Abstract
Background
Displaced anterior column fractures have increasingly been treated surgically by the ilioinguinal approach and fixation with lag screws and a buttress plate on the pelvic brim. However, a major disadvantage of the ilioinguinal approach is possible damage to the neurovascular bundle and the lymphatic structures in the intermediate part of the approach. This study aims to present a novel surgical technique of the less invasive anterior iliac approach and compression osteosynthesis for high anterior column fractures of the acetabulum.
Methods
In this retrospective case series, 19 patients treated operatively for isolated high anterior column fractures using the less invasive anterior iliac approach and compression osteosynthesis were included. Patient demographics, the cause of injury, associated injuries, time to surgical reconstruction, and operation time were collected from the medical records. The quality of reduction was assessed by postoperative standard radiographic views and computed tomography scans and graded according to Matta's criteria. Clinical and radiographic grades were assessed according to Matta's criteria at the last follow-up.
Results
This less invasive surgical technique was successful for reduction and fixation in all high anterior column fractures and provided sufficient stability to allow immediate mobilization of the patients after surgery. Twelve fractures were combined with the quadrilateral plate fracture and seven fractures did not involve the quadrilateral plate. According to Matta's criteria, anatomical reduction was obtained in 17 patients and imperfect reduction in two patients. Clinical results were excellent in 17 patients and good in two patients. Radiographic results were excellent in 17 patients and good in two patients. Ten patients had neurapraxia of the lateral femoral cutaneous nerve related to the approach, which was resolved completely in seven. One patient had deep vein thrombosis.
Conclusions
Our less invasive surgical technique of the anterior iliac approach and compression osteosynthesis is a useful addition to the existing techniques in the treatment of high anterior column fractures of the acetabulum. Despite being a limited approach and fixation, this technique provides sufficient exposure for reducing and fixing the fracture and adequate stability to allow immediate mobilization of the patient after surgery.
An isolated anterior column fracture is a rare injury that accounts for 3%–6.3% of total acetabular fractures.123) Although conservative treatment has shown good results for anterior column fractures with adequate reduction of the femoral head beneath the weight-bearing dome,4) in recent years, displaced anterior column fractures have increasingly been treated surgically by the ilioinguinal approach and fixation with lag screws and a buttress plate on the pelvic brim.5) However, a major disadvantage of the ilioinguinal approach is possible damage to the neurovascular bundle and the lymphatic structures in the intermediate part of the approach. To prevent these complications, the modified Stoppa approach, alone or in combination with the lateral window of the ilioinguinal approach, has been advocated for use.6789) The minimally invasive approach can reduce the risk of developing complications associated with the classic ilioinguinal approach; however, it also has the risk of bleeding from the corona mortise and inguinal hernia.
Because of these risks, we developed a less invasive surgical technique, the anterior iliac approach and compression osteosynthesis, for the treatment of high anterior column fractures. The anterior iliac approach is almost the same as the use of a lateral window in the classic ilioinguinal approach and compression osteosynthesis is achieved by interfragmentary compression using lag screw(s) and a plate. The objective of this study is to describe the surgical technique and investigate the clinical and radiographic outcomes of this novel less invasive anterior iliac approach and compression osteosynthesis for high anterior column fractures of the acetabulum.
We conducted this study in compliance with the principles of the Declaration of Helsinki. The protocol of this study was reviewed and approved by the Institutional Review Board of Daegu Fatima Hospital (IRB No. DFE17ORIO021). Between 2006 and 2015, 19 consecutive patients with an isolated high anterior column fracture were treated by a less invasive anterior iliac approach, which is almost the same as the lateral window of the classic ilioinguinal approach, and compression osteosynthesis. Patients who had associated fractures such as T-shaped fractures, anterior column and posterior hemitransverse fractures, and both-column fractures were excluded from the study.
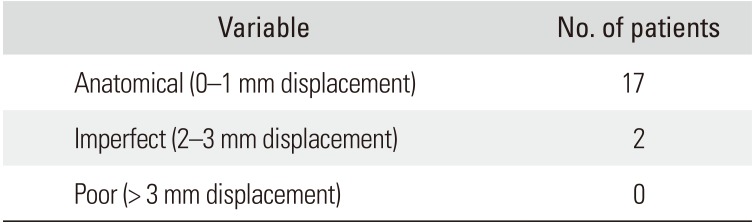
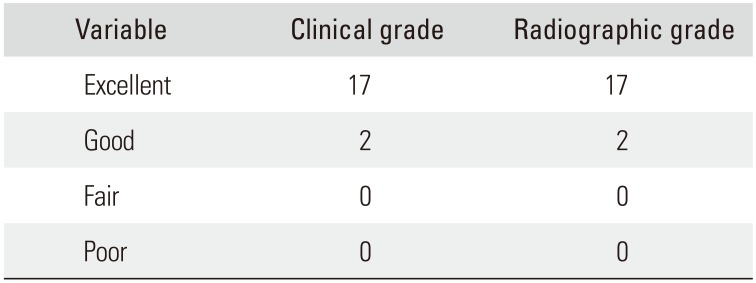
Patient demographics, the cause of injury, associated injuries, time to surgical reconstruction, and operation time were collected from the medical records. Three standard radiographs (anteroposterior, iliac oblique, and obturator oblique views) and computed tomography (CT) scans were used to clarify the fracture pattern and displacement of fracture fragments. The quality of fracture reduction was assessed by postoperative standard radiographic views and CT scans and graded as anatomical (displacement, 0–1 mm), imperfect (displacement, 2–3 mm), and poor (displacement, > 3 mm) according to Matta's criteria.2) Patients were prospectively followed up at 1, 2, 3, 6, and 12 months after surgery. None of the patients was lost to follow up. During the follow-up, standard radiographs were obtained and clinical findings such as pain, walking, the range of motion of both hips, and the level of activity were examined. Clinical and radiographic grades were assessed according to Matta's criteria at the last follow-up.2) Data on postoperative complications including infection, neurovascular injury, heterotopic ossification, loss of reduction, deep vein thrombosis, and posttraumatic osteoarthritis of the hip were also retrieved.
The patient is placed supine on a radiolucent operating table to allow for intraoperative manipulation of the affected lower extremity. The fracture is exposed through the anterior iliac approach, which is almost the same as the lateral window of the classic ilioinguinal approach (Fig. 1). The incision starts at the junction of posterior and middle third of the iliac crest, curves toward the anterior superior iliac spine, and ends 1–2 inches medial to the anterior superior iliac spine. The lateral femoral cutaneous nerve is exposed and protected. The iliopectineal fascia is detached from the iliopectineal eminence to place a buttress plate and to insert an infra-acetabular screw. Complete, displaced fractures of the iliac wing are reduced and fixed first with a long screw or a reconstruction plate and screws. Incomplete fractures of the iliac wing at the level of the iliac crest are not completed to reduce the anterior column fracture.
In high anterior column fractures not involving the quadrilateral plate, fracture reduction and compression osteosynthesis are performed as follows (Fig. 2). (1) The anterior column fracture is reduced by compressing the displaced anterior column using a colinear reduction forceps (Synthes, Zuchwil, Switzerland). (2) One or two lag screws (a 3.5 mm or 4.5 mm cortical screw or a 6.0 mm cancellous screw) are inserted in the supraacetabular area to obtain interfragmentary compression. (3) A 4.5 mm under-contoured narrow limited contact dynamic compression plate or a 4.5 mm reconstruction plate is placed on the pelvic brim and fixed with two 4.5 mm cortical screws through the two proximal holes of the plate placed on the intact ilium just lateral to the sacroiliac joint for additional compression and buttress of the anterior column fracture. The lag screws and the screws in the plate holes are tightened alternatively to obtain maximum interfragmentary compression without breaking the cortical bone. The plate is fixed additionally with one or two 4.5 mm cortical screws through the plate hole in the supra-acetabular area as in the lag screw technique. (4) An infra-acetabular screw is inserted additionally to increase the fixation strength whenever possible. In high anterior column fractures with a displaced quadrilateral plate fracture, fracture reduction and compression osteosynthesis are conducted as follows (Fig. 3). (1) The anterior column fracture is reduced by compressing the displaced anterior column with use of a colinear reduction forceps. One or two lag screws (a 3.5 mm or 4.5 mm cortical screw or a 6.0 mm cancellous screw) are inserted in the supra-acetabular area to obtain interfragmentary compression of the anterior column fracture. (2) The quadrilateral plate fracture is reduced with use of a colinear reduction forceps. (3) An over-contoured spring plate which was made preoperatively with a 3.5 mm 7- or 8-hole reconstruction plate is placed on the quadrilateral plate and the supra-acetabular area of the anterior column. The plate is pulled laterally with use of a pointed reduction forceps to compress the quadrilateral plate, and three or four 3.5 mm cortical screws are inserted eccentrically through the plate holes as in the lag screw technique for additional compression and buttress of the anterior column and the quadrilateral plate. (4) An infra-acetabular screw is inserted additionally to increase the fixation strength whenever possible.
Continuous passive motion or active motion of the hip is started after postoperative pain is sufficiently reduced with analgesics, usually postoperative day 3. Partial weight-bearing of a maximum of 20 kg is allowed at 3 weeks after surgery. Full weight-bearing is allowed at 6–8 weeks depending on fracture healing and muscle strength.
Nineteen patients with an isolated high anterior column fracture were included in this study. The mean age of patients was 47.8 years (range, 16 to 69 years), and 16 patients were male. The mean time from injury to surgery was 6.3 days (range, 3 to 12 days). The mean operation time (skin to skin) was 145 minutes (range, 100 to 220 minutes). The average follow-up was 42 months (range, 12 to 115 months). The mechanism of injury was as follows: 10 motor vehicle accidents, seven falls, one cycling accident, and one direct impact to the pelvis. Eleven patients had the associated injuries (Table 1).
Of the 19 fractures, 12 were incomplete high anterior column fractures where the fracture line did not reach to the iliac crest. Twelve fractures involved the quadrilateral plate, while the other seven did not. According to Matta's criteria, anatomical reduction was achieved in 17 patients and imperfect reduction in two patients (Table 2). According to Matta's criteria, clinical results were excellent in 17 patients and good in two patients, and radiographic results were excellent in 17 patients and good in two patients at the last follow-up (Table 3). The clinical results were excellent in all patients with anatomical reduction.
No patient in the series had loss of fracture reduction on any postoperative radiograph. Postoperative infection, heterotopic ossification, and posttraumatic osteoarthritis of the hip did not occur in any patient. There were no patients with an injury to the femoral vessel or nerve. However, 10 patients had neurapraxia of the lateral femoral cutaneous nerve related with the approach. Seven of them resolved completely without treatment, but three improved incompletely at the final follow-up. One patient had deep vein thrombosis. One patient had an injury to a small branch of the internal iliac artery during the procedure, which required pelvic packing and embolization of the artery.
Since Letournel10) introduced the ilioinguinal approach in the 1960s, it has been adopted by many surgeons as the principal anterior surgical approach for the treatment of acetabular fractures for several decades.351011) The classic ilioinguinal approach provides excellent access to the anterior and internal aspects of the entire pelvis and acetabulum. However, most of the complications are related to the neurovascular bundle and lymphatic structures and arise in the intermediate part of the ilioinguinal approach. Therefore, less invasive approaches have been developed to avoid surgical dissection of the second window of the approach.67891213)
In 1994, Cole and Bolhofner7) reported the use of the modified Stoppa limited intrapelvic approach for open reduction and internal fixation of acetabular fractures. This limited approach has well-known advantages of direct visualization, reduction, and plate fixation of medially displaced acetabular wall fractures as well as the avoidance of exposing the second window of the classic ilioinguinal approach. For these reasons, the modified Stoppa approach has gained popularity for use alone or in combination with a limited ilioinguinal approach using the lateral window.67891314) However, the modified Stoppa approach also carries the risk of bleeding from the corona mortise, injury to the obturator nerve and superior gluteal artery, and inguinal hernia.613141516)
In the current study, the high anterior column fracture was exposed only through the anterior iliac approach, which was almost the same as the lateral window of the classic ilioinguinal approach; therefore, major complications related to both of the ilioinguinal approach and the modified Stoppa approach could be avoided. However, injury to the lateral femoral cutaneous nerve could not be avoided because of applied tension to the nerve during the procedure. Injury to the lateral femoral cutaneous nerve has been reported in 12%–57% of patients treated with the ilioinguinal approach.1312) In our series, 10 patients had symptoms of neurapraxia of the lateral femoral cutaneous nerve, which resolved completely in all but three patients at the final follow-up. Care must be taken to avoid damage to the nerve by reducing tension of the nerve during the procedure.
Through a smaller incision, this anterior iliac approach offers sufficient exposure for fracture reduction and compression osteosynthesis of the high anterior column fracture. In cases of high anterior column fractures, the weight-bearing dome of the acetabulum must be reduced anatomically; however, the distal portion of the high anterior column fracture which is the superior pubic ramus fracture does not need anatomical reduction because this portion is not the weight-bearing dome. This concept led us to develop the less invasive surgery of compression osteosynthesis with limited fixation through the limited anterior iliac approach. In this study, the mean operation time of 145 minutes was relatively short though the composition of the patient cohort was different from other studies.912131718) The quality of reduction was satisfactory. Anatomical reduction was achieved in 17 patients and imperfect reduction in two patients, but there were no patients with poor reduction.
Anterior column fractures can be divided into several subtypes depending on the completeness of the iliac wing fracture and the presence of the quadrilateral plate fracture. Occasionally the anterior column fracture is incomplete at the level of the iliac crest. In such circumstances, there may be plastic deformation of the bone in the very thin central portion of the iliac wing. According to the literature, it is often impossible to achieve complete reduction without osteotomizing the iliac crest; therefore, the first step of reduction may be to complete the partial fracture in the iliac wing.19) However, we thought that accurate reduction of the fracture may be difficult to achieve after osteotomizing the iliac crest to make a complete fracture because of plastic deformation of the bone. In our series, all incomplete fractures in the iliac wing were reduced successfully without completing the partial fracture in the iliac wing. If the incomplete fracture of the iliac wing is not osteotomized, surgery may be rather simple and the operation time can be shortened because it does not need osteotomy and stabilization.
The anterior column fracture without the quadrilateral plate fracture was fixed with the under-contoured plate placed on the pelvic brim for interfragmentary compression and buttress of the fracture. The anterior column fracture with the quadrilateral plate fracture was fixed with the overcontoured spring plate for interfragmentary compression and buttress of both of the anterior column fracture and the quadrilateral plate fracture. Additionally, an infra-acetabular screw was fixed to improve fixation strength whenever possible.20) These fixation techniques provided sufficient stability to allow immediate mobilization of the patient and the hip joint after surgery; therefore, no patients had loss of reduction and the functional outcome was satisfactory.
Limitations of our study are the small number of patients and the retrospective study design involving consecutive patients. Considering the low incidence of anterior column fractures of the acetabulum, a multicenter study including a longer follow-up and a larger series of patients is necessary to determine the validity of our less invasive surgery. In addition, this study is not a randomized controlled trial but a retrospective analysis of consecutive patients. The low incidence of anterior column fractures is the major obstacle to randomized controlled trial design in this field. However, the quality of reduction and clinical results in our series are comparable to those of other studies. 51718)
Our less invasive surgical technique of the anterior iliac approach and compression osteosynthesis is a useful addition to the existing techniques in the treatment of high anterior column fractures of the acetabulum. Despite the limited approach and fixation, this technique provides sufficient exposure for reducing and fixing the fracture and adequate stability to allow immediate mobilization of the patient after surgery. With this technique, most complications related to the classic ilioinguinal approach can be avoided and the comparable quality of reduction and stable fixation can be achieved.
References
1. Letournel E, Judet R. Fractures of the acetabulum. 2nd ed. Berlin: Springer-Verlag;1993. p. 431–436.
2. Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996; 78(11):1632–1645. PMID: 8934477.
3. Mayo KA. Open reduction and internal fixation of fractures of the acetabulum: results in 163 fractures. Clin Orthop Relat Res. 1994; (305):31–37.

4. Heeg M, Otter N, Klasen HJ. Anterior column fractures of the acetabulum. J Bone Joint Surg Br. 1992; 74(4):554–557. PMID: 1624515.

5. Giannoudis PV, Kanakaris NK, Dimitriou R, Mallina R, Smith RM. The surgical treatment of anterior column and anterior wall acetabular fractures: short- to medium-term outcome. J Bone Joint Surg Br. 2011; 93(7):970–974. PMID: 21705573.
6. Hirvensalo E, Lindahl J, Bostman O. A new approach to the internal fixation of unstable pelvic fractures. Clin Orthop Relat Res. 1993; (297):28–32.

7. Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach: description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994; (305):112–123. PMID: 8050220.

8. Wolf H, Wieland T, Pajenda G, Vecsei V, Mousavi M. Minimally invasive ilioinguinal approach to the acetabulum. Injury. 2007; 38(10):1170–1176. PMID: 16979170.

9. Jakob M, Droeser R, Zobrist R, Messmer P, Regazzoni P. A less invasive anterior intrapelvic approach for the treatment of acetabular fractures and pelvic ring injuries. J Trauma. 2006; 60(6):1364–1370. PMID: 16766988.

10. Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993; (292):62–76.

11. Matta JM. Operative treatment of acetabular fractures through the ilioinguinal approach: a 10-year perspective. Clin Orthop Relat Res. 1994; (305):10–19.

12. Ruchholtz S, Buecking B, Delschen A, et al. The two-incision, minimally invasive approach in the treatment of acetabular fractures. J Orthop Trauma. 2013; 27(5):248–255. PMID: 22810546.

13. Sagi HC, Afsari A, Dziadosz D. The anterior intra-pelvic (modified rives-stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010; 24(5):263–270. PMID: 20418730.

14. Shazar N, Eshed I, Ackshota N, Hershkovich O, Khazanov A, Herman A. Comparison of acetabular fracture reduction quality by the ilioinguinal or the anterior intrapelvic (modified Rives-Stoppa) surgical approaches. J Orthop Trauma. 2014; 28(6):313–319. PMID: 24100918.

15. Bastian JD, Tannast M, Siebenrock KA, Keel MJ. Mid-term results in relation to age and analysis of predictive factors after fixation of acetabular fractures using the modified Stoppa approach. Injury. 2013; 44(12):1793–1798. PMID: 24008225.

16. Vikmanis A, Vikmanis A, Jakusonoka R, Jumtins A, Pavare Z. Mid-term outcome of patients with pelvic and acetabular fractures following internal fixation through a modified Stoppa approach. Acta Orthop Belg. 2013; 79(6):660–666. PMID: 24563971.
17. Mallina RK, Kanakaris NK, Tzioupis C, Giannoudis PV. Clinical outcomes following reconstruction of anterior column: anterior wall fractures of the acetabulum. Injury Extra. 2009; 40(10):218.
18. Mokawem M, Kanakaris NK, Mallina RK, Giannoudis PV. Medium to long term results of acetabular reconstruction following anterior column and anterior wall fractures. Injury Extra. 2011; 42(9):124–125.

19. Tile M, Helfet DL, Kellam JF. Fractures of the pelvis and acetabulum. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins;2003. p. 629–661.
20. Gras F, Marintschev I, Schwarz CE, Hofmann GO, Pohlemann T, Culemann U. Screw-versus plate-fixation strength of acetabular anterior column fractures: a biomechanical study. J Trauma Acute Care Surg. 2012; 72(6):1664–1670. PMID: 22695438.
Fig. 1
(A) Intraoperative photograph showing the anterior iliac approach. (B) Intraoperative photograph showing the adequate exposure of the anterior column fracture through the anterior iliac approach.
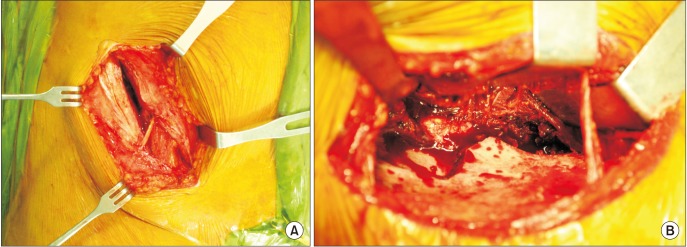
Fig. 2
(A) Standard anteroposterior radiograph of a fracture of the left acetabulum. Computed axial tomography (CAT) scans (B) and three-dimensional computed tomography (CT) scan (C) showing an anterior column fracture not involving the quadrilateral plate. (D) Postoperative anteroposterior radiograph of the anterior column fracture stabilized by compression osteosynthesis using a supra-acetabular lag screw and a narrow limited contact dynamic compression plate. Postoperative CAT scans (E) and sagittal reconstruction of CT scan (F) showing anatomical reduction of the fracture.
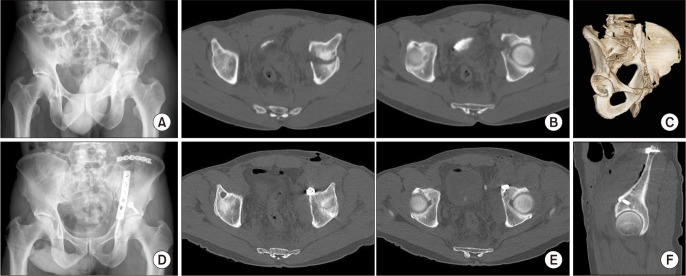
Fig. 3
(A) Standard anteroposterior radiograph of a fracture of the right acetabulum. Computed axial tomography (CAT) scans (B) and three-dimensional CT scan (C) showing an incomplete anterior column fracture with a displaced quadrilateral plate fracture. (D) Intraoperative photograph showing anatomical reduction of the fracture and fixation with a lag screw and a spring plate. (E) Postoperative anteroposterior radiograph of the anterior column fracture stabilized by compression osteosynthesis using a supra-acetabular lag screw and a spring plate. Postoperative CAT scans (F) and sagittal reconstruction of CT scan (G) showing anatomical reduction of the fracture.
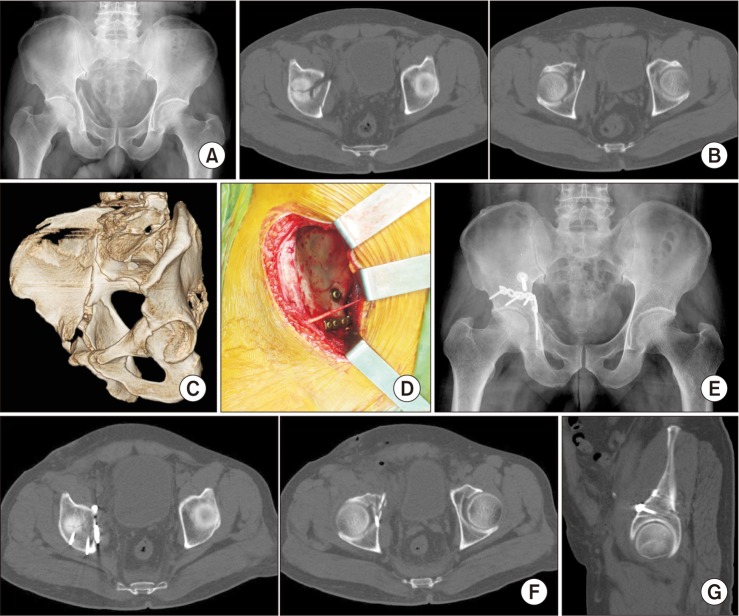
Table 1
Associated Injuries (Including Overlapping Injury)
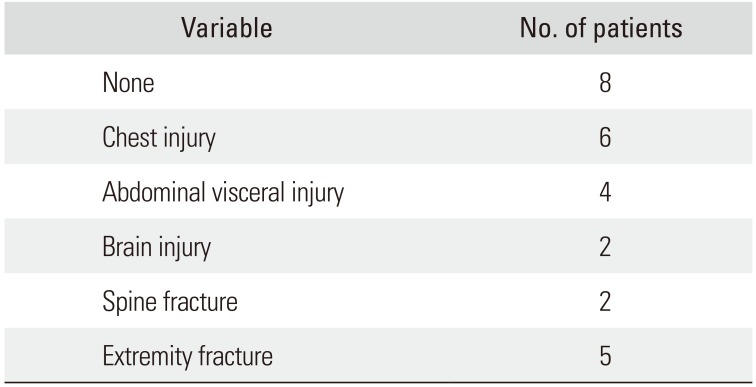
| Variable | No. of patients |
|---|---|
| None | 8 |
| Chest injury | 6 |
| Abdominal visceral injury | 4 |
| Brain injury | 2 |
| Spine fracture | 2 |
| Extremity fracture | 5 |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download