Abstract
Background
The aim of this study was to assess the consistency between preoperative ultrasonographic and intraoperative measurements of the ulnar nerve in patients with cubital tunnel syndrome.
Methods
Twenty-six cases who underwent anterior transposition of the ulnar nerve for cubital tunnel syndrome were enrolled prospectively. On preoperative ultrasonography, largest cross-sectional diameters of the ulnar nerve were measured at the level of medial epicondyle (ME) and 3 cm proximal (PME) and distal (DME) to the ME on the transverse scan by a single experienced radiologist. Intraoperative direct measurements of the largest diameter at the same locations were performed by a single surgeon without knowledge of the preoperative values. The consistency between ultrasonographic and intraoperative values including the largest diameter and swelling ratio were assessed.
Results
Significant differences between ultrasonographic and intraoperative values of the largest diameter were found at all levels. The mean difference was 1.29 mm for PME, 1.38 mm for ME, and 1.12 mm for DME. The mean ME-PME swelling ratio for ultrasonographic and intraoperative measurements was 1.50 and 1.39, respectively, showing significant difference. The mean ME-DME swelling ratio for ultrasonographic and intraoperative measurements was 1.53 and 1.43, respectively, showing no significant difference.
Cubital tunnel syndrome is the second most common compression neuropathy after carpal tunnel syndrome and the cubital tunnel of the elbow is the most common site of ulnar nerve compression.1) The diagnosis of cubital tunnel syndrome has traditionally depended on information obtainedfrom detailed history taking, physical examination, and electrodiagnostic study.2) However, ulnar neuropathy around the elbow has a variety of clinical features, making it difficult to make a proper treatment decision based on clinical presentation and an electrodiagnostic study. Although electrodiagnostic study is a valuable diagnostic tool for cubital tunnel syndrome, it has some limitations such as discomfort for patients, difficulty with precise localization, inability to identify structural abnormalities, possibility of false-negative results, and the time-consuming process.3)
Recently, high-resolution ultrasonography (HRUS) has shown the potential to alleviate diagnostic uncertainty for ulnar neuropathy around the elbow.4) It can provide much information about the space-occupying lesion or surrounding anatomy and allow for optimal visualization of the nerve running the pathway and quantitative size of the nerve itself.5) Several studies have been performed to investigate the feasibility of HRUS for cubital tunnel syndrome. 126789)
However, the accuracy of HRUS on measurements of the ulnar nerve is still controversial.4) Several studies showed inconsistent results concerning the diagnostic sensitivity and specificity of HRUS in ulnar neuropathy around the elbow.41011) The differences in reported values may be the results of methodological differences in the research design, differences in measurement techniques, measurement errors, or differences in the characteristics of the patient population.7) Furthermore, few studies have investigated the accuracy of ultrasonography for cubital tunnel syndrome compared to intraoperative measurements of the ulnar nerve.12) The aim of this study was to assess the consistency between preoperative ultrasonographic and intraoperative measurements of the ulnar nerve in patients with cubital tunnel syndrome. We hypothesized that ultrasonographically measured values may be smaller than the direct intraoperative measurement values and the swelling ratio may improve diagnostic accuracy in patients with cubital tunnel syndrome.
Between 2011 and 2012, we prospectively enrolled 26 consecutive cases (three bilateral and 20 unilateral) in 23 patients who underwent anterior transposition of the ulnar nerve for cubital tunnel syndrome. All patients with cubital tunnel syndrome were diagnosed using detailed history taking, physical examination, and electrodiagnostic study according to the criteria of the American Association of Electrodiagnostic Medicine.13) Exclusion criteria included (1) a history of polyneuropathy; (2) acute trauma involving the upper extremity; (3) a history of previous elbow surgery; or (4) brachial plexus injury. We conducted this study in compliance with the principles of the Declaration of Helsinki. The protocol of this study was reviewed and approved by the Institutional Review Board of Keimyung University Dongsan Medical Center (IRB No. 201511009). Informed consent was waived.
Preoperatively, ultrasonographic examination was conducted using a 12–17 MHz linear transducer of IU 22 HRUS (Philips Medical Systems, Bothell, WA, USA) by a single experienced musculoskeletal radiologist (SML) blinded to the clinical and electrodiagnostic data.
During the examination, all patients were in the supine position with their involved arm in slight flexion position (15°). First, the pathway of the ulnar nerve from the proximal upper arm to the distal forearm was checked on the longitudinal scan. Dislocation or subluxation of the ulnar nerve, space-occupying lesion, and anatomical variance were also evaluated. Largest cross-sectional diameters of the ulnar nerve were measured at the level of medial epicondyle (ME) and 3 cm proximal (PME) and distal (DME) to the ME on the transverse scan. Diameters were estimated within the echogenic rim surrounding the nerve (Fig. 1).
Intraoperatively, largest diameters of the ulnar nerve were measured at the same locations in slight flexion position (15°) using calipers with a sensitivity of 0.1 mm by a single surgeon (CHC) (Fig. 2). The surgeon was blinded to the previous information gathered by ultrasonographic examination.
Swelling ratios were calculated by dividing the largest diameter measured at the ME by that at PME (ME-PME) and at DME (ME-DME). The consistency between ultrasonographic and intraoperative values including the largest diameter and swelling ratio were assessed.
Statistical analyses were performed using IBM SPSS ver. 22.0 (IBM Corp., Armonk, NY, USA). The Wilcoxon signed-rank test was used to compare ultrasonographic and intraoperative values according to the locations and to compare ultrasonographic and intraoperative swelling ratios. Statistical significance was set at a p-value < 0.05.
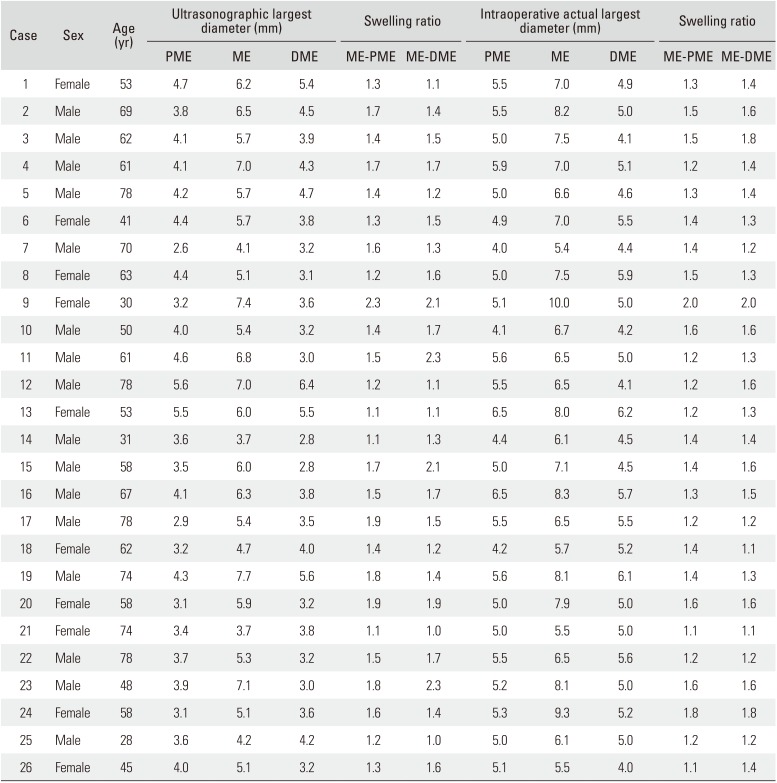
The mean age of all patients was 58.8 years (range, 28 to 78 years), and there were 16 males and 10 females. The affected limbs were equally divided between the right and left sides (13 each), and the mean duration of symptoms was 17.6 months (range, 2 to 84 months). Causes of cubital tunnel syndrome included elbow contracture due to osteoarthritis (11 cases), idiopathic causes (10 cases), cubitus valgus (three cases), ganglion (one case), and dislocation of the ulnar nerve (one case). The patient data are listed in Table 1.
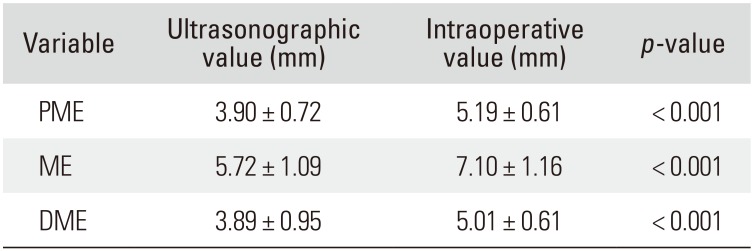
On preoperative ultrasonography, enlargement of the ulnar nerve was observed at the level of the ME in all patients. The mean value of the largest diameter of the ulnar nerve at PME, ME, and DME on the axial scan was 3.90 mm, 5.72 mm, and 3.89 mm, respectively. On the intraoperative measurement, the mean value of the largest diameter of the ulnar nerve at PME, ME, and DME was 5.19 mm, 7.10 mm, and 5.01 mm, respectively. Significant differences between ultrasonographic and intraoperative values of the largest diameters were found at all levels (all p < 0.001) (Table 2). The mean difference was 1.29 mm for PME, 1.38 mm for ME, and 1.12 mm for DME.
The mean ME-PME swelling ratio was 1.50 for ultrasonographic measurement and 1.39 for intraoperative measurement, showing significant difference (p = 0.03). The mean ME-DME swelling ratio was 1.53 for ultrasonographic measurement and 1.43 for intraoperative measurement, showing no significant difference (p = 0.17).
This study showed that the largest diameters of the ulnar nerve at three locations (PME, ME, and DME) on the ultrasonographic transverse scan were smaller than the actual values determined intraoperatively. The ME-DME swelling ratios of the ulnar nerve measured by ultrasonography were consistent with intraoperatively measured values.
Although the accuracy of ultrasonographic examination may vary depending on the experience and ability of the operator, it can show anatomical and morphological changes of the nerve, the precise compression site, osteophyte, space-occupying lesion, and anatomical variation around the elbow.111) Because of these advantages, ultrasonographic examination has been considered as a valuable adjunctive method in the diagnosis, screening, and follow-up of cubital tunnel syndrome.1211) In the present study, we could confirm morphological or dynamic changes of the ulnar nerve including enlargement, subluxation, or dislocation through ultrasonographic examination in all patients.
Several quantitative parameters including the diameter, cross-sectional area, and distal to proximal swelling ratio have been provided for ultrasonographic evaluation of cubital tunnel syndrome.126789) The cross-sectional area and largest diameter on transverse scans are frequently used as quantitative parameters.491415) Okamoto et al.1617) reported that the mean ultrasonographic value of the largest diameter of the ulnar nerve at the level of ME in patients with cubital tunnel syndrome (7.2 mm) was significantly larger than that in healthy men (3.1 mm). However, recommendations on what and how to measure vary among publications and there is no commonly agreed “standard technique.”4) Furthermore, the consistency between ultrasonographic and intraoperative measurements is undetermined as of yet. Only a single study was performed to investigate the relationship and accuracy of ultrasonographic examination compared to intraoperative measurements of the ulnar nerve;12) based on anatomical knowledge gathered during surgery, ultrasonographic measurements of the ulnar nerve were smaller than intraoperative directmeasurements.12)
Bartels et al.12) reported that the mean difference between ultrasonographic and intraoperative measurement values of the largest diameter was 3.7 mm (2.3 mm vs. 6.0 mm) on the longitudinal scan and 1.5 mm (4.4 mm vs. 6.0 mm) on the transverse scan. They concluded that the diameter of the ulnar nerve as determined ultrasonographically suggesting ulnar neuropathy did not correspond with the anatomically determined actual diameter. Because the difference on the longitudinal scan was substantial and caused by the difference in the angle of view of the surgeon and that of the probe, they suggested that the largest diameter can be best estimated using a transverse scan.12)
In this study, as a quantitative parameter of the ulnar nerve, we used the largest diameter on the transverse scan. The mean values of the largest diameter of the ulnar nerve at all reference points on the transverse scan in ultrasonography were smaller than the intraoperatively determined values. The mean difference was 1.29 mm for PME, 1.38 mm for ME, and 1.12 mm for DME. The explanation for this phenomenon may be that the epineural fibrous tissues are not seen separately in ultrasonography. Because all measurements were made within the echogenic rim, the difference may be associated with the exclusion of the thickness of the epineurium, perineurium, and perineural fibrous tissue or the difference of the ultrasonic velocity in the tissues.101216)
There is still controversy regarding the most accurate ultrasonographic parameter. Thoirs et al.7) reported that two cross-sectional measurements of the area and largest diameter of the ulnar nerve at the level of the ME were found to be robust discriminators between nerves with and without ulnar neuropathy around the elbow. Because of the high individual variation of ultrasonographic measurements of the nerve size and discrepancy between ultrasonographic and intraoperative measurements of the ulnar nerve, several researchers have been using the swelling ratio.491415) Gruber et al.4) reported that a combination of at least partial inner fascicular masking plus a cubitalto-humeral swelling ratio for cross sectional area > 1.4 showed a positive linear coherence with cubital tunnel syndrome at a specificity > 95% and a positive predictive value > 90%. They concluded that the swelling ratio may be an effective parameter for the ultrasonographic diagnosis of cubital tunnel syndrome. In the present study, we used the largest cross-sectional diameter and swelling ratios (ME-PME and ME-DME) on the transverse scan. The largest cross-sectional diameter was the only quantitative parameter that can be measured intraoperatively because cross-sectional area can only be determined by cutting the nerve to see the axial plane. According to recommendations by Yoon et al.,15) we chose to use both distal and proximal sites along the ulnar nerve for comparison because, albeit rare, one of these sites can be difficult to visualize. In our results, no significant difference was found between ultrasonographic and intraoperative ME-DME swelling ratios (1.53 vs. 1.43), although ME-PME swelling ratios (1.50 vs. 1.39) were significantly different. We believe that the ME-DME swelling ratio can be a useful parameter for diagnostic confirmation of cubital tunnel syndrome. A swelling ratio of > 1.4 may be informative for detection of cubital tunnel syndrome.
There are several limitations of this study. First, we did not perform a power analysis test. Second, a control group was not included. However, this study was focused on the consistency between ultrasonographic and intraoperative measurements of the ulnar nerve in each patient with cubital tunnel syndrome. Also, it is impossible to observe an ulnar nerve intraoperatively in healthy people. Third, both the radiologist and surgeon were blinded to the previous information including clinical record, electrodiagnostic study, ultrasonographic examination, but they were aware of the existence of cubital tunnel syndrome. Fourth, we cannot rule out the possibility of measurements errors. Although we were able to observe the complete nerve in all cases in this study, it is theoretically possible that the obtained values were not the largest diameters.12) Also, the effect of decompression could diminish the intraneural pressure leading to a smaller actual diameter of the ulnar nerve. To confirm the diagnostic value of ultrasonography in cubital tunnel syndrome, further well-designed prospective studies with larger cohorts may be needed.
Ultrasonographic largest diameters of the ulnar nerve at any levels were smaller than the actual values determined intraoperatively. The ME-DME swelling ratio of the ulnar nerve measured by ultrasonography was consistent with intraoperatively measured values and can be used as a diagnostic tool for cubital tunnel syndrome.
ACKNOWLEDGEMENTS
We thank Eun-Ji Jeon, Keimyung University Dongsan Medical Center, for her support with data collection. This study was supported by a National Research Foundation of Korea grant funded by the Korean Government (grant no. 2017R1D1A1B03035113).
References
1. Chiou HJ, Chou YH, Cheng SP, et al. Cubital tunnel syndrome: diagnosis by high-resolution ultrasonography. J Ultrasound Med. 1998; 17(10):643–648. PMID: 9771609.

2. Wiesler ER, Chloros GD, Cartwright MS, Shin HW, Walker FO. Ultrasound in the diagnosis of ulnar neuropathy at the cubital tunnel. J Hand Surg Am. 2006; 31(7):1088–1093. PMID: 16945708.

3. Jeon IH, Lee SM, Choi JW, Kim PT. Dynamic morphologic study of the ulnar nerve around the elbow using ultrasonography. J Korean Shoulder Elbow Soc. 2007; 10(1):99–105.

4. Gruber H, Glodny B, Peer S. The validity of ultrasonographic assessment in cubital tunnel syndrome: the value of a cubital-to-humeral nerve area ratio (CHR) combined with morphologic features. Ultrasound Med Biol. 2010; 36(3):376–382. PMID: 20133042.

5. Kim BK, Shin HD, Kim KC, Park JY. Tardy ulnar nerve palsy secondary to the anconeus epitrochlearis muscle: 2 case report. Clin Should Elbow. 2010; 13(2):270–274.
6. Park GY, Kim JM, Lee SM. The ultrasonographic and electrodiagnostic findings of ulnar neuropathy at the elbow. Arch Phys Med Rehabil. 2004; 85(6):1000–1005. PMID: 15179657.
7. Thoirs K, Williams MA, Phillips M. Ultrasonographic measurements of the ulnar nerve at the elbow: role of confounders. J Ultrasound Med. 2008; 27(5):737–743. PMID: 18424649.
8. Volpe A, Rossato G, Bottanelli M, et al. Ultrasound evaluation of ulnar neuropathy at the elbow: correlation with electrophysiological studies. Rheumatology (Oxford). 2009; 48(9):1098–1101. PMID: 19567661.

9. Bayrak AO, Bayrak IK, Turker H, Elmali M, Nural MS. Ultrasonography in patients with ulnar neuropathy at the elbow: comparison of cross-sectional area and swelling ratio with electrophysiological severity. Muscle Nerve. 2010; 41(5):661–666. PMID: 19941341.

10. Beekman R, Visser LH, Verhagen WI. Ultrasonography in ulnar neuropathy at the elbow: a critical review. Muscle Nerve. 2011; 43(5):627–635. PMID: 21484821.

11. Mondelli M, Filippou G, Frediani B, Aretini A. Ultrasonography in ulnar neuropathy at the elbow: relationships to clinical and electrophysiological findings. Neurophysiol Clin. 2008; 38(4):217–226. PMID: 18662618.

12. Bartels RH, Meulstee J, Verhagen WI, Luttikhuis TT. Ultrasound imaging of the ulnar nerve: correlation of preoperative and intraoperative dimensions. Clin Neurol Neurosurg. 2008; 110(7):687–690. PMID: 18486322.

13. Practice parameter for electrodiagnostic studies in ulnar neuropathy at the elbow: summary statement. American Association of Electrodiagnostic Medicine, American Academy of Neurology, American Academy of Physical Medicine and Rehabilitation. Muscle Nerve. 1999; 22(3):408–411. PMID: 10086904.
14. Scheidl E, Bohm J, Farbaky Z, Simo M, Bereczki D, Aranyi Z. Ultrasonography of ulnar neuropathy at the elbow: axonal involvement leads to greater nerve swelling than demyelinating nerve lesion. Clin Neurophysiol. 2013; 124(3):619–625. PMID: 23068559.

15. Yoon JS, Walker FO, Cartwright MS. Ultrasonographic swelling ratio in the diagnosis of ulnar neuropathy at the elbow. Muscle Nerve. 2008; 38(4):1231–1235. PMID: 18785184.

16. Okamoto M, Abe M, Shirai H, Ueda N. Diagnostic ultrasonography of the ulnar nerve in cubital tunnel syndrome. J Hand Surg Br. 2000; 25(5):499–502. PMID: 10991822.

17. Okamoto M, Abe M, Shirai H, Ueda N. Morphology and dynamics of the ulnar nerve in the cubital tunnel. Observation by ultrasonography. J Hand Surg Br. 2000; 25(1):85–89. PMID: 10763732.
Fig. 1
Ultrasonographic findings. (A) A normal ulnar nerve (largest diameter, 4.1 mm) at 3 cm proximal to the medial epicondyle. (B) Focal enlargement of the ulnar nerve (largest diameter, 7.0 mm) at the level of the medial epicondyle. (C) A normal ulnar nerve (largest diameter, 4.3 mm) at 3 cm distal to the medial epicondyle.
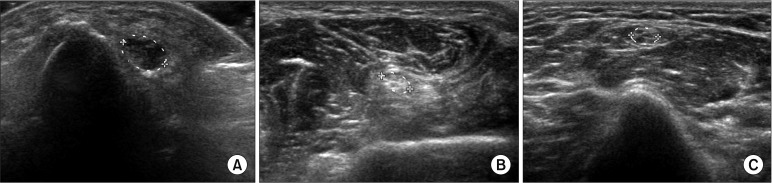
Fig. 2
Intraoperative findings. (A) Focal enlargement of the ulnar nerve. (B) Measurement of the largest diameter of the ulnar nerve at the level of the medial epicondyle using a caliper.
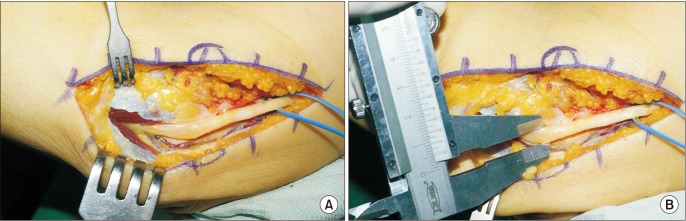
Table 1
Patient Data




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download