Abstract
Background
This study evaluated outcomes following total knee arthroplasty for severely stiff knees in Asians.
Methods
Registry data of patients undergoing primary total knee arthroplasty between 2004 and 2013 were collected and retrospectively reviewed. Sociodemographic and anthropometric data together with the Oxford Knee Score and the Knee Society Score (Knee Society Knee Score and the Knee Society Function Score) were collected both preoperatively and postoperatively for up to 2 years. Case subjects consisted of patients with a preoperative flexion range of ≤ 20°. Control subjects consisted of patients with a preoperative flexion range of > 90°. Patients were matched for age, sex, and all preoperative scores in a 2:1 fashion. Two-year outcomes and 5-year revision rates were then compared between cases and controls.
Results
There were 28 cases and 56 controls. Cases had a significantly lower body mass index than the controls (p = 0.003) and had a longer hospital stay (p < 0.0001). At 2 years, cases had a significantly lower flexion range (p < 0.001) and a lower Knee Society Function Score (p = 0.020) than the controls. Cases had a significantly greater improvement in the flexion range (p < 0.001) postoperatively than controls. The mean change in functional outcomes at 2 years was comparable between the two groups. Seventy-one percent of the cases and 88% of controls were satisfied. There was a significant difference in the 5-year revision rate (10% vs 0%, p = 0.013). More cases were discharged to a rehabilitation facility compared to controls (p = 0.011). There were no differences in inpatient complication rates.
The surgical approach for total knee arthroplasty (TKA) in a stiff knee can be very challenging, as routine patellar eversion or subluxation and adequate exposure of the joint cannot be easily achieved.123) Failure to obtain adequate exposure may lead to technical errors such as unbalanced flexion and extension gaps with resultant complications such as component malalignment. There is also the inherent risk of iatrogenic injury to the extensor mechanism such as patellar tendon rupture and avulsion of the tibial tuberosity, or collateral ligaments.4) The major goals of TKA for patients with late-stage knee osteoarthritis include relieving pain, providing knee stability, and correcting knee deformity. However, for patients with severe stiffness, increasing the flexion range after TKA will be an additional goal that may affect the clinical outcome.
There are limited reports regarding the results of primary TKA in Asians with a preoperative flexion range of ≤ 20°.5) The Asian culture requires kneeling and squatting, and patients have an expectation to achieve good flexion following TKA. Dissatisfied patients following TKA are known to value high flexion activities more than satisfied patients do.6) It is already known that the range of motion after TKA is related to the preoperative range of motion.7) How then do Asians with severely stiff knees fare following TKA? There have been many studies conducted on Western populations to evaluate outcomes following TKA in severely stiff knees, whereas there is a dearth of studies on Asian populations. We aimed to evaluate outcomes following TKA in Asians with stiff knees.
Prospectively collected registry data of all consecutive primary unilateral TKAs performed at Singapore General Hospital, a tertiary teaching hospital between January 2004 and January 2013 were assessed retrospectively. Our Institutional Review Board (No. CIRB 2017/2467) granted a waiver for informed consent for this study as no patient identifiable data was used. Patients were included only if they underwent a primary unilateral TKA with the other knee asymptomatic or successfully replaced and they completed all appropriate follow-up appointments and outcome assessments for at least 2 years following the index surgery. Exclusion criteria included the following: (1) spastic or flaccid paralysis of one or both lower limbs regardless of cause; (2) New York Heart Association Class II and III cardiac failure; (3) severe pulmonary disorders limiting the patient to only home ambulation; (4) all revision arthroplasties including infected arthroplasties; and (5) severe hip and/or spine conditions preventing the patient from ambulating independently. From this registry data, we identified 28 patients with a preoperative flexion arc of ≤ 20° and and matched them to 56 controls with a preoperative flexion arc of > 90°. Patients were matched for age, sex, and all preoperative scores in a 1:2 fashion during the same study period to ensure uniformity of follow-up.
All patients received a posterior-stabilized TKA with a fixed bearing tibial prosthesis. All surgeries were performed by fellowship-trained senior orthopaedic surgeons (NNL and SJY from Singapore General Hospital, Singapore) in a tertiary teaching hospital of a developed nation. A midline skin incision was made and the joint was exposed through a medial parapatellar approach. A medial parapatellar approach was chosen regardless of the coronal deformity as it could be easily converted into a quadriceps snip, which was required in six out of the 28 cases. Sequential soft tissue releases were performed depending on the demands of the knee deformity. Fibrous adhesion bands in the patellofemoral and suprapatellar pouch were excised. The medial and lateral gutters of the knee were developed fully. Debulking and excision of the lateral aspect of the prepatellar fat pad and division of the lateral patellofemoral ligaments were performed to help in patellar eversion. The menisci and cruciate ligaments were excised. The knee was flexed and the tibia was maneuvered anteriorly for the bone cuts. Care was taken to preserve the collateral ligaments during resection of bone and soft tissue release. No patients in our series had bony ankylosis. Tibial bone cuts were performed with use of an extramedullary guidance jig. After initial resection, the knee was carefully flexed after an extensive soft tissue release. Thereafter, tibial cuts were completed and femoral bone cuts were performed with use of an intramedullary guidance jig. Flexion and extension gaps were checked and balanced with further soft tissue release. Trial implant components were inserted. Osteotomy was performed on the patella with the final thickness not less than 12 mm. Range of motion, stability, rotational balance, and patellar tracking were manually checked with the trial components in place. The definitive implants were then cemented (Smartset; DePuy, Raynham, MA, USA). All excess cement was removed and the surgical field was irrigated copiously before wound closure in layers with sutures. Patients received mechanical or oral prophylaxis against venous thromboembolism. Patients were assessed by physiotherapists immediately following surgery and taught range of motion exercises. From the 1st postoperative day, patients ambulated with assistive devices. Patients were considered independently ambulant if they were able to ambulate independently with or without use of an aid. Patients were deemed fit for discharge to their homes after they successfully ambulated 20 to 30 m independently and after they were assessed to be competent with stair climbing, if required. The duration of hospitalization was the number of days the patient took to be independent enough to be discharged back to their own home. They were then followed up at the specialist outpatient clinic at 1 month, 3 months, 6 months, 1 year, and 2 years postoperatively.
All assessments were made independently. Baseline interviews were conducted preoperatively to assess sociodemographic characteristics, body mass index (BMI) and knee arthritis severity using the Knee Society Score (KSS)8) that consists of the Knee Society Knee Score (KSKS), the Knee Society Function Score (KSFS), and Oxford Knee Questionnaire Score (OKQS).9) We used the 1997 “12–60” version of the OKQS for which higher scores indicate greater severity. Patient satisfaction scores were recorded on a Likert scale of 1–6, with one representing excellent satisfaction and six representing extreme dissatisfaction. To generate binary data, the overall satisfaction grade was categorized into two groups with patients who answered 1, 2, and 3 being assigned to the satisfied group and those who answered 4, 5, and 6 being assigned to the dissatisfied group. The minimal clinically important difference (MCID) criterion was also used to assess whether the improvement in the KSS and OKQS was clinically meaningful. We used an MCID of 5 for both the KSS and OKQS based on previous studies conducted at our institution.1011) All data, including pre- and postoperative variables, were collected up to 2 years by hospital staff from the Orthopaedic Diagnostic Center. Comorbidities and revision surgery were assessed via the electronic health records.
We stratified the patients into two groups: cases and controls. Outcomes at 2 years were then compared between the two groups. The Student t-test was used for comparison of means and the Z-test for comparison of proportions. Revision rates were calculated for both groups at a median follow-up of 5 years.
Twenty-eight patients with severely stiff knees and 56 control subjects were identified. Among the 28 patients with severely stiff knees, the primary diagnosis was rheumatoid arthritis in 12 patients, osteoarthritis in 10 patients, and gouty arthritis in six patients. Preoperatively, the mean age and sex distribution were similar between the two groups (Table 1). The cases had a significantly lower BMI than the control subjects (26.8 vs. 29.7, p = 0.003). The mean postoperative follow-up duration for our patients was 4.3 years (range, 2.5 to 6.3 years).
Cases had a longer hospital stay than control subjects and were in the hospital for 1.4 more days than controls (p < 0.0001) (Table 1). A higher percentage of the controls (71%) was discharged directly home compared to the cases (43%) (p = 0.011). There was no significant difference in inpatient complication rates between the groups with 14% of patients with severely stiff knees experiencing postoperative complications compared to 9% of the controls (p = 0.453). These complications include superficial wound infection, urinary tract infection, and below-knee deep vein thrombosis.
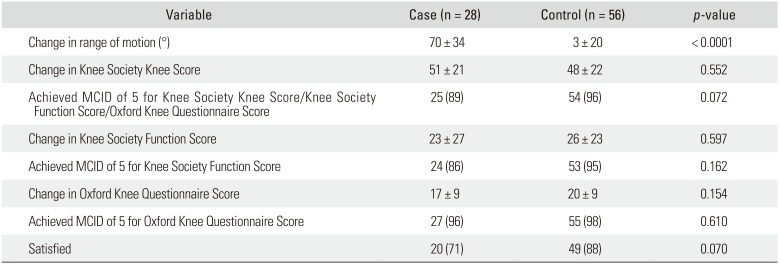
At 2 years, controls had a significantly higher flexion range than cases (118° vs. 80°, p < 0.0001) as well as a higher KSFS than cases (75 vs. 64, p = 0.020) (Table 2). However, the cases had a significantly greater improvement in the flexion range at 2 years postoperatively (70° vs. 3°, p < 0.0001) (Table 3). The mean change in functional outcomes at 2 years compared to the preoperative values was similar between the two groups (Table 3). The mean change in KSKS was 51 in the cases compared to 48 in the controls (p = 0.552), with 89% of cases and 96% of controls achieving MCID (p = 0.072). The mean change in KSFS was similar in both groups (23 vs. 26, p = 0.597), with 86% of cases and 95% of controls achieving MCID (p = 0.162). The mean change in OKQS was 17 in cases whereas it was 20 in the controls (p = 0.154), achieving MCID in 96% of cases and 98% of controls (p = 0.610).
Regarding patient satisfaction, 71% of cases and 88% of controls were satisfied (p = 0.070) at 2 years following TKA. There was a significant difference in the 5-year revision rate between the two groups with three patients (10%) with severely stiff knees requiring revision compared to none in the controls (p = 0.013). Two patients underwent revision TKA for Rorabeck C periprosthetic fractures with loose femoral components and one patient underwent a two-stage revision for periprosthetic joint infection.
Knee stiffness can be physically disfiguring, functionally limiting, and emotionally disabling in affected individuals. The functional impairment of the knee leads to pain, which further hampers activities of daily living, such as walking, sitting, and navigating stairs, as was reflected in the low preoperative KSKS in our patient population. In an Asian population, in particular, the ability to squat for cultural and religious purposes is important yet not feasible with one or more stiff knees. TKA has become mainstream for the treatment of these stiff and painful knees.1112) However, TKA can be technically challenging and the risk of complications, such as radiolucent lines, patellar fracture, infection, and skin necrosis, among others, are not insignificant12131415) and can be as high as 29%.16) Nevertheless, TKA can result in pain relief and functional improvement.17)
There are conflicting outcomes following TKA in patients with stiff or ankylosed knees.38141819202122) Nevertheless, preoperative flexion has been shown to be the strongest predictor of postoperative flexion, regardless of preoperative alignment of the knee.2324) In our study, patients with severely stiff knees had less absolute flexion (80°) than controls (118°) at 2 years postoperatively. In the series by Kim and Kim,16) absolute flexion similarly improved to a mean of 79° in 99 stiff Asian knees at final follow-up. Rajgopal et al.22) reported improved flexion to a mean of 75° in 84 stiff knees at final follow-up. Absolute flexion is an important variable to consider for its effects on daily function; 65° to 70° of flexion is reportedly necessary for the swing phase of a normal gait, at least 90° of flexion is needed to descend steps, and 105° of flexion is needed to rise independently from a low chair.
It is important to note that since the stiff knees had more range of motion to gain postoperatively than the controls in our study, the mean improvement in range of motion was significantly higher for the cases (70°) compared to controls (3°). Other series found similar results.522) In the series by Kim et al.,5) the mean range of flexion improved approximately 69° (from 9.5° to 78.5°) in 10 stiff knees that underwent TKA. Rajgopal et al.22) reported a significant mean gain of 61° following TKA in 84 stiff knees with an average follow-up of 9 years; the mean preoperative range of flexion was 14°.
At 2 years postoperatively, there were no significant differences between cases and controls in the mean OKQS and KSKS. Even though there was a significant difference in the absolute KSFS (64 in cases vs. 75 in controls) at 2 years postoperatively, this is likely not clinically significant. We say this because the proportions of patients achieving the MCID for KSFS in both cases and controls are similar (Table 2). MCID is an important concept used to determine whether a medical intervention improves perceived outcomes in patients and is believed to be a more rigorous measure of success following any intervention. Similar KSKS values between the cases and controls indicate that both groups have a similar ability to function in their daily activities although absolute flexion may remain higher for the controls.
In our study, the difference in satisfaction rates (71% vs. 88%) between cases and controls were not statistically significant but was trending towards significance. Choi and Ra25) have demonstrated that extensive preoperative discussion may contribute to improved postoperative satisfaction. After primary TKA, it has been shown that addressing patient expectations is an important factor in achieving patient satisfaction with surgical outcomes.2627) Kim et al.28) in their study found that unlike in the Western populations, limited flexion less than 130° reportedly impairs patient satisfaction in Asian populations because it precludes performance of common activities of daily living such as squatting, sitting cross-legged, or kneeling. We postulate that the relative lack of preoperative discussion and moderation of patient expectations as well as the lower absolute flexion achieved at 2 years postoperatively were all contributory factors to the lower satisfaction rate seen in the cases. Nonetheless, the authors believe that a satisfaction rate of 71% given the severe preoperative stiffness would be deemed acceptable.
While there was no difference in the inpatient complication rate between cases and controls, cases had a significantly longer postoperative length of stay. The explanation for this observation may be multifactorial. Surgical exposure during TKA for stiff knees can be challenging and thus require increased surgical manipulation to gain exposure. This increased intraoperative manipulation combined with the need for more extensive soft tissue releases may have translated into a longer postoperative length of stay than controls due to prolonged inpatient postoperative pain management. Comorbidities in patients with the limited ambulation and function associated with stiff knees may contribute to a longer length of stay.29) Another notable finding in our study was that the cases were more likely to be discharged to a rehabilitation facility instead of home. The markedly limited preoperative range of motion that characterizes these stiff knees is associated with secondary muscle contractures and weakening, and this requires more intensive postoperative rehabilitation than in those with a greater preoperative range of motion. When compared to home-based treatment, Lopez-Liria et al.30) concluded that hospital-based rehabilitation programs were significantly better at improving knee extension and strength in patients after TKA.
Moreover, there was a higher revision rate of 10% for patients with severely stiff knees at 5 years compared to 0% in controls and this indicates room for improvement. The 10% revision rate in our study compares favorably to revision rates in the published literature. Some series, such as that by Naranja et al.,15) reported revision rates as high as 35% whereas McAuley et al.18) reported a lower revision rate of 19%. In the Asian setting, Kim and Kim16) reported a rate of 4%. In our series, three cases underwent revision TKA-2 for periprosthetic fractures and one for prosthetic joint infection.
This study has several strengths. It is the first study evaluating outcomes of TKA in a Southeast Asian population with stiffness of the knee. Furthermore, the case-control study design involving a comparative control group matched for age, sex, and all preoperative scores in a 2:1 fashion for reference was suitable for less common conditions such as knee stiffness presented in this study. Data was also prospectively collected from the registry. Our patients also had good mid-term follow-up participation (mean, 4.3 years). Post-hoc power analysis showed that the study was adequately powered for all our outcome measures except for satisfaction rates where the power was only 50%. This could explain the lack of statistical significance for the difference in satisfaction between cases and controls. The weaknesses of our study include the selection bias, which is inherent to a case-control study. Since we were dealing with a relatively uncommon condition, we had a modest sample size although we believe the study is adequately powered for primary analysis. The results studied were at best short-term (i.e., 2 years). In our study, BMI was significantly higher in the control group. In current literature, there is conflicting data with regards to the impact of BMI on clinical outcomes following TKA. In a recent study by Wilson et al.,31) it was suggested that obese class III TKA patients are at increased odds of superficial and deep surgical site infection compared to other BMI cohorts. However, in an earlier study, Bin Abd Razak et al.32) concluded that BMI had little clinical impact on short-term outcomes of conventional TKAs in Asian patients. The latter study originated from the same institution as the current study with a similar patient profile. While we agree that significantly different BMI can be a confounding factor, we do not think it was a significant one in our study. Another possible criticism is the lack of radiographic evaluation. However, time points when radiographs were taken varied with individual surgeons and we could not make a meaningful comparison as such; therefore, we decided to focus on functional outcomes instead. Having originated in a unique Southeast Asian setting, the authors agree that we cannot generalize our results to other Asian countries and other hospitals. However, it is one of the few studies looking at an Asian cohort with significantly stiff knees undergoing TKA.
In our Asian population, TKA in severely stiff knees resulted in a significant gain in the range of motion and improvement in pain, satisfaction, and thus quality of life. Patients with severely stiff knees had a significantly lower flexion range than controls at 2 years following TKA. Nonetheless, functional outcomes and satisfaction rates were acceptable. While there was no difference in the inpatient complication rate, the higher revision rate for patients with severely stiff knees is a concern that warrants further research. Functional outcomes and patient satisfaction were acceptable following TKA in Asian patients with severe stiffness of the knee.
ACKNOWLEDGEMENTS
We would like to thank all the surgeons who had contributed their patients to the Singapore General Hospital Total Knee Arthroplasty Registry, without whom this study would not be possible. We would also like to extend our sincere thanks to the wonderful people at the Orthopaedic Diagnostic Centre for their hard work in maintaning the Registry.
References
1. Aglietti P, Windsor RE, Buzzi R, Insall JN. Arthroplasty for the stiff or ankylosed knee. J Arthroplasty. 1989; 4(1):1–5. PMID: 2926403.

2. Bradley GW, Freeman MA, Albrektsson BE. Total prosthetic replacement of ankylosed knees. J Arthroplasty. 1987; 2(3):179–183. PMID: 3668545.

3. Montgomery WH 3rd, Insall JN, Haas SB, Becker MS, Windsor RE. Primary total knee arthroplasty in stiff and ankylosed knees. Am J Knee Surg. 1998; 11(1):20–23. PMID: 9533049.
4. Kelly MA, Clarke HD. Stiffness and ankylosis in primary total knee arthroplasty. Clin Orthop Relat Res. 2003; (416):68–73. PMID: 14646741.

5. Kim HJ, Mun JU, Kim KH, Kyung HS. Total knee arthroplasty conversion for patients with ankylosed knees. J Orthop Surg (Hong Kong). 2017; 25(1):2309499016684095. PMID: 28142345.

6. Kim TK, Kwon SK, Kang YG, Chang CB, Seong SC. Functional disabilities and satisfaction after total knee arthroplasty in female Asian patients. J Arthroplasty. 2010; 25(3):458–464. 464.e1–464.e2. PMID: 19251391.

7. Bin Abd Razak HR, Han XA, Chong HC, Tan HC. Total knee arthroplasty in Asian subjects: preoperative range of motion determines postoperative range of motion? Orthop Surg. 2014; 6(1):33–37. PMID: 24590991.

8. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989; (248):13–14. PMID: 2805470.

9. Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998; 80(1):63–69. PMID: 9460955.

10. Lee WC, Kwan YH, Chong HC, Yeo SJ. The minimal clinically important difference for Knee Society Clinical Rating System after total knee arthroplasty for primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2017; 25(11):3354–3359. PMID: 27324635.

11. Bin Abd Razak HR, Tan CS, Chen YJ, et al. Age and preoperative Knee Society Score are significant predictors of outcomes among Asians following total knee arthroplasty. J Bone Joint Surg Am. 2016; 98(9):735–741. PMID: 27147686.

12. Kim YH, Kim JS, Cho SH. Total knee arthroplasty after spontaneous osseous ankylosis and takedown of formal knee fusion. J Arthroplasty. 2000; 15(4):453–460. PMID: 10884205.

13. Henkel TR, Boldt JG, Drobny TK, Munzinger UK. Total knee arthroplasty after formal knee fusion using unconstrained and semiconstrained components: a report of 7 cases. J Arthroplasty. 2001; 16(6):768–776. PMID: 11547376.
14. Clemens D, Lereim P, Holm I, Reikeras O. Conversion of knee fusion to total arthroplasty: complications in 8 patients. Acta Orthop. 2005; 76(3):370–374. PMID: 16156465.
15. Naranja RJ Jr, Lotke PA, Pagnano MW, Hanssen AD. Total knee arthroplasty in a previously ankylosed or arthrodesed knee. Clin Orthop Relat Res. 1996; (331):234–237.

16. Kim YH, Kim JS. Total knee replacement for patients with ankylosed knees. J Bone Joint Surg Br. 2008; 90(10):1311–1316. PMID: 18827240.

17. Suh JT, Rhee SJ, Park SH, Hong SM. Total knee arthroplasty in a patient with an ankylosing knee after previous patellectomy. Knee Surg Relat Res. 2014; 26(3):182–186. PMID: 25229049.

18. McAuley JP, Harrer MF, Ammeen D, Engh GA. Outcome of knee arthroplasty in patients with poor preoperative range of motion. Clin Orthop Relat Res. 2002; (404):203–207.

19. Kim YH, Cho SH, Kim JS. Total knee arthroplasty in bony ankylosis in gross flexion. J Bone Joint Surg Br. 1999; 81(2):296–300. PMID: 10204937.

20. Kim YH, Oh SH, Kim JS. Conversion of a fused knee with use of a posterior stabilized total knee prosthesis. J Bone Joint Surg Am. 2003; 85-A(6):1047–1050. PMID: 12784000.

21. Bhan S, Malhotra R, Kiran EK. Comparison of total knee arthroplasty in stiff and ankylosed knees. Clin Orthop Relat Res. 2006; 451:87–95. PMID: 16906096.

22. Rajgopal A, Ahuja N, Dolai B. Total knee arthroplasty in stiff and ankylosed knees. J Arthroplasty. 2005; 20(5):585–590. PMID: 16309993.

23. Gatha NM, Clarke HD, Fuchs R, Scuderi GR, Insall JN. Factors affecting postoperative range of motion after total knee arthroplasty. J Knee Surg. 2004; 17(4):196–202. PMID: 15553586.

24. Lizaur A, Marco L, Cebrian R. Preoperative factors influencing the range of movement after total knee arthroplasty for severe osteoarthritis. J Bone Joint Surg Br. 1997; 79(4):626–629. PMID: 9250752.

25. Choi YJ, Ra HJ. Patient satisfaction after total knee arthroplasty. Knee Surg Relat Res. 2016; 28(1):1–15. PMID: 26955608.

26. Chesworth BM, Mahomed NN, Bourne RB, Davis AM. OJRR Study Group. Willingness to go through surgery again validated the WOMAC clinically important difference from THR/TKR surgery. J Clin Epidemiol. 2008; 61(9):907–918. PMID: 18687289.

27. Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006; 452:35–43. PMID: 16967035.

28. Kim TK, Chang CB, Kang YG, Kim SJ, Seong SC. Causes and predictors of patient's dissatisfaction after uncomplicated total knee arthroplasty. J Arthroplasty. 2009; 24(2):263–271. PMID: 18534422.

29. Tay KS, Cher EW, Zhang K, Tan SB, Howe TS, Koh JS. Comorbidities have a greater impact than age alone in the outcomes of octogenarian total knee arthroplasty. J Arthroplasty. 2017; 32(11):3373–3378. PMID: 28641971.

30. Lopez-Liria R, Padilla-Gongora D, Catalan-Matamoros D, Rocamora-Perez P, Perez-de la Cruz S, Fernandez-Sanchez M. Home-based versus hospital-based rehabilitation program after total knee replacement. Biomed Res Int. 2015; 2015:450421. PMID: 25961017.
31. Wilson CJ, Georgiou KR, Oburu E, Theodoulou A, Deakin AH, Krishnan J. Surgical site infection in overweight and obese total knee arthroplasty patients. J Orthop. 2018; 15(2):328–332. PMID: 29881146.

32. Bin Abd Razak HR, Chong HC, Tan AH. Obesity does not imply poor outcomes in Asians after total knee arthroplasty. Clin Orthop Relat Res. 2013; 471(6):1957–1963. PMID: 23212771.

Table 1
Patient Characteristics and Postoperative Scores
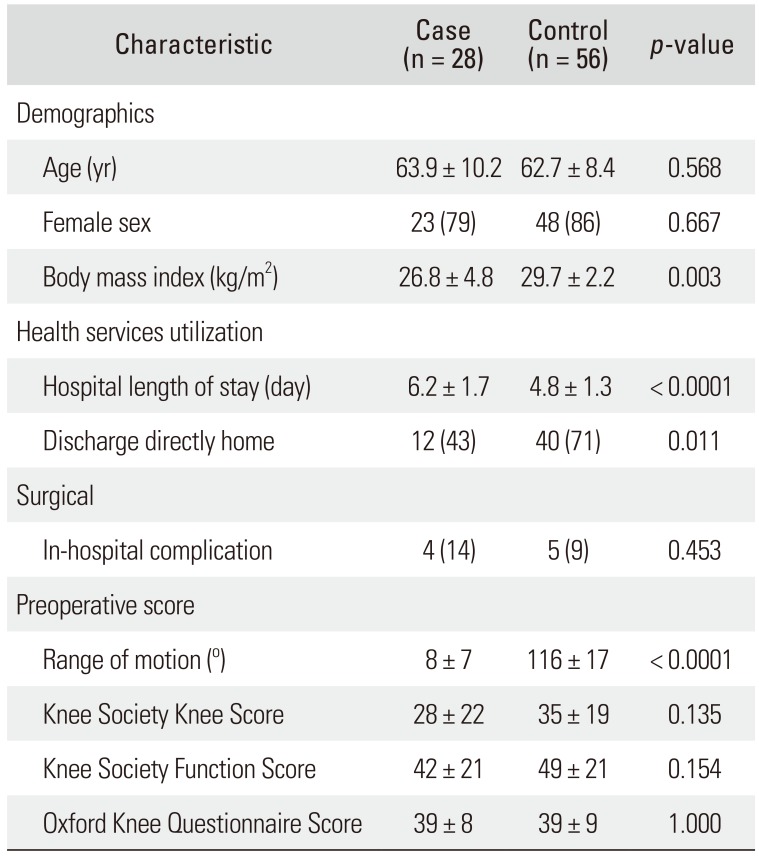
Table 2
Two-Year Postoperative Scores
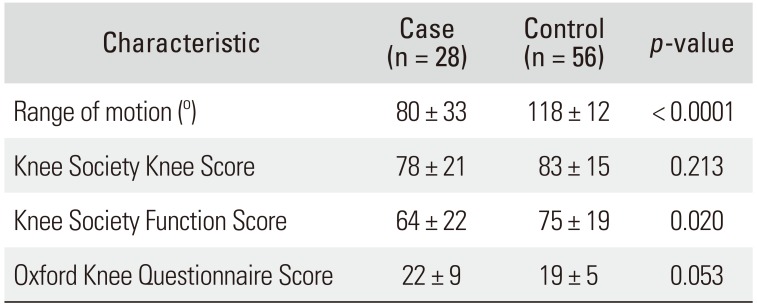
Table 3
Outcomes Assessed by Improvement, MCID, and Satisfaction




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download