Abstract
Pincer nail deformity is a severe condition in which the nail bed becomes compressed and the nail shows an overcurvature. We retrospectively analyzed 13 pincer nail deformities treated using our nail plate and bed reconstruction technique. Visual analogue scale scores, the width of nail root, width of nail tip, height of nail tip, width index, and height index were assessed before and after surgery. The overcurvature was corrected after detachment of the nail plate. The nail fold was pushed underneath the nail plate and then fixed. The width of nail tip significantly increased after surgery (p < 0.05) and was maintained during follow-up. The height of nail tip decreased after surgery (p < 0.05). This nail plate and bed reconstruction technique is a simple and quick surgical method for correcting deformities and reduces risks of complications such as skin necrosis and infection compared to other existing surgical techniques. We recommend this efficient surgical technique for the treatment of pincer nails.
Pincer nail deformity was first defined as a transverse overcurvature by Cornelius and Shellery in 1968.1) A pincer nail compresses the nailbed increasing pain during walking or exercising and causes cosmetic problems. It commonly develops on the lateral, medial, and bilateral sides of the big toe; it can also develop on the other toes and fingers. It is sometimes confused with an ingrown nail. A pincer nail presents as a deformity where the nail width decreases while the nail plate height increases. By contrast, an ingrown nail is a painful inflammatory condition and does not lead to severe deformity. It is a condition where the nail widens and compresses the sides of the nail bed.2)
Although many treatments are available for pincer nail deformity, the nail plate and bed reconstruction technique we devised differs from previous surgical techniques that correct the deformity as horizontally as possible and insert the nail fold underneath the nail bed. Here, we report this novel surgical treatment method for pincer nail deformity.
Eleven patients (13 cases) with pincer nail deformity of the big toe, who were treated between October 2015 and October 2016, were analyzed retrospectively. Age, sex, and duration of disease were investigated before surgery.
The width of the top and the base of each nail and the height of the curve at the tip of the nail were measured. Width index was defined as the percentage ratio of the width of the nail tip to the width of the nail root, whereas height index was defined as the percentage ratio of the height of the nail tip to the width of the nail tip (Fig. 1). We could devise treatment plans according to the severity of disease estimated from these measurements.3) The measurements were performed before surgery and at 1 and 6 months after surgery.
After confirming digital block anesthesia was sufficiently induced, a 5-mm long incision was obliquely made in the proximal area of the nail along the nail fold to approach the germinal matrix. A subperiosteal dissection was performed using an elevator, and the deformed nail plate was detached to prevent an injury to the nail bed. Next, we used a Kelly to bend the nail plate at the point of the maximal curve (Fig. 2). The nail bed was dissected from the bone using a sharp knife (#11 blade). Areas of severe hypertrophy were carefully removed using a small rongeur. Protruding osteophytes were carefully removed using a small burr.
The curvature of the nail was checked once again and the nail bed was flattened as much as possible. In the case of nails with severe deformities on the lateral side or with unclear margins, 1–2 mm of the nail was removed from the lateral side of the plate. Following the removal, any infected lesions around the nail fold were removed. To prevent recurrence, ablation was performed on the proximal nail bed. After irrigation, the nail fold was placed underneath the lifted nail bed to act as a buttress (Fig. 2). Next, the nail fold was fixed with a 3-0 nylon suture. To ensure sufficient circulation, care was taken to avoid dense suturing. The tourniquet was removed and the skin was disinfected after absence of active bleeding was confirmed (Fig. 3).
Weight bearing was allowed immediately after surgery. The sutures were removed in the 2nd postoperative week, and the patients returned to daily life in the 4th postoperative week. Visual analogue scale (VAS) scores related to pain were assessed before and after surgery. The width index and height index of each nail were calculated and compared postoperatively. For the statistical analysis, one-way analysis of variance was performed using IBM SPSS ver. 24.0 (IBM Corp., Armonk, NY, USA). The level of significance was set at p < 0.05.
We conducted this study in compliance with the principles of the Declaration of Helsinki. The protocol of this study was reviewed and approved by the Institutional Review Board of Kangdong Sacred Heart Hospital (IRB No. 2017-12-004). Written informed consents were obtained.
Of the 11 patients, seven were male and four were female. Their mean age was 61.7 years (range, 52 to 72 years). Two patients had bilateral deformities, while the other nine had unilateral deformities. The mean disease duration was 3.9 years (range, 1 to 12 years).
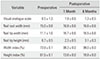
The mean nail root width increased from 15.0 ± 0.8 mm before surgery to 16.8 ± 0.6 mm after surgery. The mean nail root width was 16.6 ± 0.6 mm at the final follow-up; thus, it did not change significantly after surgery. The mean nail tip width increased from 11.1 ± 1.0 mm to 16.7 ± 0.6 mm and was 16.5 ± 0.6 mm at the final follow-up. The mean nail tip height decreased from 6.7 ± 0.5 mm to 2.3 ± 0.5 mm after nail deformity correction, and its final measurement value was 3.1 ± 0.3 mm.
The mean width index and height index changed from 73.9% ± 0.1% and 61.5% ± 0.1%, respectively, before surgery to 99.3% ± 0.0% and 13.8% ± 0.0%, respectively, after surgery. The mean width and height indices at the final follow-up were 99.0% ± 0.0% and 18.8% ± 0.0%, respectively; thus, they had not changed significantly since the surgery.
The mean VAS score decreased from 6.5 ± 1.3 before surgery to 1.9 ± 0.6 after surgery and then to 1.3 ± 0.5 at the final follow-up (Table 1). None of the patients experienced recurrence during follow-up. There were no cases in which the nails stopped growing or grew incompletely. Among the 11 patients, two showed mild ischemic changes on the incision and the sutured site. However, their wounds healed without any problem.
Pincer nail deformity can be congenital or acquired and are associated with shoes, osteoarthritis, and onychomycosis.4) Conservative treatment such as nail bracing is primarily used; however, since it often results in failure or recurrence, most patients require surgical treatment.5) Lee et al.6) reported that 14 of 35 patients (40%) who were treated for pincer nails had a history of failure of previous conservative treatment or recurrence. Since nails have curvatures, Sano and Ogawa7) nonsurgically controlled the balance between mechanical and automatic curvature forces by thinning thickness of the nail using a grinder. Afterwards, the new nail arising from growth was also thinned, and the deformity was corrected by different automatic nail curvature force and upward mechanical force. Another method consists of depression of the lateral nail folds by the dermal flap. Cho et al.8) reported treatment cases using a modified double Z-plasty to remove osteophytes and correct the nail fold. Markeeva et al.9) shortened the nail plates with a 40% urea paste and performed ablation on deformed nail beds and lateral narrowing.
When the overcurvature of a pincer nail becomes severe, it damages the nail bed, significantly reduces the nail width, and increases the height. In our patients, because some portions of the lateral sides of the nails were removed in cases of irregular margins and severe hypertrophy, there was difficulty in determining the increase in the length of the nail root. On the other hand, a large increase in the width of nail tip where deformities had been severe was observed. The nail plates were properly fixed, and thus no significant changes in the length of nail tip were observed during the 6-month follow-up period. The large height of nail tip caused by severe deformities was significantly reduced after the corrective surgery, and the results were maintained until the final follow-up. The width index was improved after correction because the nail root and tip were corrected or polished to match the lengths of each other. Similar indices were maintained during follow-up because the fixation was well maintained. The height index was significantly reduced because the nail tip width had definitely increased. Similar values for the height index were observed until the end of the follow-up period.
Although this study produced satisfactory clinical outcomes, research involving more than 11 patients is still necessary. It is also necessary to investigate the risk of recurrence through over 3–5 years of long-term follow-up. There were four follow-up losses because the condition of each patient was improved and there was no disruption to daily life. In addition, there were total seven patients who had more than 1 year of follow-up. Those patients did not show any complications or other functional problems as well. However, more systematic long-term studies and clinical comparisons with other procedures are warranted. In addition, more detailed observation of relevant clinical conditions in patients with severe complications, such as diabetes and renal disease, is needed.
Here, we proposed a new technique that allows for precise removal of bony osteophytes underneath the nail bed by lifting the nail plate. This reduces unnecessary bony removal and prevents bony destruction. Skin necrosis and ischemic changes that may occur due to the flap can also be prevented with this technique. Because there is no touching area other than the nail plate, there is no risk of interference with circulation. Removing inflammation helps with wound healing and fills the areas with granular tissues. This surgical technique can be applied to both severe bony deformity and severe nail deformity, and it is not difficult to perform.
The nail plate and bed reconstruction technique can be a useful technique considering that it facilitates precise anatomical correction compared to other previous techniques, causes few complications such as infections, and offers good clinical results.
Figures and Tables
Fig. 1
Illustration of nail measurements. A: width of the nail root. B: width of the nail tip. C: height of the nail tip. Width index = B/A × 100. Height index = C/B × 100.

Fig. 2
Illustration of nail bending technique and nail bed fixation. (A) The nail plate is bent to detach periosteum at the point of the maximal curve. (B) The nail fold is placed and fixed underneath the lifted nail bed to act as a buttress. Curved arrow: nail plate. White arrow: nail bed.
Fig. 3
Nail plate and bed reconstruction technique. (A) Preoperative photograph. (B) A 5-mm bilateral oblique incision is made in the proximal area of the nail fold. (C) We used the Kelly to bend the nail at the highest point of the curve. (D) The nail bed is gently detached from the distal phalangeal bone using a sharp #11 blade. (E) The inflammatory lesion in the nail fold is identified and removed. (F) The germinal matrix is gently ablated. (G) The nail bed under the nail plate is sutured with 3-0 or 4-0 nylon. (H) Postoperative photograph.

Table 1
Clinical Outcomes and Nail Measurements During the Treatment Period
References
1. Sano H, Ichioka S. Influence of mechanical forces as a part of nail configuration. Dermatology. 2012; 225(3):210–214.

2. Kosaka M, Kusuhara H, Mochizuki Y, Mori H, Isogai N. Morphologic study of normal, ingrown, and pincer nails. Dermatol Surg. 2010; 36(1):31–38.

4. Baran R, Haneke E, Richert B. Pincer nails: definition and surgical treatment. Dermatol Surg. 2001; 27(3):261–266.

5. el-Gammal S, Altmeyer P. Successful conservative therapy of pincer nail syndrome. Hautarzt. 1993; 44(8):535–537.
6. Lee JI, Lee YB, Oh ST, Park HJ, Cho BK. A clinical study of 35 cases of pincer nails. Ann Dermatol. 2011; 23(4):417–423.

7. Sano H, Ogawa R. A novel nonsurgical treatment for pincer nail that involves mechanical force control. Plast Reconstr Surg Glob Open. 2015; 3(2):e311.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download