Abstract
Background
Our goal was to determine whether postoperative delirium is associated with inpatient complication rates after primary elective total hip arthroplasty (THA).
Methods
Using the National Inpatient Sample, we analyzed records of patients who underwent primary elective THA from 2000 through 2009 to identify patients with delirium (n = 13,551) and without delirium (n = 1,992,971) and to assess major perioperative complications (acute renal failure, death, myocardial infarction, pneumonia, pulmonary embolism, and stroke) and minor perioperative complications (deep vein thrombosis, dislocation, general procedural complication, hematoma, seroma, and wound infection). Patient age, sex, length of hospital stay, and number of comorbidities were assessed. We used multivariate logistic regression to determine the association of delirium with complication rates (significance, p < 0.01).
Results
Patients with delirium were older (mean, 75 ± 0.2 vs. 65 ± 0.1 years), were more likely to be male (56% vs. 52%), had longer hospital stays (mean, 5.7 ± 0.07 vs. 3.8 ± 0.02 days), and had more comorbidities (mean, 2.8 ± 0.03 vs. 1.4 ± 0.01) (all p < 0.001) versus patients without delirium. Patients with delirium were more likely to have major (11% vs. 3%) and minor (17% vs. 7%) perioperative complications versus patients without delirium (both p < 0.001). When controlling for age, sex, and number of comorbidities, delirium was independently associated with major and minor complications (odds ratio, 2.0; 95% confidence interval, 1.7 to 2.3).
Postoperative delirium has been shown to be associated with higher risk of death,1234) functional decline,56) and cognitive decline,57) as well as longer hospitalization8) and higher cost of care.910) Older patients are at especially high risk for postoperative delirium, which is often unrecognized and may be inadequately treated.8) Given the association between osteoarthritis and age, a substantial proportion of patients who undergo elective total hip arthroplasty (THA) are elderly and at high risk for postoperative delirium.89) In addition to age, postoperative pain has also been shown to be a risk factor for delirium in orthopaedic patients.9) The reported incidence of delirium after THA ranges from 7% to 17%.89)
The literature on total joint arthroplasty patients with delirium does not include any large-scale clinical studies.58) Marcantonio et al.3) showed that delirium after orthopaedic surgery was associated with higher rates of death and decreased functional outcome. Gottesman et al.1) reported similar findings in patients undergoing cardiac surgery. It is important to characterize the postoperative complications associated with delirium and to identify characteristics associated with postoperative delirium to optimize quality of care in arthroplasty patients.
The goals of our study were (1) to compare the demographic characteristics of patients with delirium after primary, elective THA with those of patients who did not have delirium; (2) to compare acute perioperative complication rates of patients with delirium after primary, elective THA with those of patients who did not have delirium; and (3) to determine whether there are any associations between specific comorbidities and delirium. We hypothesized that patients with postoperative delirium would have higher rates of major complications (including death) and minor complications compared with patients without postoperative delirium.
We searched the National Inpatient Sample (NIS) database for patients who underwent primary THA from 2000 through 2009. The NIS database includes discharge information from a 20% stratified sample of U.S. hospitals and patient information for all payers. The sampling methodology is reported to capture 97% of U.S. hospital discharges.11) Discharge weights were used to scale the NIS data to represent the general U.S. population. Our Institutional Review Board deemed this study to be exempt from approval.
All patients with an International Classification of Diseases, ninth revision, Clinical Modification (ICD-9-CM) procedure code for primary THA (code 81.51 or 81.52) were candidates for inclusion.12) We excluded patients who had a hip or lower extremity fracture, were admitted through the emergency department, were transferred from another hospital, or had acute or chronic osteomyelitis, malignancy, or pathologic fracture to select for a purely elective primary arthroplasty population. Of the hospital discharges for 3,316,928 THA cases, 1,310,406 cases were excluded. The remaining 2,006,522 cases formed our study group. These patients were divided into two subgroups: (1) those who had been diagnosed with delirium (ICD-9-CM codes 293.0, 291.1, 290.41, 292.81) and (2) those who were not diagnosed with delirium. We included all subtypes of delirium as each patient had been diagnosed with delirium in this study because our patient population (from the NIS) only included patients in the postoperative period. Patients diagnosed with delirium represented 0.68% (n = 13,551) of all primary THA patients.
We extracted data on patient age, sex, race, hospital charges, and comorbidities (Table 1). Race was identified as black, white, other (Hispanic, Asian, and Native American were combined in this category), or missing. Comorbidities were classified according to the Elixhauser coding schematic described by Quan et al.13) Length of hospitalization and total charges were evaluated as continuous variables. We searched the database for the following complications by ICD-9-CM code: acute renal failure, death, deep vein thrombosis, hip dislocation, general procedural complication, hematoma, myocardial infarction, pneumonia, pulmonary embolism, seroma, stroke, and wound infection.
Descriptive statistics with standard errors for continuous variables were used for analyzing complications, demographic characteristics, hospital charges, and length of hospitalization. Student t-tests were used for continuous variables, and chi-square tests were used for categorical variables. Significance was set at p < 0.01. Univariate and multivariate logistic regression models were constructed to assess the association of delirium with major and minor perioperative complications. All subtypes of delirium (i.e., alcohol withdrawal, drug-induced, acute, subacute, presenile, senile, and vascular) were included in pooled analysis. Major complications were defined as acute renal failure, death, myocardial infarction, pneumonia, pulmonary embolism, and stroke. Minor complications were defined as deep vein thrombosis, hip dislocation, general procedural complication, hematoma, seroma, and wound infection. Descriptive statistics for the association of the major Elixhauser comorbidities (i.e., cardiac arrhythmias, chronic pulmonary disease, congestive heart failure, liver disease, obesity, weight loss, and peripheral vascular disease) and delirium with death and complications were assessed (as multivariate odds ratios [ORs] with 95% confidence intervals [CIs]). Statistical analysis was performed using Stata ver. 10 (Stata Corp., College Station, TX, USA).
Patients with delirium after primary elective THA were older (mean age, 75 ± 0.2 vs. 65 ± 0.1 years, p < 0.001), more likely to be male (56% vs. 52%, p < 0.001), and less likely to be black (3.3% vs. 4.4%, p = 0.002) or “other” race (2.7% vs. 4.4%, p < 0.001) versus patients without delirium (Table 1). Data on race were missing in equally high proportions in both groups (for 28% of patients with delirium and 27% of patients without delirium).
According to multivariate analysis, the following comorbidities were significantly associated with the risk of perioperative delirium: history of drug abuse, history of alcohol abuse, weight loss, fluid or electrolyte abnormality, neurologic disorder, psychosis, coagulopathy, congestive heart failure, depression, cardiac arrhythmia, and diabetes with known medical complications (Table 2).
Compared with patients without delirium, those with delirium had longer hospitalizations (mean, 5.7 ± 0.07 vs. 3.8 ± 0.02 days; p < 0. 001); higher charges (mean, $46,153 ± $885 vs. $38,287 ± $486; p < 0.001); and more comorbidities (mean, 2.8 ± 0.03 vs. 1.4 ± 0.01; p < 0.001). Multivariate logistic regression using number of comorbidities, age, and sex as covariates showed that delirium was independently associated with major and minor perioperative complications (OR, 2.0; 95% CI, 1.7 to 2.3).
Compared with patients without delirium, those with delirium were more likely to have major perioperative complications according to a pooled analysis (Table 3). Univariate analysis also showed associations of delirium with acute renal failure, death, myocardial infarction, pneumonia, and pulmonary embolism. On multivariate analysis, death, pulmonary embolism, and stroke were not independently associated with delirium.
Compared with patients without delirium, those with delirium were more likely to have minor perioperative complications. On univariate analysis, hip dislocation, general complications, and wound infection were associated with delirium (Table 3). All of these factors were found to be associated with delirium independently on multivariate analysis.
Using data from the NIS from 2000 through 2009, we found associations of postoperative delirium with perioperative major and minor complications and death after primary, elective THA. Patients who experienced delirium after THA were older, were more likely to be male, had longer hospitalizations, had higher overall hospital charges, and had more comorbidities. Alcohol abuse is strongly associated with delirium in primary THA patients (observed in 5% of patients with delirium vs. 0.7% of patients who did not develop delirium). Prior studies have shown that alcohol abuse is associated with significantly higher risk for worse perioperative outcomes after arthroplasty surgery;14) however, Jankowski et al.5) suggested that alcohol abuse is not associated with postoperative delirium. They performed a rigorous analysis using the confusion assessment method, which takes approximately 55 minutes to complete. Because of this, it is possible that they were able to identify patients with more subtle delirium that may not have been recognized or appropriately diagnosed in our patient population—and that patients diagnosed with delirium in our study had more profound delirium. Therefore, the association with alcohol abuse might apply only to profound delirium after THA. No studies describe the relationship between duration of sobriety and risk of postoperative delirium, which would be important information for patient counseling when discussing the risks and benefits of THA.
Drug abuse is also strongly associated with delirium in primary THA patients (Table 2); however, the OR in our study may be artificially high because of statistical overfitting in our model or skewing due to differences in sample size. Prior literature has shown that history of drug abuse significantly increases the risk for postoperative delirium in patients undergoing orthopaedic surgery.15) Additionally, a prior study has found that patients with a history of drug abuse are at significantly greater risk of postoperative complications.16) In our study, we found that history of drug abuse was the strongest risk factor for postoperative delirium (Table 2).
Mental illnesses such as psychosis and depression were also found to be associated with delirium after THA surgery. Psychosis and depression (Table 2) were associated with an increased risk of postoperative delirium. Similar to a study by Stundner et al.,17) our study showed a higher risk of postoperative delirium in patients with depression and anxiety. Our findings are consistent with this literature;17181920) however, as described, Jankowski et al.5) found that depression was not associated with postoperative delirium. Again, because of their rigorous diagnostic method, it is possible that they were able to identify patients with more subtle delirium that may not have been recognized or appropriately diagnosed in our patient population, and that patients diagnosed with delirium in our study had more profound delirium. Therefore, depression may be associated with more profound postoperative delirium.
When using multivariate regression, our study showed higher rates of postoperative delirium in patients with cardiac arrhythmias, coagulopathy, congestive heart failure, diabetes with known medical complications, and fluid and electrolyte disorders. These medical comorbidities have been shown to be associated with increased rates of delirium in patients in previous studies, and our findings are consistent with this (Table 2).5818192021)
Berstock et al.22) investigated acute perioperative death after THA and found a 30-day mortality rate of 0.30% and a 90-day mortality rate of 0.65%. We found an inpatient mortality rate of 0.13% for THA patients. Of note, our study found that patients who experienced postoperative delirium were more than four times as likely to die during the same admission (0.55% vs. 0.13%, p < 0.001) versus patients without delirium; however, on multivariate analysis, delirium was not an independent risk factor for death (OR, 1.01; 95% CI, 0.48 to 2.13).
Delirium is a complex syndrome that is likely the manifestation of several intertwined mechanisms without a distinct pathophysiology. We sought to identify some of the comorbidities associated with postoperative delirium. We also sought to determine the association of delirium with perioperative complications in primary elective THA patients. A limitation of this study is that any patient with a history of alcohol abuse is included in this analysis, including those who have sought treatment and are separated from their most recent use by several years. Further, the temporal relationship between complications and onset of delirium is unable to be established in an administrative database. Therefore, we can say with certainty only that there is an association because delirium may have caused the complication or the complication may have caused delirium. The limitations of our study are related to the use of the NIS database, which records administrative data for only the duration of the initial hospitalization. Administrative databases have been shown to have varying levels of reliability depending on the comorbidity.23) Further, some comorbidities have subjective definitions, such as weight loss.13) Long-term outcomes after discharge, which are an important metric for THA, cannot be evaluated using the NIS. Another limitation is the completeness of the data in the NIS. Previous analysis has shown that the information coded in the NIS is reasonably accurate, with a specificity of more than 92%, but it may not be complete.24) Studies have shown that postoperative delirium is often underdiagnosed.25) In our study, it is likely that postoperative delirium was underdiagnosed because an incidence of 0.68% is substantially lower than that reported in more rigorous studies.589) Prior studies have suggested that the incidence is between 7% to 17%, although these studies use methods for diagnosing delirium that are extremely time intensive and likely capable of identifying more subtle and less severe cases of delirium.589) Additionally, these are smaller studies that may not be reflective of an entire population. In our study, we likely did not identify all patients with delirium; however, the NIS has the major advantage of being the largest available administrative database that includes all payers. For patient subsets in which there are few cases at single or even multiple institutions such as patients with delirium, the NIS database is an excellent tool for providing a large sample size to determine incidence of relatively rare outcomes such as inpatient death. According to our findings, there is an association between delirium and perioperative morbidity and mortality in primary hip arthroplasty patients. Elective THA should be approached with caution after a thorough evaluation of comorbidities and with shared decision-making with the patient regarding the substantial risks.
Primary THA patients with postoperative delirium are at significantly higher risk of acute perioperative inpatient complications than those without delirium. Specific comorbidities and demographic characteristics are strongly associated with delirium. Elective THA should be approached with caution after careful consideration of comorbidities and risk factors. Understanding these factors can aid in preoperative counseling and allow patients to participate in a shared decision-making process.
References
1. Gottesman RF, Grega MA, Bailey MM, et al. Delirium after coronary artery bypass graft surgery and late mortality. Ann Neurol. 2010; 67(3):338–344. PMID: 20373345.

2. Lalmohamed A, Vestergaard P, de Boer A, Leufkens HG, van Staa TP, de Vries F. Changes in mortality patterns following total hip or knee arthroplasty over the past two decades: a nationwide cohort study. Arthritis Rheumatol. 2014; 66(2):311–318. PMID: 24504803.

3. Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001; 49(5):516–522. PMID: 11380742.

4. Sampson EL, Raven PR, Ndhlovu PN, et al. A randomized, double-blind, placebo-controlled trial of donepezil hydrochloride (Aricept) for reducing the incidence of postoperative delirium after elective total hip replacement. Int J Geriatr Psychiatry. 2007; 22(4):343–349. PMID: 17006875.

5. Jankowski CJ, Trenerry MR, Cook DJ, et al. Cognitive and functional predictors and sequelae of postoperative delirium in elderly patients undergoing elective joint arthroplasty. Anesth Analg. 2011; 112(5):1186–1193. PMID: 21415433.

6. Rudolph JL, Inouye SK, Jones RN, et al. Delirium: an independent predictor of functional decline after cardiac surgery. J Am Geriatr Soc. 2010; 58(4):643–649. PMID: 20345866.

7. Saczynski JS, Marcantonio ER, Quach L, et al. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012; 367(1):30–39. PMID: 22762316.

8. Bin Abd Razak HR, Yung WY. Postoperative delirium in patients undergoing total joint arthroplasty: a systematic review. J Arthroplasty. 2015; 30(8):1414–1417. PMID: 25818653.

9. Scott JE, Mathias JL, Kneebone AC. Incidence of delirium following total joint replacement in older adults: a meta-analysis. Gen Hosp Psychiatry. 2015; 37(3):223–229. PMID: 25774049.

10. Postler A, Neidel J, Gunther KP, Kirschner S. Incidence of early postoperative cognitive dysfunction and other adverse events in elderly patients undergoing elective total hip replacement (THR). Arch Gerontol Geriatr. 2011; 53(3):328–333. PMID: 21288579.

11. Healthcare Cost and Utilization Project. Overview of the National (Nationwide) Inpatient Sample (NIS) [Internet]. Rockville, MD: Agency for Healthcare Research and Quality;2014. cited 2018 Jun 18. Available from: http://www.hcup-us.ahrq.gov/nisoverview.jsp.
12. Centers for Disease Control and Prevention. International Classification of Diseases, ninth revision, Clinical Modification (ICD-9-CM) [Internet]. Atlanta, GA: Centers for Disease Control and Prevention;cited 2018 Jun 18. Available from: https://www.cdc.gov/nchs/icd/icd9cm.htm.
13. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43(11):1130–1139. PMID: 16224307.

14. Best MJ, Buller LT, Gosthe RG, Klika AK, Barsoum WK. Alcohol misuse is an independent risk factor for poorer postoperative outcomes following primary total hip and total knee arthroplasty. J Arthroplasty. 2015; 30(8):1293–1298. PMID: 25769745.

15. Fineberg SJ, Nandyala SV, Marquez-Lara A, Oglesby M, Patel AA, Singh K. Incidence and risk factors for postoperative delirium after lumbar spine surgery. Spine (Phila Pa 1976). 2013; 38(20):1790–1796. PMID: 23797502.

16. Best MJ, Buller LT, Klika AK, Barsoum WK. Outcomes following primary total hip or knee arthroplasty in substance misusers. J Arthroplasty. 2015; 30(7):1137–1141. PMID: 25765129.

17. Stundner O, Kirksey M, Chiu YL, et al. Demographics and perioperative outcome in patients with depression and anxiety undergoing total joint arthroplasty: a population-based study. Psychosomatics. 2013; 54(2):149–157. PMID: 23194934.

18. Nandi S, Harvey WF, Saillant J, Kazakin A, Talmo C, Bono J. Pharmacologic risk factors for post-operative delirium in total joint arthroplasty patients: a case-control study. J Arthroplasty. 2014; 29(2):268–271. PMID: 23831083.

19. Priner M, Jourdain M, Bouche G, Merlet-Chicoine I, Chaumier JA, Paccalin M. Usefulness of the short IQCODE for predicting postoperative delirium in elderly patients undergoing hip and knee replacement surgery. Gerontology. 2008; 54(2):116–119. PMID: 18285677.

20. Radcliff KE, Orozco FR, Quinones D, Rhoades D, Sidhu GS, Ong AC. Preoperative risk stratification reduces the incidence of perioperative complications after total knee arthroplasty. J Arthroplasty. 2012; 27(8 Suppl):77–80. 80.e1–80.e8. PMID: 22682037.

21. Rade MC, Yadeau JT, Ford C, Reid MC. Postoperative delirium in elderly patients after elective hip or knee arthroplasty performed under regional anesthesia. HSS J. 2011; 7(2):151–156. PMID: 22754416.

22. Berstock JR, Beswick AD, Lenguerrand E, Whitehouse MR, Blom AW. Mortality after total hip replacement surgery: a systematic review. Bone Joint Res. 2014; 3(6):175–182. PMID: 24894596.
23. Rattanaumpawan P, Wongkamhla T, Thamlikitkul V. Accuracy of ICD-10 coding system for identifying comorbidities and infectious conditions using data from a Thai University Hospital Administrative Database. J Med Assoc Thai. 2016; 99(4):368–373. PMID: 27396219.
24. Bozic KJ, Bashyal RK, Anthony SG, Chiu V, Shulman B, Rubash HE. Is administratively coded comorbidity and complication data in total joint arthroplasty valid? Clin Orthop Relat Res. 2013; 471(1):201–205. PMID: 22528384.

25. Neufeld KJ, Nelliot A, Inouye SK, et al. Delirium diagnosis methodology used in research: a survey-based study. Am J Geriatr Psychiatry. 2014; 22(12):1513–1521. PMID: 24745562.

Table 1
Demographic Characteristics of Patients with Primary Elective Total Hip Arthroplasty According to Postoperative Delirium Status (National Inpatient Sample, 2000–2009)
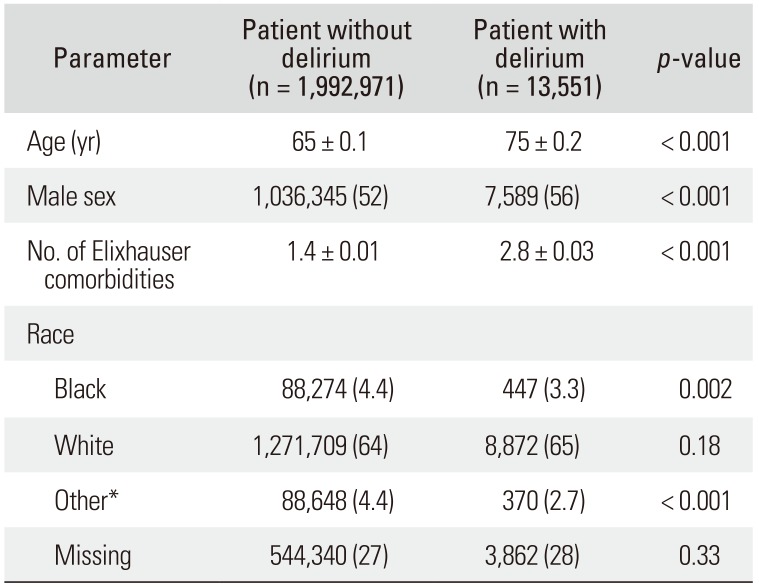
Table 2
Odds of Developing Delirium after Primary Elective Total Hip Arthroplasty According to Multivariate Analysis of Comorbidities and Risk Factors (National Inpatient Sample, 2000–2009)
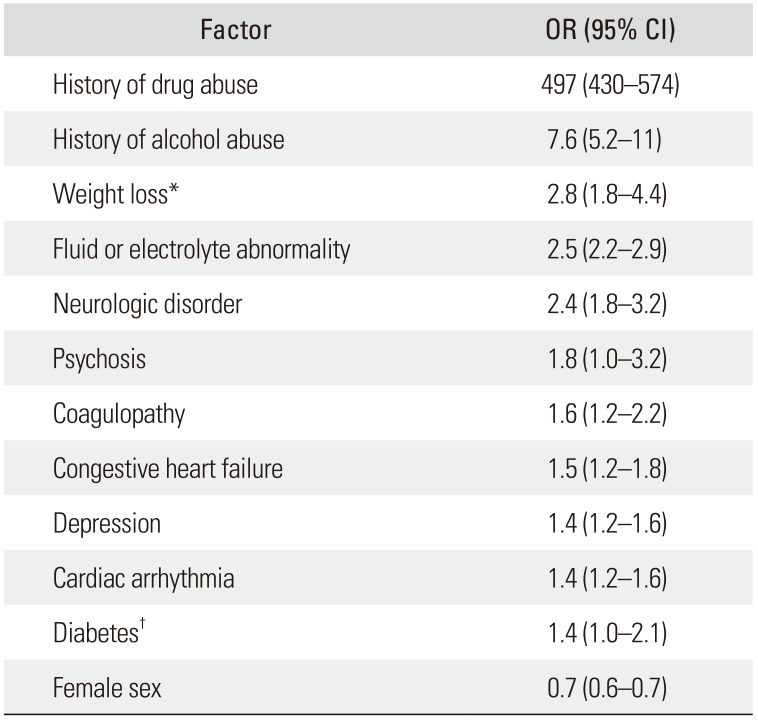
Table 3
Perioperative Inpatient Complications of Primary Elective Total Hip Arthroplasty According to Postoperative Delirium Status (National Inpatient Sample, 2000–2009)
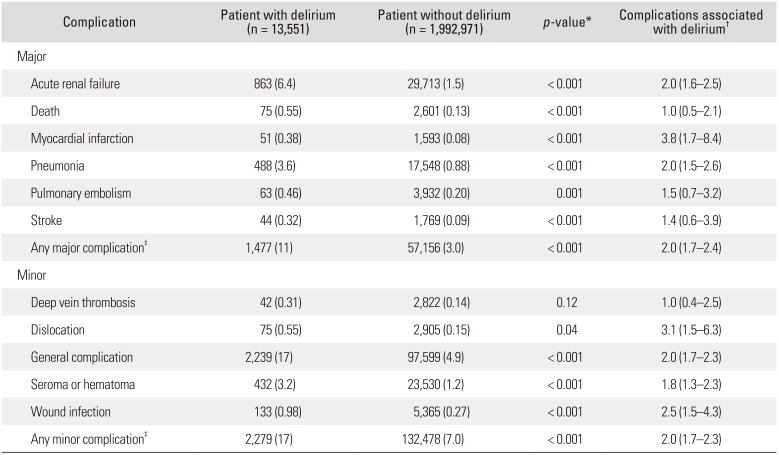
Values are presented as number (%) or odds ratio (95% confidence interval).
*By univariate analysis. †By multivariate analysis using patient age, sex, and number of Elixhauser comorbidities as covariates. ‡Patients with more than one complication are counted only once in the aggregate complication categories.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download