Abstract
Background
The aim of this study was to evaluate the clinical and radiological outcomes of minimally invasive total knee arthroplasty (MIS-TKA) in obese patients.
Methods
We examined the records of 371 cases of MIS-TKA performed using the mini-midvastus approach from January 2006 to December 2006. According to body mass index (BMI), the cases were classified into group A (BMI < 25 kg/m2, 114 knees), group B (25 kg/m2 ≤ BMI < 30 kg/m2, 179 knees), and group C (BMI ≥ 30 kg/m2, 78 knees). Clinical outcomes were measured with the Hospital for Special Surgery Score and Knee Society Score. Radiological evaluation included measurements of knee alignment.
Results
MIS-TKA was performed on all patients. The skin incision size in group A, group B, and group C was 8.2 ± 0.8 cm, 8.3 ± 0.8 cm, and 8.5 ± 0.9 cm, respectively, and the operation time was 86.4 ± 10.4 minutes, 85.9 ± 11.3 minutes, and 89.0 ± 11.4 minutes, respectively, indicating no significant difference among the groups (p > 0.05). There was no difference in terms of the accuracy of the tibial implant alignment, with 97.6%, 95.2%, and 93.4% of each group showing 90° ± 3° varus angulation (p > 0.05). With respect to the accuracy of the femorotibial angle, 93.9%, 94.6%, and 90.2% of each group had 6° ± 3° valgus angulation, with group C demonstrating the lowest level of accuracy (p < 0.05). The preoperative range of motion and Knee Society Score of group C were less than those of groups A and B (p < 0.05), but there was no notable difference among groups at the postoperative 3-month and 1-year follow-ups (p > 0.05).
The increasing prevalence of obesity is a significant social problem. One recent survey conducted in the United States between 2011 and 2012 found that 69.0% of adults older than 20 years were overweight and 35.1% were considered obese.1) Obesity has been strongly linked to the development of osteoarthritis of the knee. Several studies have demonstrated the association between obesity and osteoarthritis.234) There is a growing tendency of patients who undergo total knee arthroplasty (TKA) being overweight or obese, along with the increase in the prevalence of obesity.5678) In 1990, it was reported that 31% of TKA patients were obese; the proportion increased to 52% in 2005.9)
The relationship between obesity and outcomes after TKA is ambiguous. Some studies have reported negative effects of obesity on the results of TKA: poor quality of life and physical function, less range of motion, and more postoperative complications such as peripheral edema, deep vein thrombosis, wound infection and dehiscence, and respiratory tract infection for obese patients with body mass index (BMI) greater than 40 kg/m2.1011121314) The relationship is also difficult to elucidate in Asian patients since there are fewer obese patients in Asia and the severity of obesity is relatively low.15)
In a midterm study, the clinical results for 78 knees of 68 obese patients were poorer than those of nonobese patients.16) A longer skin and soft tissue incision might be necessary in order to evert the patella during the conventional TKA in obese patients, which might be one of the reasons for the poor clinical results in obese patients compared to nonobese patients.717181920) Other studies have reported no significant relationship of obesity with results of TKA.716171819) Amin et al.17) reported that obesity did not influence the clinical outcomes 5 years after total knee replacement. Suleiman et al.20) reported there was no notable difference in perioperative complication rates in patients undergoing TKA or total hip arthroplasty according to BMI.
However, the above studies compared obese patients treated with conventional TKA. There are no reports on the effect of body weight on the results after primary minimally invasive TKA (MIS-TKA). MIS-TKA is believed to be helpful for less immediate postoperative pain, short skin incision, small soft tissue dissection, and preservation of integrity of the knee extensor mechanism. However, MIS may increase the risks of malpositioning of the prosthesis and wound problems with inadequate visualization of the operative field.21)
In this study, we hypothesized that MIS-TKA in obese patients would result in poorer clinical outcomes and more complications than in nonobese patients. The aim of this study was to evaluate the clinical and radiological outcomes of MIS-TKA in obese patients.
We retrospectively reviewed 379 cases (275 patients) of MIS-TKA performed by the same surgeon (JHY) from January 2006 to December 2006. Inclusion criteria were clinically significant osteoarthritis or rheumatoid arthritis of the knee and severe knee pain refractory to conventional treatment. Eight knees of eight patients were excluded from the study: one case of severe osteoarthritis with huge osteophytes, two cases of severe valgus, one case of scarred knee due to pyogenic arthritis, one case of severe tibial bone defect, one case of severe anterior angular deformity of the distal femur, and two cases of intraoperative complication including one case of rupture of the medial collateral ligament and one case of detachment of the cortex from the medial femoral condyle. There were no other complications, and the remaining 371 knees were eligible for inclusion. Institutional Review Board approval was obtained for this study (IRB No. SU-YON 2009-23HO). The senior author, who is a fellowship-trained high-volume arthroplasty surgeon (JHY), performed all of the operation with the same type of prosthesis (NexGen LPS-Flex Total Knee System; Zimmer, Warsaw, IN, USA) using Zimmer MIS instrumentation (Zimmer) (Fig. 1). All implants were of a posterior cruciate sacrificing design, and the tibial prosthesis was mini-keel type prosthesis. All MIS-TKAs were performed with the mini-midvastus approach. A curved incision from 5 mm above the medial patella to the medial tibial tuberosity was made and it was used as mobile window in the operation. We, the experienced operation team, gently moved the window for minimal soft tissue invasion in every step.22)
Deep vein thrombosis prophylaxis was performed using a foot pump for 72 hours after surgery and compression stockings were worn for 6 weeks after surgery in all patients. World Health Organization defined overweight as a BMI between 25.0 kg/m2 and 29.9 kg/m2 and obesity as a BMI of more than 30 kg/m2.62324) Accordingly, we classified 371 knees into three groups: group A (BMI < 25 kg/m2, 114 knees), group B (25 kg/m2 ≤ BMI < 30 kg/m2, 179 knees), and group C (BMI ≥ 30 kg/m2, 78 knees). We analyzed preoperative data, surgical data, radiological data, and clinical data in each group. Their mean age (69.0 years; range, 53 to 88 years) and mean follow-up period (361 weeks; range, 261 to 429 weeks) were evaluated. At the 1-year follow-up, 258 out of 371 knees could be evaluated in our outpatient clinic, and there were 114 knees in group A, 179 knees in group B, and 78 knees in group C. The length of skin incision, operative time, total blood loss, alignment of knee joint were evaluated. The length of skin incision was measured upon completion of skin suture as the straight line distance with the knee joint extended. In all cases, the Hemovac was removed in the morning of the 2nd postoperative day. The amount of bleeding for this period was recorded as the total postoperative blood loss. Preoperatively and 3 months, 1 year, and 5 years postoperatively, the same investigator (LJP) manually evaluated Knee Society Scores25) and range of motion of the knee joint.
The mean BMI was 23.1 ± 1.4 kg/m2 (range, 19.3 to 24.9 kg/m2) in group A, 27.2 ± 1.5 kg/m2 (range, 25.0 to 29.9 kg/m2) in group B, and 32.5 ± 2.1 kg/m2 (range, 30.0 to 39.0 kg/m2) in group C. Female patients were dominant (male:female = 26:345). The surgery was performed on the right side in 188 knees and on the left side in 183 knees. Rheumatoid arthritis was noted in four knees and the remaining 367 knees had osteoarthritis. There were no demographic differences between groups (Table 1).
Continuous data were expressed as mean and standard deviation while discrete data were reported as frequency. One-way analysis of variance (ANOVA) and chi-square tests were used to determine statistical differences in preoperative values, postoperative outcomes, and clinical and radiological outcomes. ANOVA test was performed to compare quantitative variables of three groups. Post-hoc analysis (Scheffe test) determined the difference between groups. The size of implants among groups was compared using Kruskal-Wallis test with statistical significance set at p < 0.05. SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Statistical differences were considered significant when the p-value was under 0.05.
The length of skin incision was 8.2 ± 0.8 cm in group A, 8.3 ± 0.8 cm in group B, and 8.5 ± 0.9 cm in group C (p > 0.05). The operative time was 86.4 ± 10.4 minutes in group A, 85.9 ± 11.3 minutes in group B, and 89.0 ± 11.4 minutes in group C (p > 0.05). Total blood loss until removal of drainage was 1,022 ± 379 mL in group A, 1,048 ± 361 mL in group B, and 1,017 ± 325 mL in group C (p > 0.05) (Table 2). Larger femoral and tibial components were used in group B than group A (p < 0.05), but there was no difference in the size of femoral and tibial components between group A and group C. The size of patellar component or thickness of bearing were not different between groups (Table 3).
In all groups, the Knee Society Scores increased after surgery. The average preoperative and postoperative 3-month and 1-year Knee Society Scores were 67.8 ± 5.8, 91.8 ± 6.0, and 95.4 ± 4.7, respectively, in group A, 66.2 ± 6.8, 92.0 ± 7.3, and 94.1 ± 6.1, respectively, in group B, and 62.7 ± 8.7, 93.3 ± 4.3, and 93.8 ± 5.0, respectively, in group C. The preoperative knee score of group C was lower than that of group A and group B (p < 0.05), but the postoperative knee scores showed no statistically significant difference between groups at postoperative 3 months and 1 year (p > 0.05) (Table 4). The average range of motion preoperatively and at postoperative 3 months, 1 year, and 5 years were 132° ± 14°, 133° ± 13°, 136° ± 10°, and 136° ± 11°, respectively, in group A, 128° ± 16°, 129° ± 14°, 132° ± 13°, and 132° ± 14°, respectively, in group B, and 118° ± 15°, 126° ± 14°, 131° ± 10°, and 133° ± 10°, respectively, in group C. The preoperative range of motion of group C was less than that of group A and group B (p < 0.05), but there was no notable difference between groups at postoperative 3 months and 1 year (p > 0.05) (Table 5). There was no clinically detectable deep vein thrombosis, infection, or major complication during the follow-up period.
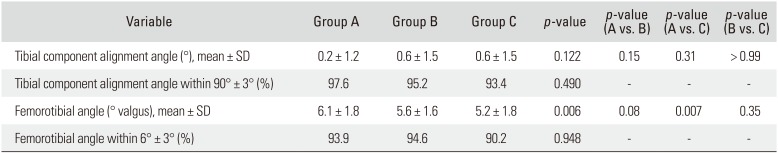
The postoperative tibial component alignment angle was similar between groups (p > 0.05). The optimal tibial component alignment angle was defined as within 3° of 90°, and it was achieved in 97.6% in group A, 95.2% in group B, and 93.4% in group C (p > 0.05). The postoperative femorotibial angle of group C (5.2° ± 1.8°) was significantly smaller than that of group A (6.1° ± 1.8°) (p = 0.007). The optimal femorotibial angle was defined as 6° ± 3° valgus, and it was achieved in 93.9% in group A, 94.6% in group B, and 90.2% in group C (p > 0.05) (Table 6).
In this study, MIS-TKA in obese patients did not result in poor clinical outcomes compared to those in nonobese patients. During the study period, there was no evidence of a longer skin incision, prolonged operative time, and more complications in obese patients. In addition, there were no significant differences between groups at the 3-month, 1-year, and 5-year follow-ups in terms of clinical outcomes and radiological outcomes.
MIS-TKA can be a reliable and safe option in obese patients regardless of the level of BMI.26) Higher BMI was not related to inferior outcome in terms of knee flexion, Knee Society pain and function scores, and postoperative pain.26) MIS has been associated with improved early clinical outcome without sacrificing radiographic positioning of the implants.1325) The similar length of skin incision between obese and nonobese patients indicates relatively less soft tissue damage in obese patients than nonobese patients. This can be attributed to mini mid-vastus surgical approach, quadriceps-sparing MIS instruments, mini-keel type tibial prosthesis, and the well experienced surgical team. In addition, the relatively flexible tension of soft tissue in obese patients may contribute to successful MIS. Based on previous studies, fat distribution and consistency are probably more important and reliable factors in identifying candidates for the mini-incision approach.52627) The authors of such studies suggested that obese patients with relatively thin lower limbs and elastic tissues would be suitable for short incisions.2627) In the current study, larger femoral and tibial prostheses were used in group B than group A, but group A and group C had similar component sizes. Therefore, it can be deduced that obesity does not necessitate the use of a large prosthesis, and it is one of the reasons for the possibility of MIS-TKA in obese patients.
Many authors reported relatively poor clinical and radiological results of TKA in obese patients with a BMI over 40 kg/m2 compared to nonobese patients.10152829) However, there were few obese patients in Asian population and the severity of obesity was also relatively low.15) In the present study, although the preoperative range of motion of the knee joint and Knee Society Scores were lower in group C than group A or group B, there was no notable difference between groups at the 3-month, 1-year, and 5-year follow-ups. This means that the clinical outcomes were better improved in the obese group than the nonobese group after TKA. The radiological data showing postoperative tibial component alignment angle were similar between groups (p > 0.05). Group A had more optimal femorotibial angle than group C. Focal osteolysis in obese patients was five times greater than that in nonobese patients in a study by spice et al.,19) and the prevalence of nonprogressive radiolucent lines was higher in obese patients in previous studies.152629) However, no knee in our study showed focal osteolysis and radiolucency. No major intraoperative complication was noted due to the careful and skillful surgical technique of the surgical team.
This study has several limitations. This study has a retrospective design, and reproducibility of the outcomes is not guaranteed considering all MIS-TKAs in our patients were performed by the same experienced surgeon. It is common to have inadequate exposure of the surgical field in TKA on obese patients. Under such circumstance, a long incision may be considered necessary for surgical convenience. However, the surgeon also needs to consider expectations of patients, pain relief with minimal cosmetic damage. For this purpose, skin incision should be minimal, if possible, and the mini-midvastus approach using MIS instrument would be beneficial for obese patients unless there is significant difference in clinical results of MIS between the obese and nonobese patients.
In this study, MIS-TKA in obese patients resulted in relatively satisfactory radiological outcomes and midterm clinical outcomes. There was no significant difference between the nonobese and obese groups regarding the skin incision, operative time, success rate of MIS, postoperative Knee Society Score and complication rate during the postoperative 5-year follow-up. Therefore, with appropriate technical support, MIS-TKA using the mini-midvastus approach can be useful in obese patients.
ACKNOWLEDGEMENTS
The authors would like to thank investigator Li-Jeung Park, RN, Department of Orthopedic Surgery, National Health Insurance Service Ilsan Hospital, Goyang, and participants involved for facilitating this research.
References
1. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014; 311(8):806–814. PMID: 24570244.

2. Cooper C, McAlindon T, Snow S, et al. Mechanical and constitutional risk factors for symptomatic knee osteoarthritis: differences between medial tibiofemoral and patellofemoral disease. J Rheumatol. 1994; 21(2):307–313. PMID: 8182642.
3. Felson DT, Anderson JJ, Naimark A, Walker AM, Meenan RF. Obesity and knee osteoarthritis. The Framingham Study. Ann Intern Med. 1988; 109(1):18–24. PMID: 3377350.
4. Hart DJ, Spector TD. The relationship of obesity, fat distribution and osteoarthritis in women in the general population: the Chingford Study. J Rheumatol. 1993; 20(2):331–335. PMID: 8474072.
5. Aglietti P, Rinonapoli E. Total condylar knee arthroplasty: a five-year follow-up study of 33 knees. Clin Orthop Relat Res. 1984; (186):104–111. PMID: 6723130.
6. Ahlberg A, Lunden A. Secondary operations after knee joint replacement. Clin Orthop Relat Res. 1981; (156):170–174.

7. Mont MA, Mathur SK, Krackow KA, Loewy JW, Hungerford DS. Cementless total knee arthroplasty in obese patients: a comparison with a matched control group. J Arthroplasty. 1996; 11(2):153–156. PMID: 8648308.
8. Stern SH, Insall JN. Total knee arthroplasty in obese patients. J Bone Joint Surg Am. 1990; 72(9):1400–1404. PMID: 2229120.

9. Fehring TK, Odum SM, Griffin WL, Mason JB, McCoy TH. The obesity epidemic: its effect on total joint arthroplasty. J Arthroplasty. 2007; 22(6 Suppl 2):71–76.
10. Amin AK, Clayton RA, Patton JT, Gaston M, Cook RE, Brenkel IJ. Total knee replacement in morbidly obese patients: results of a prospective, matched study. J Bone Joint Surg Br. 2006; 88(10):1321–1326. PMID: 17012421.
11. Friedman RJ, Hess S, Berkowitz SD, Homering M. Complication rates after hip or knee arthroplasty in morbidly obese patients. Clin Orthop Relat Res. 2013; 471(10):3358–3366. PMID: 23670675.

12. Gadinsky NE, Ehrhardt JK, Urband C, Westrich GH. Effect of body mass index on range of motion and manipulation after total knee arthroplasty. J Arthroplasty. 2011; 26(8):1194–1197. PMID: 21277161.

13. Liljensoe A, Lauersen JO, Soballe K, Mechlenburg I. Overweight preoperatively impairs clinical outcome after knee arthroplasty: a cohort study of 197 patients 3–5 years after surgery. Acta Orthop. 2013; 84(4):392–397. PMID: 23992141.
14. Seo JG, Moon YW, Jo BC, Kim YT, Park SH. Soft tissue balancing of varus arthritic knee in minimally invasive surgery total knee arthroplasty: comparison between posterior oblique ligament release and superficial MCL release. Knee Surg Relat Res. 2013; 25(2):60–64. PMID: 23741700.

15. Tay K, Bin Abd Razak HR, Tan AH. Obesity and venous thromboembolism in total knee arthroplasty patients in an Asian population. J Arthroplasty. 2016; 31(12):2880–2883. PMID: 27369301.

16. Foran JR, Mont MA, Etienne G, Jones LC, Hungerford DS. The outcome of total knee arthroplasty in obese patients. J Bone Joint Surg Am. 2004; 86(8):1609–1615. PMID: 15292406.

17. Amin AK, Patton JT, Cook RE, Brenkel IJ. Does obesity influence the clinical outcome at five years following total knee replacement for osteoarthritis? J Bone Joint Surg Br. 2006; 88(3):335–340. PMID: 16498007.

18. Deshmukh RG, Hayes JH, Pinder IM. Does body weight influence outcome after total knee arthroplasty? A 1-year analysis. J Arthroplasty. 2002; 17(3):315–319. PMID: 11938508.

19. Spicer DD, Pomeroy DL, Badenhausen WE, et al. Body mass index as a predictor of outcome in total knee replacement. Int Orthop. 2001; 25(4):246–249. PMID: 11561501.

20. Suleiman LI, Ortega G, Ong'uti SK, et al. Does BMI affect perioperative complications following total knee and hip arthroplasty? J Surg Res. 2012; 174(1):7–11. PMID: 21816426.

21. Dalury DF, Dennis DA. Mini-incision total knee arthroplasty can increase risk of component malalignment. Clin Orthop Relat Res. 2005; 440:77–81. PMID: 16239787.

22. Yoo JH, Park BK, Han CD, Oh HC, Park SH. Minimum 5-year follow-up results of minimally invasive total knee arthroplasty using mini-keel modular tibial implant. Knee Surg Relat Res. 2014; 26(3):149–154. PMID: 25229044.

23. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: the evidence report. National Institutes of Health. Obes Res. 1998; 6(Suppl 2):51S–209S. PMID: 9813653.
24. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000; 894:i–xii. 1–253. PMID: 11234459.
25. Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989; (248):9–12.

26. Chalidis BE, Petsatodis G, Christodoulou AG, Christoforidis J, Papadopoulos PP, Pournaras J. Is obesity a contraindication for minimal invasive total knee replacement? A prospective randomized control trial. Obes Surg. 2010; 20(12):1633–1641. PMID: 19756888.

27. Aglietti P, Baldini A, Giron F, Sensi L. Minimally invasive total knee arthroplasty: is it for everybody? HSS J. 2006; 2(1):22–26. PMID: 18751842.

28. Winiarsky R, Barth P, Lotke P. Total knee arthroplasty in morbidly obese patients. J Bone Joint Surg Am. 1998; 80(12):1770–1774. PMID: 9875934.

Fig. 1
(A) Anteroposterior radiograph of a well-fixed NexGen Legacy posterior stabilized flex fixed bearing and modular tibial implant total knee prosthesis in a 79-year-old female with a body mass index of 28.2 kg/m2 (weight, 79 kg; height, 1.47 m). (B) Lateral radiograph showing the skin incision length of 8.5 cm.
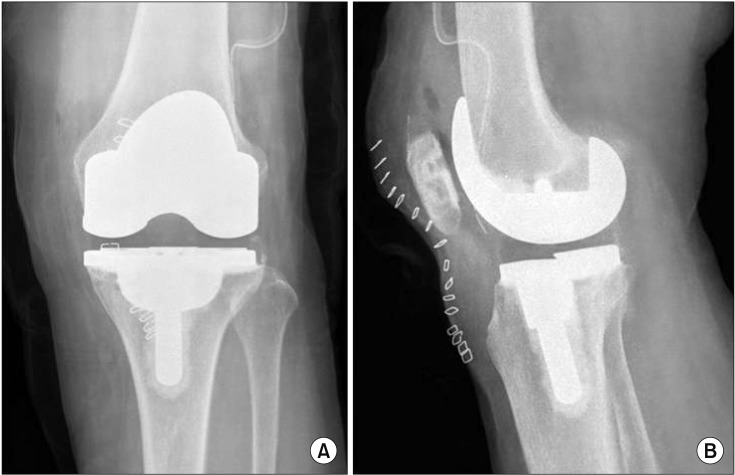
Table 1
Patient Demographics
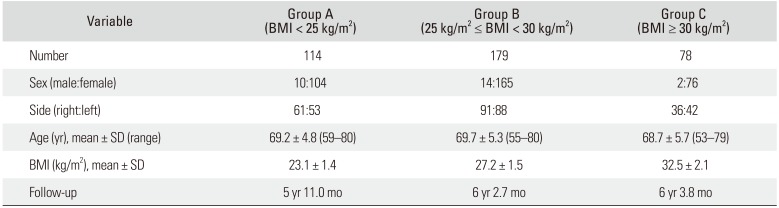
Table 2
Postoperative Surgical Data
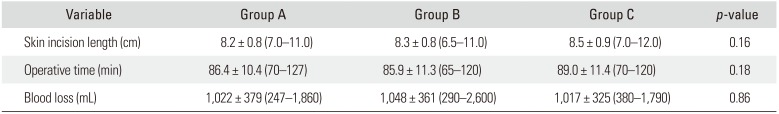
Table 3
Size of Prosthesis
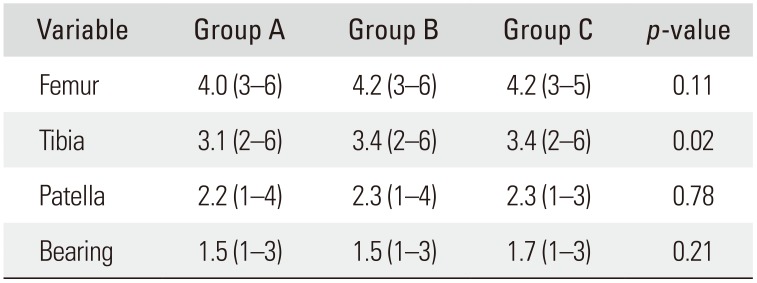
Values are presented as mean (range). Group A: body mass index (BMI) < 25 kg/m2. Group B: 25 kg/m2 ≤ BMI < 30 kg/m2. Group C: BMI ≥ 30 kg/m2. Size of femur: A = 1, B = 2, C = 3, D = 4, E = 5, F = 6; size of tibia: 1 = 1, 2 = 2, 3 = 3, 4 = 4, 5 = 5, 6 = 6; size of patella: 26 mm = 1, 29 mm = 2, 32 mm = 3, 35 mm = 3, 38 mm = 4; thickness of polyethylene: 10 mm = 1, 12 mm = 2, 14 mm = 3, 17 mm = 4.
Table 4
Postoperative Knee Score
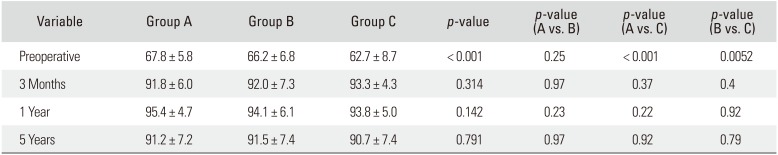
Table 5
Postoperative ROM
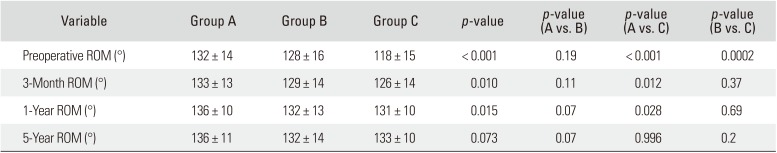
Table 6
Postoperative Component Alignment




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download