Abstract
Background
We evaluated the radiological and clinical results of reduction using a dynamic hip screw according to the grade of medial cortical support in patients with AO Foundation and Orthopaedic Trauma Association (AO/OTA) classification type 31-A2 pertrochanteric fractures.
Methods
We enrolled 100 patients with AO/OTA type 31-A2 fractures with displaced lesser trochanter fragments (length of the cortical area longer than 20 mm on the pelvis anteroposterior view). Patients with positive medial cortical support were assigned to group 1 (n = 28); neutral medial cortical support, group 2 (n = 42); and negative medial cortical support, group 3 (n = 30). Radiological evaluation was done by measuring the change in the femoral neck-shaft angle and sliding distance of the lag screw. Clinical outcomes of each group were compared by means of the walking ability score proposed by Ceder.
Results
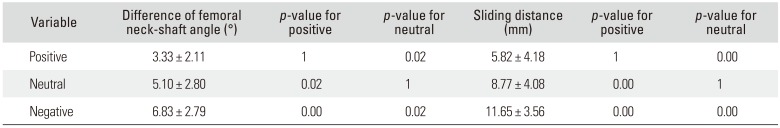
Group 1 showed significantly less changes in the femoral neck-shaft angle and shorter sliding distance than groups 2 and 3. Group 2 showed significantly less changes in the femoral neck-shaft angle and shorter sliding distance than group 3. Group 1 showed significantly higher walking ability scores than group 3 (p = 0.00). The use of trochanter stabilizing plates or fixation using wires for posteromedial wall defect resulted in no significant changes in terms of the femoral neck-shaft angle or sliding distance.
Restoration of posteromedial cortical continuity is essential for successful surgical treatment of AO Foundation and Orthopaedic Trauma Association (AO/OTA) classification type 31-A2 pertrochanteric fractures.1) Studies have reported on the importance of posteromedial cortex in stability, and fractures with posteromedial cortical damage are regarded as unstable pertrochanteric fractures.2) Either dynamic hip screws or nails are used according to the surgeon's preference for posteromedial cortical defect. Numerous studies have described the difference in surgical outcomes between the two implants.345) Dynamic hip screws may cause over-sliding when posteromedial cortex is substantially damaged.6) To overcome this flaw, additional fixation methods can be applied to the posteromedial cortex.78) Compared to anatomical fixation, a slight valgus alignment can provide greater medial cortical support. Chang et al.9) have reported that among patients with AO/OTA type 31-A2 fractures, those with positive medial cortical support showed superior radiological and clinical results after surgery. However, no study has reported the surgical outcomes of dynamic hip screws contingent upon medial cortical support.
Our aim is to evaluate the radiological and clinical results of reduction using dynamic hip screws according to the grade of medial cortical support in patients with AO/OTA type 31-A2 fractures. In the management of unstable fractures due to posteromedial wall injury, we hypothesized that reduction with positive medial cortical support would enhance stability of the fractures and thus improve clinical outcomes.
Among patients who underwent surgery due to pertrochanteric fractures from January 1, 2010 through December 31, 2015, this retrospective study enrolled 100 patients with AO/OTA type 31-A2 fractures aged 60 or over who showed displaced lesser trochanteric fragments on the preoperative pelvis anteroposterior (AP) view and a cortical length of longer than 20 mm. This study was conducted after approval of the Institutional Review Board of Daegu Catholic University Medical Center (IRB No. CR17-138).
Among 354 patients who underwent surgery for pertrochanteric fractures between 2010 and 2015, 182 patients were classified as AO/OTA type 31-A2, with the cortical area including the lesser trochanter over 20 mm. Of the 182 patients, 122 were followed up for at least 1 year. Of the 122 patients, 103 were able to provide appropriate radiological data allowing for detailed analysis. Among them, 100 patients, aged 60 years or over, were ultimately enrolled in this study (Fig. 1).
Twenty-eight of the 100 patients underwent fixation using wires for stabilizing the posteromedial fragments, whereas 74 underwent fixation using the trochanter stabilizing plate (TSP) to prevent lateral wall damage. All patients showing lateral wall breakage on the preoperative radiograph were classified as AO/OTA type 31-A3 and were excluded from this study. After evaluation of the reduction status shown in C-arm fluoroscopy, we assigned patients with positive medial cortical support to group 1, patients with neutral medial cortical support to group 2, and patients with negative medial cortical support where the proximal medial cortex is formed more laterally than the distal medial cortex to group 3 (Fig. 2). Between the groups, there were no significant differences in age, sex, body mass index, follow-up duration, the pretrauma walking ability score of Ceder, and bone mineral density (BMD) of the opposite femoral neck assessed within 3 postoperative months (Table 1).
All surgeries were performed by a single surgeon (MRC). For fixation, 129° antihypersliding dynamic hip screws (Break Top System Compression Hip Screw; Solco, Pyeongtaek, Korea) and 135° dynamic hip screws (4CIS CHS System, Solco) were used. Under the guidance of C-arm fluoroscopy, lag screws were inserted and placed at the center of the femoral head, if possible, or were inserted on the posteroinferior side of the femoral head. Due to posteromedial damage in the pertrochanteric area, we tried to achieve anatomic reduction of the anteromedial cortex, the area where displacement was rather minimal.10) During surgery, we tried to compress the fracture site as much as possible using compression screws. Depending on the pre- or intraoperative decisions of the surgeon, wires or TSP were used.
Radiological evaluation was performed by two residents (JSD and JHL). The length of the posteromedial cortex, including the displaced lesser trochanter, was measured using the preoperative pelvis AP view (Fig. 3). Changes in the neck-shaft angle and the degree of lag screw sliding were evaluated using pelvis AP views. Radiographic errors were corrected by means of the error correction method of Doppelt.11) The degree of lag screw sliding was defined as the difference in the shortest distance from the end of the lag screw to the barrel between simple radiographs taken immediately after surgery and at the follow-up session during 1 to 3 years after surgery. A sliding of 15 mm or more was regarded as radiological failure and recorded as 15 mm sliding. The position of the lag screw within the femoral head shown on the postoperative radiograph was evaluated by means of the method by Kyle et al.12) The tip-apex distance, the sum of the values of the distance from the top of the femoral head to the end of the lag screw measured on AP and lateral views, was used to measure the depth of the inserted lag screw. BMD scans performed within the postoperative 3 months were also evaluated.
The gait of the patient was evaluated using the walking ability score suggested by Ceder et al.13) before trauma and at the follow-up session during 1 to 3 years after surgery.
A post-hoc test was performed for statistical analysis of the three groups divided by the grade of medial cortical support. The Bonferroni test was performed for intergroup evaluation of two groups among three groups. The Mann-Whitney test was also performed for evaluation of the radiological and clinical results of medal fixation and the use of TSP. A p-value ≤ 0.05 was considered to indicate statistical significance.
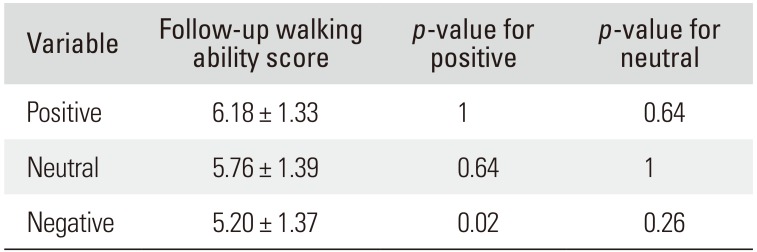
The intraclass correlation coefficients for radiological measurement were all above 0.8 (Table 2). The average length of the posteromedial cortex, including the displaced lesser trochanter, was 44.92 ± 13.53 mm on pelvis AP views. The BMD of the opposite femoral neck measured within 3 postoperative months showed a T-score of −2.40 ± 0.76. The average neck-shaft angle was 132.35° ± 4.92° at the initial postoperative measurement, and it was 127.22° ± 6.06° at the follow-up session during 1 to 3 years after surgery, showing a varus change of 5.13° ± 2.92° and the average lag screw sliding was 8.81 ± 4.41 mm. All 100 patients showed a tip-apex distance of less than 25 mm on the postoperative radiographs. Lag screws were located at the center in most cases; there was no case with the lag screw located superiorly. There were no significant differences in the neck-shaft angle and the lag screw sliding contingent upon the use of TSP or wire fixation of the posteromedial cortex (Table 3). After evaluation of the intraoperative reduction status using C-arm fluoroscopy, patients with positive medial cortical support were assigned to group 1, patients with neutral medial cortical support were assigned to group 2, and patients with negative medial cortical support where the proximal medial cortex is formed more laterally than the distal medial cortex, were assigned to group 3. The difference in the neck-shaft angle and lag screw sliding distance showed statistical significance (Table 4). Group 1 showed significantly less changes in the neck-shaft angle and shorter lag screw sliding distance than groups 2 and 3. Group 2 showed significantly less changes in the neck-shaft angle and shorter lag screw sliding distance than group 3. Among the 42 patients in group 2, 14 patients underwent additional posteromedial fixation, and 28 patients did not. Patients with additional posteromedial fixation showed significantly lower lag screw sliding (p = 0.02). The average walking ability score at the follow-up session during 1 to 3 years after surgery was 5.71 ± 1.40. Walking ability scores showed significant difference between the three groups (p = 0.00) (Table 5). The mean walking ability score of group 1 was significantly higher than group 3 (p = 0.00). There was no significant difference between groups 2 and 3.
In unstable pertrochanteric fractures, dynamic hip screws increase stability of the fracture site through sliding of the proximal fragment and impaction of the fracture site and thus induce bone union. Due to the impaction of the proximal fragment, the moment arm decreases, and in turn, the weight bearing stress decreases, improving stability of the fracture site.1415) However, due to excessive sliding of the lag screw, complications might occur including nonunion, malunion, perforation of the femoral head, fixation failure, leg shortening, and breakage of the fixture.616)
Such complications are more common in unstable fractures. Thus, stability assessment of a pertrochanteric fracture plays a crucial role in determining prognosis and surgical techniques. In our study, we considered fractures with a posteromedial cortical length of 20 mm or over as unstable AO/OTA type 31-A2 fractures and included for analysis in this study.
Several studies have already considered the sliding distance of the lag screw as the indicator of stability in pertrochanteric fractures, and have reported the values of lag screw sliding after the treatment of unstable pertrochanteric fractures. Jacobs et al.17) reported the average lag screw sliding was 5.3 mm in stable fractures and 15.7 mm in unstable fractures. Larsson et al.18) reported the value was 6.3 mm in stable fractures and 12.4 mm in unstable fractures. Steinberg et al.19) reported that lag screw sliding of 15 mm or over results in the increase in failure rates. Kim et al.20) observed leg shortening and femoral pain in patients with lag screw sliding of 20 mm or over. In our study, we defined sliding of 15 mm or more as radiological failure, and such cases were recorded as 15 mm sliding. Among 17 patients that showed a sliding of 15 mm, two patients of 28 were in group 1, nine patients of 42 in group 2, and six patients of 30 in group 3. In other words, patients with positive medial cortical support showed a lower failure rate. All patients enrolled in this study were patients with unstable pertrochanteric fractures, and the average lag screw sliding distance was 8.81 ± 4.41 mm, which is a rather smaller value than that in previous studies. In particular, patients with positive medial cortical support showed an average lag screw sliding distance of 5.82 ± 4.18 mm, which may indicate that positive medial cortical reduction contributes to increased stability in pertrochanteric fractures.
During the management of pertrochanteric fractures using dynamic hip screws, compression on the fracture site occurs in two situations. Firstly, compression is applied to the bone fragments during operation to provide stability to the fracture site. In this study, 30 of 100 patients (30%) had negative medial cortical support. Although we aimed to achieve anatomic reduction during surgery, due to the posteromedial cortical bone defect, fractures were unstable, and thus much more pressure was applied to the fracture site. The percentage of patients with negative medial cortical support, which was 30, is thought to be attributable to the excessive compression to the axial plane of the lag screw. Secondly, compression also occurs due to the patient's body weight. In order to prevent this, when using dynamic hip screws, surgeons use various techniques such as additional fixation to the posteromedial portion or TSP.821) In our study, with a single technique, the positive medial cortical support group (group 1) showed statistically significant superiority in radiographic evaluation, compared with the other groups. Additional fixation to the posteromedial portion and TSP resulted in no significant difference. We think reduction with positive medial cortical support would prevent undesirable sliding, playing a role as a cortical block.
The goal in the treatment of pertrochanteric fractures is to restore ambulatory function. Ingemarsson et al.22) have reported that recovery of the gait must be evaluated after at least a year after surgery. Accordingly, we evaluated the degree of gait at the follow-up session during 1 to 3 years after surgery.
This study has several limitations. Firstly, it was conducted retrospectively. Secondly, due to the low follow-up rate of the patients, selection bias might have occurred. Thirdly, the follow-up period was between 1 and 3 years after surgery, which only reflects short-term postoperative results. However, considering the advanced age of the patients (over 60 years) and the high 1-year mortality rate of pertrochanteric fractures, longer follow-up results could be difficult to obtain. When treating pertrochanteric fractures accompanied by posteromedial wall defect using dynamic hip screw, negative cortical support should be avoided.
References
1. Marmor M, Liddle K, Pekmezci M, Buckley J, Matityahu A. The effect of fracture pattern stability on implant loading in OTA type 31-A2 proximal femur fractures. J Orthop Trauma. 2013; 27(12):683–689. PMID: 23412511.

2. Knobe M, Gradl G, Ladenburger A, Tarkin IS, Pape HC. Unstable intertrochanteric femur fractures: is there a consensus on definition and treatment in Germany? Clin Orthop Relat Res. 2013; 471(9):2831–2840. PMID: 23389806.

3. Parker MJ, Pryor GA. Gamma versus DHS nailing for extracapsular femoral fractures: meta-analysis of ten randomised trials. Int Orthop. 1996; 20(3):163–168. PMID: 8832319.
4. Anglen JO, Weinstein JN. American Board of Orthopaedic Surgery Research Committee. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am. 2008; 90(4):700–707. PMID: 18381305.
5. Saudan M, Lubbeke A, Sadowski C, Riand N, Stern R, Hoffmeyer P. Pertrochanteric fractures: is there an advantage to an intramedullary nail? A randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma. 2002; 16(6):386–393. PMID: 12142826.
6. Madsen JE, Naess L, Aune AK, Alho A, Ekeland A, Stromsoe K. Dynamic hip screw with trochanteric stabilizing plate in the treatment of unstable proximal femoral fractures: a comparative study with the Gamma nail and compression hip screw. J Orthop Trauma. 1998; 12(4):241–248. PMID: 9619458.

7. Jones JB. Screw fixation of the lesser trochanteric fragment. Clin Orthop Relat Res. 1977; (123):107.

8. Cho SH, Lee SH, Cho HL, Ku JH, Choi JH, Lee AJ. Additional fixations for sliding hip screws in treating unstable pertrochanteric femoral fractures (AO Type 31-A2): short-term clinical results. Clin Orthop Surg. 2011; 3(2):107–113. PMID: 21629470.

9. Chang SM, Zhang YQ, Ma Z, Li Q, Dargel J, Eysel P. Fracture reduction with positive medial cortical support: a key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch Orthop Trauma Surg. 2015; 135(6):811–818. PMID: 25840887.

10. Carr JB. The anterior and medial reduction of intertrochanteric fractures: a simple method to obtain a stable reduction. J Orthop Trauma. 2007; 21(7):485–489. PMID: 17762483.

11. Doppelt SH. The sliding compression screw: today's best answer for stabilization of intertrochanteric hip fractures. Orthop Clin North Am. 1980; 11(3):507–523. PMID: 7413172.
12. Kyle RF, Gustilo RB, Premer RF. Analysis of six hundred and twenty-two intertrochanteric hip fractures. J Bone Joint Surg Am. 1979; 61(2):216–221. PMID: 422605.

13. Ceder L, Lindberg L, Odberg E. Differentiated care of hip fracture in the elderly: mean hospital days and results of rehabilitation. Acta Orthop Scand. 1980; 51(1):157–162. PMID: 6246706.
14. Schumpelick W, Jantzen PM. A new principle in the operative treatment of trochanteric fractures of the femur. J Bone Joint Surg Am. 1955; 37-A(4):693–698. PMID: 13242603.

15. Clawson DK. Trochanteric fractures treated by the sliding screw plate fixation method. J Trauma. 1964; 4:737–752. PMID: 14225321.

16. Ecker ML, Joyce JJ 3rd, Kohl EJ. The treatment of trochanteric hip fractures using a compression screw. J Bone Joint Surg Am. 1975; 57(1):23–27. PMID: 1123368.

17. Jacobs RR, Armstrong HJ, Whitaker JH, Pazell J. Treatment of intertrochanteric hip fractures with a compression hip screw and a nail plate. J Trauma. 1976; 16(08):599–603. PMID: 957454.

18. Larsson S, Friberg S, Hansson LI. Trochanteric fractures: influence of reduction and implant position on impaction and complications. Clin Orthop Relat Res. 1990; (259):130–139.
19. Steinberg GG, Desai SS, Kornwitz NA, Sullivan TJ. The intertrochanteric hip fracture: a retrospective analysis. Orthopedics. 1988; 11(2):265–273. PMID: 3357844.

20. Kim WY, Han CH, Park JI, Kim JY. Failure of intertrochanteric fracture fixation with a dynamic hip screw in relation to pre-operative fracture stability and osteoporosis. Int Orthop. 2001; 25(6):360–362. PMID: 11820441.

21. Hsu CE, Chiu YC, Tsai SH, Lin TC, Lee MH, Huang KC. Trochanter stabilising plate improves treatment outcomes in AO/OTA 31-A2 intertrochanteric fractures with critical thin femoral lateral walls. Injury. 2015; 46(6):1047–1053. PMID: 25890863.

22. Ingemarsson AH, Frandin K, Mellstrom D, Moller M. Walking ability and activity level after hip fracture in the elderly: a follow-up. J Rehabil Med. 2003; 35(2):76–83. PMID: 12691337.
Fig. 1
Flowchart of patient selection. AO/OTA: AO Foundation and Orthopaedic Trauma Association classification, DHS: dynamic hip screw, LT: lesser trochanter.

Fig. 2
(A) Reduction with positive medial cortical support. (B) Reduction with neutral medial cortical support. (C) Reduction with negative medial cortical support.
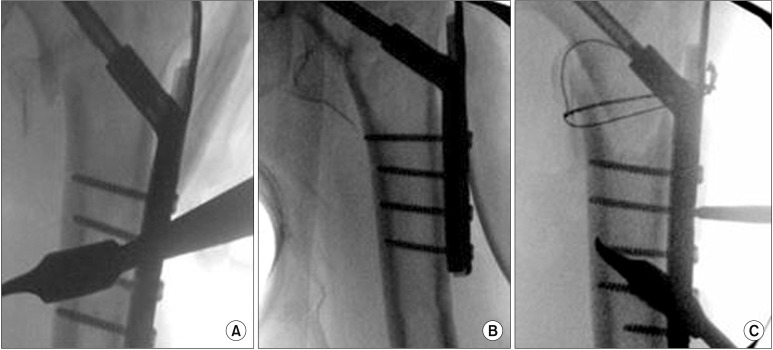
Fig. 3
The length of the posteromedial cortex (arrow), including the displaced lesser trochanter, measured on the preoperative pelvis anteroposterior view was ≥ 20 mm for inclusion in the study.

Table 1
Patient Characteristics
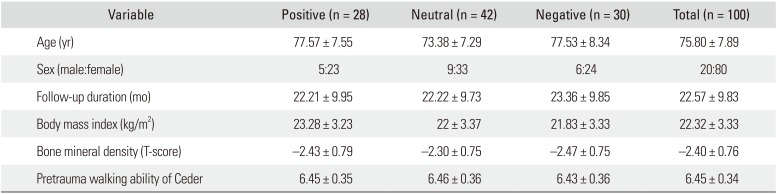
Table 2
Intra- and Interobserver Reliability of Radiographic Evaluation
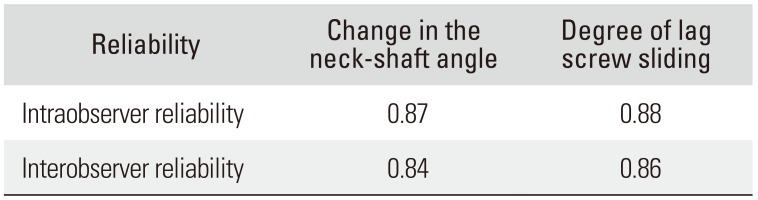
| Reliability | Change in the neck-shaft angle | Degree of lag screw sliding |
|---|---|---|
| Intraobserver reliability | 0.87 | 0.88 |
| Interobserver reliability | 0.84 | 0.86 |
Table 3
Radiological Results According to the Method of Additional Fixation (Wire/TSP)
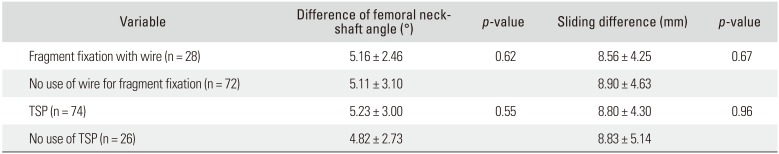
Table 4
Radiological Results According to Grade of Medial Cortical Support




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download