Abstract
Atypical fractures have been reported as a complication of long-standing bisphosphonate therapy and occur commonly in the subtrochanteric region or shaft of the femur showing typical radiographic features. We encountered a case of atypical fracture of the proximal one-third of the shaft of the ulna. Radiographic findings of this case differed from previously reported cases of ulnar fracture in terms of showing a transverse fracture line with cortical thickening and an oblique fracture line with anterior cortical spike. On the other hand, these findings were similar to radiographic features of atypical femoral fractures. The present case was managed surgically and union of fracture was achieved after 6 months. As there are possibilities of occurrence of atypical fractures in sites other than the femur, the physicians should cautiously examine the patients' history and radiographic findings.
With an increase in the aging population worldwide, there is a growing interest in age-related diseases such as osteoporosis. As osteoporosis can lead to fragility fractures of the spine, hip, pelvis, proximal humerus, or distal radius, the condition requires appropriate management for prevention of these fractures. Bisphosphonates are one of the most widely prescribed classes of medications for the management of osteoporosis. Previous studies have reported that bisphosphonates prevent future osteoporotic fractures in patients with a history of osteoporosis-related fractures or postmenopausal osteoporosis.12)
Atypical fractures have been reported as a complication in patients with prolonged bisphosphonate administration and occur commonly as subtrochanteric or diaphyseal fractures of the femur showing characteristic findings on plain radiographs.34) Occurrence of atypical fractures is very rare in sites other than the femur even though incidences in the pelvis, tibia, clavicle, and forearm have been reported.56789) There exists seldom awareness about atypical fractures in the forearm as compared to the femur. To date, only eight cases in seven patients have been published in English literature.9) Seven of the eight fractures were accompanied by shaft fractures of the ulna and one was associated with the shaft fracture of the radius. These fractures should be treated surgically because of a risk of nonunion and discontinuation of bisphosphonate administration is required for fracture healing. Therefore, the physicians should be aware of typical findings of these fractures for accurate diagnosis and treatment. We present a case of atypical shaft fracture of the ulna in a patient receiving long-term bisphosphonate therapy.
A 72-year-old woman experienced a light fall while taking a walk around her house on March 28, 2015. She visited the outpatient department of Konyang University Hospital after 3 days of injury with a complaint of mild pain in her left forearm although she was able to move the forearm. The patient weighed 66 kg and height was 159 cm. She had no prodromal symptom in the left forearm and had no restrictions in daily activities and walking. Furthermore, comorbidities such as hypertension, diabetes mellitus, thyroid disease, or gynecologic cancer, were absent. She was neither a smoker nor a drinker of alcohol. She had a past history of fracture of the left distal radius and ulnar styloid and was treated with closed reduction and percutaneous pinning in 2008. Since 2008, after the fracture of the left wrist, she had been continuously taking oral alendronate (a dosage of alendronic acid 70 mg/wk) of bisphosphonates for osteoporosis.
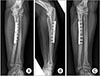
There were no signs of skin abrasion, ecchymosis, and swelling in the left forearm, but tenderness on the proximal border of the ulna was noted. She complained of discomfort during rotation of the injured forearm although range of motion of the left elbow and wrist was not limited. We confirmed a complete shaft fracture without comminution and minimal displacement in the proximal one-third of the ulna on radiographs of the left forearm (Fig. 1A and B). This fracture showed a combined configuration of a transverse fracture line and an oblique fracture line. Radiographs of the contralateral forearm and both femurs did not show any findings of fracture. Also, the whole body bone scan showed no hot uptake except for hot-uptake in the left proximal forearm consistent with fracture (Fig. 1C). Bone mineral density measured by dual-energy X-ray absorptiometry was 0.776 mg/cm2 (T score, −2.4), 0.858 g/cm2 (T score, −0.3) and 0.912 g/cm2 (T score, 0.1) at the lumbar spine, right hip, and left hip, respectively. The results of laboratory tests at the time of presentation were as follows: serum creatinine, 0.57 mg/dL (normal, 0.51 to 1.17 mg/dL); blood urea nitrogen, 9.8 mg/dL (normal, 8 to 20 mg/dL); alkaline phosphatase, 60 IU/L (normal, 40 to 120 IU/L); osteocalcin, 18.34 ng/mL (postmenopausal, 13 to 48 ng/mL); C-telopeptide, 0.593 ng/mL (postmenopausal, < 1.00 ng/mL); procollagen III peptide, 0.81 U/mL (normal, 0.3 to 0.8 U/mL); and urine N-telopeptide, 50.68 nM BCE/mM (normal, 5.0 to 65.0 nM BCE/mM).
The fracture was fixed using a 3.5-mm dynamic compression plate without bone graft (Fig. 2). We applied a cast immobilization to the patient for 4 weeks postoperatively and allowed light daily activities later. Union of the fracture was achieved at 6 months after surgery (Fig. 3). Bisphosphonate therapy was stopped immediately after surgery and restarted after the union of fracture.
Atypical fractures are different from osteoporotic fragility fractures in many respects.3) Common sites of atypical fractures are the subtrochanteric or shaft region of the femur, whereas osteoporotic fractures occur mainly in the spine and the neck or intertrochanteric region of the femur. Atypical femoral fractures are commonly associated with prodromal pain and demonstrate several typical features on radiographs. Certain major and minor features for diagnosing atypical femoral fractures were described by Shane et al.4)
Prevalent factors associated with atypical femoral fractures include Asian descent, bilateral fractures, prodromal pain, concomitant glucocorticoids/proton pump inhibitors, and delayed fracture healing.3) Because an increased curvature of the femoral diaphysis could be altered by stress on the lateral cortex of the femur, the geometry of the lower limb may be considered as a predisposing factor for development of atypical femoral fractures.10)
Several studies have shown a significantly increased risk of atypical femoral fractures in patients taking bisphosphonates for over 5 or more years.3) Recently, atypical femoral fractures have been commonly observed in patients taking bisphosphonates for over 3 years.4) Although the relative risk of occurrence of atypical femoral fractures are high in patients taking bisphosphonates (2.1 to 128 cases per 100,000 persons per year), the absolute risk is low (3.2 to 50 cases per 100,000 persons per year). However, a long-term bisphosphonates use may be associated with a higher risk of developing atypical femoral fractures (>100 cases per 100,000 persons per year).4)
Atypical forearm fractures are rarer than atypical femoral fractures and have been reported in only seven publications previously. Tan et al.9) systematically reviewed seven publications (eight fractures in seven patients) and reported findings of atypical forearm fractures. Demographic and clinical characteristics of the seven patients with atypical forearm fractures were as follows: (1) all patients were female; (2) age range, from 76 to 85 years; (3) prodromal pain (range, from 6 weeks to 6 months) in three out of seven patients; (4) bilateral ulnar fracture in one patient; (5) premorbid ambulatory status in three out of seven patients; (6) comorbidities in three out of seven patients; and (7) all patients had a history of osteoporosis and four of them had a previous history of osteoporotic fractures.9) Furthermore, the duration of bisphosphonate use prior to atypical ulnar fracture ranged from 7 to 15 years. Demographic findings of the current case (female, 72 years of age, no prodromal pain, unilateral fracture, no comorbidity, and bisphosphonate use for 7 years) were similar to those described above.
Radiographic features of atypical forearm fractures include a common location in the proximal one-third of the ulnar shaft, transverse fracture configuration, no comminution, no spike, surrounding bony sclerosis and cortical thickening.9) On the other hand, the case presented in this report showed a combined configuration of a transverse fracture line with cortical thickening and an oblique fracture line with anterior cortical spike. We assumed that a transverse incomplete fracture line might have initially originated from the tension side (posterior border) of the proximal ulna and an oblique complete fracture line might have subsequently occurred following minor trauma. Because previous cases of atypical ulnar fracture had no trauma, we think that transverse fracture without a spike might have occurred.
Five of the previously reported eight fractures were treated surgically and other three were managed conservatively. 9) Union of fracture was achieved in four fractures fixed with plating. Nonunion was found in two fractures, one of which was managed surgically and the other conservatively. Treatment results of two fractures (bilateral fracture in one patient) were not reported in the original study. Our case achieved union by internal fixation without bone graft. We believe that conservative treatment can increase the risk of nonunion although the number of reported cases is very small.
Prolonged bisphosphonate use is commonly identified as an important risk factor for atypical fractures. Although the common site of atypical fractures is the subtrochanteric region or shaft of the femur, we experienced an atypical fracture of the proximal ulna showing different radiographic findings compared with previous reports. It is proposed that the physicians need to be careful not to miss atypical fractures in sites other than the femur.
Figures and Tables
Fig. 1
(A) Preoperative anteroposterior radiograph of the left forearm showing a transverse fracture line with cortical thickening on the proximal ulna. (B) Preoperative lateral radiograph of the left forearm showing an oblique fracture line with anterior cortical spike on the proximal ulna. (C) Whole body bone scan showed no uptake in the right forearm and both femurs.

References
1. Black DM, Schwartz AV, Ensrud KE, et al. Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA. 2006; 296(24):2927–2938.

2. Cranney A, Wells G, Willan A, et al. Meta-analyses of therapies for postmenopausal osteoporosis. II. Meta-analysis of alendronate for the treatment of postmenopausal women. Endocr Rev. 2002; 23(4):508–516.

3. Unnanuntana A, Saleh A, Mensah KA, Kleimeyer JP, Lane JM. Atypical femoral fractures: what do we know about them? AAOS Exhibit Selection. J Bone Joint Surg Am. 2013; 95(2):e8.1–e8.13.
4. Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014; 29(1):1–23.

5. Imai K, Yamamoto S, Anamizu Y, Horiuchi T. Pelvic insufficiency fracture associated with severe suppression of bone turnover by alendronate therapy. J Bone Miner Metab. 2007; 25(5):333–336.

6. Tantavisut S, Tanavalee A, Thanakit V, Ngarmukos S, Wilairatana V, Wangroongsub Y. Spontaneous acetabular periprosthetic fracture in a patient continuously having zoledronic acid. Clin Orthop Surg. 2014; 6(3):358–360.

7. Breglia MD, Carter JD. Atypical insufficiency fracture of the tibia associated with long-term bisphosphonate therapy. J Clin Rheumatol. 2010; 16(2):76–78.

8. Vun SH, Husami Y, Shareef S, Bramley D. Acute nontraumatic clavicle fracture associated with long-term bisphosphonate therapy. Case Rep Orthop. 2014; 2014:986718.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download