% to 14% occurrence of hypotension during DSE.
12)13)14) This might be related to dynamic left ventricular obstruction
12) to cardiovascular reflexes secondary to beta-1 stimulating effect of dobutamine,
14) or caused by vasovagal reflex. However, the complications of DSE in advanced liver disease have not been well reported. In our study population, hypotension during procedure was observed in 12 (10%) patients, PVC in 18 (15%) and PAC in 9 (8%). This might be biased as these patients usually have systemic vasodilation. Ventricular fibrillation, observed in a previous study
15) was not observed in any our patients, but 9 patients (7%) developed arrhythmia, including atrial fibrillation and non-sustained ventricular tachycardia during the procedure. All complications improved with medical management, none leading to mortality.
Around 6,000 liver transplants are performed annually in United States. Our study being small in size may not be reflective of general population. The limitations of our study include its small sample size and single-center retrospective experience. Additionally, we excluded 4 patients who underwent LHC directly without undergoing DSE. Though this is a small number, it could have biased our results. Larger prospective studies with longer post OLT follow-up are needed to answer few raised questions of our study like post OLT cardiovascular risk surveillance. Newer imaging modalities like myocardial perfusion imaging (MPI) with real-time myocardial contrast echocardiography (RTMCE) may be studied in more depth to find its role in preoperative risk stratification. Tsutsui et al.
16) appreciated it as a useful tool in predicting mortality in patients with advanced liver disease. Head to head comparison trials between alternative screening modalities for predicting MACE among OLT candidates are needed to ascertain the true sensitivity of individual tests and guide our future approach to these patients with standardized protocols.
ACKNOWLEDGEMENTS
We thank Dr. Peter Nagele for his intellectual input to enhance the manuscript and for reviewing it.
References
1. Lake JR. Changing indications for liver transplantation. Gastroenterol Clin North Am. 1993; 22:213–229.

2. Donovan CL, Marcovitz PA, Punch JD, et al. Two-dimensional and dobutamine stress echocardiography in the preoperative assessment of patients with end-stage liver disease prior to orthotopic liver transplantation. Transplantation. 1996; 61:1180–1188.

3. Martin P, DiMartini A, Feng S, Brown R Jr, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American association for the study of liver diseases and the American society of transplantation. Hepatology. 2014; 59:1144–1165.

4. Lentine KL, Costa SP, Weir MR, et al. Cardiac disease evaluation and management among kidney and liver transplantation candidates: a scientific statement from the American Heart Association and the American College of Cardiology Foundation: endorsed by the American Society of Transplant Surgeons, American Society of Transplantation, and National Kidney Foundation. Circulation. 2012; 126:617–663.
5. McCaughan GW. Trekking new ground: overcoming medical and social impediments for extended criteria liver transplant recipients. Liver Transpl. 2012; 18:Suppl 2. S39–S46.

6. McAvoy NC, Kochar N, McKillop G, Newby DE, Hayes PC. Prevalence of coronary artery calcification in patients undergoing assessment for orthotopic liver transplantation. Liver Transpl. 2008; 14:1725–1731.

7. Linhares MM, Azoulay D, Matos D, et al. Liver retransplantation: a model for determining long-term survival. Transplantation. 2006; 81:1016–1021.

8. Nguyen P, Plotkin J, Fishbein TM, et al. Dobutamine stress echocardiography in patients undergoing orthotopic liver transplantation: a pooled analysis of accuracy, perioperative and long term cardiovascular prognosis. Int J Cardiovasc Imaging. 2013; 29:1741–1748.

9. Afridi I, Quinones MA, Zoghni WA, Cheirif J. Dobutamine stress echocardiography: sensitivity, specificity, and predictive value for future cardiac events. Am Heart J. 1994; 127:1510–1515.

10. Nicolau-Raducu R, Gitman M, Ganier D, et al. Adverse cardiac events after orthotopic liver transplantation: a cross-sectional study in 389 consecutive patients. Liver Transpl. 2015; 21:13–21.

11. Pisano G, Fracanzani AL, Caccamo L, Donato MF, Fargion S. Cardiovascular risk after orthotopic liver transplantation, a review of the literature and preliminary results of a prospective study. World J Gastroenterol. 2016; 22:8869–8882.

12. Pellikka PA, Oh JK, Bailey KR, Nichols BA, Monahan KH, Tajik AJ. Dynamic intraventricular obstruction during dobutamine stress echocardiography. A new observation. Circulation. 1992; 86:1429–1432.

13. Mazeika PK, Nadazdin A, Oakley CM. Paradoxical hypotension-bradycardia during dobutamine stress echocardiography. Circulation. 1991; 84:II-704.
14. Rosamond TL, Vacek JL, Crouse U. Hypotension during dobutamine stress echocardiography: the impact of chronic beta-1 selective adrenergic antagonist therapy. Circulation. 1991; 84:II-477.
15. Poldermans D, Fioretti PM, Forster T, et al. Dobutamine stress echocardiography for assessment of perioperative cardiac risk in patients undergoing major vascular surgery. Circulation. 1993; 87:1506–1512.

16. Tsutsui JM, Mukherjee S, Elhendy A, et al. Value of dobutamine stress myocardial contrast perfusion echocardiography in patients with advanced liver disease. Liver Transpl. 2006; 12:592–599.