Abstract
PURPOSE
Plasma activation of hydrophobic zirconia surfaces might be suitable to improve the bond strength of luting materials. The aim of this study was to analyze the influence of nonthermal argon-plasma on the shear bond strength (SBS) between zirconia and different combinations of 10-MDP adhesive systems and luting composites after artificial aging.
MATERIALS AND METHODS
Two hundred forty Y-TZP specimens were ground automatically with 165 µm grit and water cooling. Half of the specimens received surface activation with nonthermal argon-plasma. The specimens were evenly distributed into three groups according to the adhesive systems ([Futurabond U, Futurabond M, Futurabond M + DCA], VOCO GmbH, Germany, Cuxhaven) and into further two subgroups according to the luting materials ([Bifix SE, Bifix QM], VOCO GmbH). Each specimen underwent artificial aging by thermocycling and water storage. SBS was measured in a universal testing machine. Statistical analysis was performed using ANOVA and Scheffè procedure with the level of significance set to 0.05.
RESULTS
Surface activation with nonthermal plasma did not improve the bond strength between zirconia and the tested combinations of adhesive systems and luting materials. The plasma-activation trended to reveal higher bond strength if the self-etch luting material (Bifix SE) was used, irrespective of the adhesive system.
All-ceramic crowns or bridges are a well described alternative for metal-ceramic restorations to provide patients highly esthetic restorations. CAD/CAM technology enlarged the range of materials for these restorations, such as zirconia, silicate ceramics, or hybrid ceramics. Long term stability of dental restorations is influenced by aging during their lifetime in the patient's mouth. Nowadays a variety of aging effects on the long term stability of FPDs is well known. Besides biological factors such as the natural mobility of the abutment teeth and saliva immersion, technical factors such as the properties of the ceramic components and the design-parameters of the framework can influence the long-term stability of all-ceramic FPDs.123
To prevent chipping fractures, monolithic all-ceramic restorations have been developed in the recent past, although fractures of the entire restoration or adhesive failures can still appear.4 Further improvement of the bond strength between ceramic material, especially zirconia, and adhesive system is the focus of the current research. Different studies have been published in the recent years, which have focused on modification of the zirconia surface by mechanical techniques or primer systems. Besides various coating techniques using silica, alumina and aluminium nitride are also described.5678
Literature proves that modern 10 MDP-containing adhesive systems can bond to many types of zirconia.910 The phosphoric acid groups of 10-methacryloyloxydecyl dihydrogen phosphate (10-MDP) can react with the oxide layer on the surface of the ceramic material. This leads to adequate adhesion between zirconia and composite.7 Further, the use of 10-MDP seems to be suitable to reduce hydrolytic decrease of bond strength.8 Despite these advantages, the decrease of the bond strength between adhesive luting systems and zirconia restorations during the clinical use still remains a problem, which may be caused by the hydrophobic surface of zirconia.
Literature discusses the influence of plasma on the bond strength between zirconia and different materials. Plasma activation of the ceramic surface previous to the application of the adhesive system might be a suitable method to reduce the risk for hydrolytic failures of zirconia-composite adhesion. In general, plasma can be generated by heating a neutral gas until it becomes an ionized substance that is electrically conductive. The behaviour and properties of plasma depend on the type of gas, e.g. argon or oxygen, the temperature and on the environmental conditions. Canullo et al.11 found significantly higher bond strength between zirconia and resin cement after argon plasma activation of the zirconia surface. Noro et al.12 compared the shear bond strength (SBS) of zirconia-resin adhesion after plasma activation, UV activation, and the use of ceramic primer. They didn't find any increase of bond strength after the use of plasma. Wu et al.13 showed that the duration of plasma treatment has an influence on the effect on the zirconia surface. They also showed the increase in hydrophilicity of the zirconia surface. Tabari et al.14 showed that micro-SBS between zirconia and composite increased after treatment with a combination of 20% argon and 80 % oxygen plasma. Plasma activation resulted in a significantly smaller contact angle of the adhesive on the ceramic surface, which explains the increase in surface hydrophilicity. dos Santos et al.,15 in their study on the influence of aging of nonthermal plasma activated zirconia surfaces, showed that an initially high level of hydrophilicity did not persist after the aging process.
In general, there is lack of literature concerning the effect of plasma on the bond strength between zirconia and resin materials. The existing literature is contradictory on the effect of plasma on the bond strength between zirconia and resin. The aim of the current in vitro study was to analyze the influence of nonthermal argon-plasma on the SBS between zirconia and two types of luting composites after surface pretreatment with three different 10-MDP adhesive systems. The first hypothesis was that treatment with nonthermal argon-plasma improves the SBS of zirconia-composite interfaces significantly. The second hypothesis was that treatment with nonthermal argon-plasma improves the hydrostability of zirconia-composite interfaces significantly.
In total, 240 specimens were produced with a specimen design, which was developed at Hannover Medical School for shear bond tests in the recent years.78 Previous studies proved that a sample size of n = 10 in each group is enough for effective statistical analysis.78
240 plates measuring 8 mm × 8 mm × 3 mm were cut out of a Y-TZP zirconia block (InCoris Maxi-S, Sirona, Bensheim, Germany) and sintered at 1510℃ for 120 minutes following the manufacturer's instructions. All of the plates were embedded in round moulds (Ringform 30 mm, Buehler GmbH, Düsseldorf, Germany) using epoxy resin (EpoThin Epoxy Resin, Buehler GmbH, Düsseldorf, Germany). The samples were ground in an automatic polishing machine (PowerPro 4000, Buehler GmbH, Düsseldorf, Germany) with 165 µm grit SC paper and water cooling. 165 µm grit SC paper was used to simulate zirconia surface after CAD/CAM manufacturing and luminal adjustments with diamond burs. This surface preparation protocol was used at Hannover Medical School for recent years. After the preparation of the zirconia specimens a surface roughness of Ra = 0.31 µm (SD 0.03 µm) could be found. To ensure even ablation during the grinding process, zirconia balls were embedded together with the ceramic plates.
The specimens were cleaned with alcohol and dried using oil-free compressed air. Half of the specimens (n = 120) received surface activation using nonthermal argon-plasma applied with a handpiece for intraoral use (Plasmabeam mini, Diener electronig GmbH, Ebhausen, Germany). According to technical information, the Plasmabeam system works under atmospheric conditions with a frequency of 2.45 GHz and a demand of 10 W. The gas load of 2 – 3 L/min and pressure of the process gas is controlled by the device using automatic process control. The zirconia surface was activated for 30 seconds with a distance between zirconia and the working tip of the plasma handpiece of 10 mm ± 1.0 mm (Fig. 1).
These ground (G) and the plasma activated (PA) specimens were evenly distributed into three groups (each n = 40) for different adhesive surface treatments ([FBU = Futurabond U, FBM = Futurabond M+, FBMD = Futurabond M+ + DC-Activator], VOCO GmbH, Germany, Cuxhaven). The adhesive systems were applied following the manufacturer's instructions. An acrylic glass tube with an internal diameter of 3 mm (Hohlsticks, BEGO, Bremen, Germany) was positioned in the middle of the zirconia surface with a small portion of sticky wax (Supradent Klebewachs, M+W Dental GmbH, Bündingen, Germany) on the outer side of the tube, but sparing the tube-lumen. Each of these groups were subdivided into two subgroups (n = 20) according to the luting material ([SE = BifixSE, QM = BifixQM], VOCO GmbH, Germany, Cuxhaven).
The luting composites were applied into the acrylic tube using the manufacturer's application system; in accordance with the clinical procedure during adhesive luting of FPDs, the adhesive system and the luting composite were light cured simultaneously. Polymerization was performed using a polywave-LED polymerization lamp (Bluephase, Ivoclar Vivadent, Ellwangen, Germany) for 40 s at 1200 mW/cm2.
The sticky wax was carefully removed using a scalpel. The SBS of each half of the specimens in each group (n = 10) was tested 24 hours after polymerization. The remaining half of the specimens underwent artificial aging by thermocycling between 5℃ and 55℃ for 5000 cycles and by storage in water at 36℃ for 100 days. SBS values of these specimens were measured 24 hours after artificial aging. Fig. 2 gives an overview about the experimental groups.
The shear bond tests were performed with a universal testing machine (UTS 20K, UTS Testsysteme GmbH & Co KG, Ulm, Germany). Load transfer to the acrylic tube with the composite material was accomplished parallel to the ceramic composite interface with a steel blade with 0.5 mm radius of curvature at its loading edge. The jig to fix the samples was custom-made at Hannover Medical School.78 Shear bond tests were performed with a cross-head speed of 1 mm/min, and the load until fracture was measured (Phoenix - Version V 5.04.006, UTS - Testsysteme GmbH & Co KG, Ulm, Germany). Fracture was defined by a decrease in load of 5 N. Force at fracture was divided by the ceramic-composite interface area for conversion into apparent shear bond strength.
Statistical analysis was performed by Kolmogorow Smirnov Test, Levene Analysis, ANOVA and Scheffè Procedure with the level of significance set to 0.05 (IBM SPSS Statistics V24, 2016, IBM Corp., New York, NY, USA).
The Kolmogorov-Smirnov test showed a normal distribution of the data (P < .001). Levene-Analysis proved homogeneity of variances (P < .001). ANOVA showed significant differences among all groups (P < .001). Scheffé procedure was used for single comparisons.
To get information about the effect of plasma activation on the shear bond strength, each experimental plasma-activated group was compared to its corresponding control group with the grit surface.
Within the non-aged subgroups (P ≥ .992) (Fig. 3) and within the artificially aged subgroups (P ≥ .999) (Fig. 4), significant differences could not be found in these pairwise comparisons. Pairwise comparisons between the corresponding groups with self-etch luting cement BifixSE after the aging process showed a trend for increased bond strength after the use of nonthermal plasma (Fig. 4, accentuated dotted boxes). However, these differences were not statistically significant.
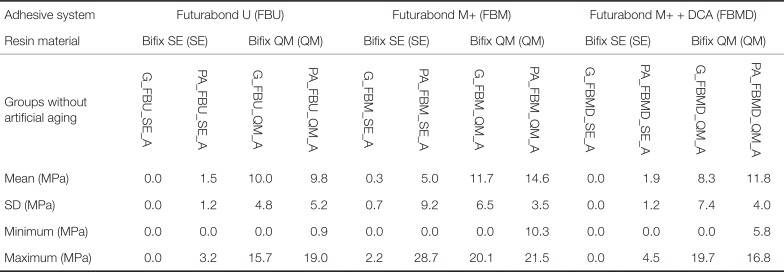
Furthermore, the data was analysed with special interest on the influence of artificial aging on the shear bond strength. SBS decreased significantly after artificial aging (P < .001) in all groups where Bifix SE has been used (e.g. G_FBU_SE vs. G_FBU_SE_A; PA_FBU_SE vs. PA_FBU_SE_A). Comparison of the correlating Bifix QM groups also showed a decrease in mean bond strength after the aging process, but these differences were statistically not significant (0.101 ≤ P ≤ 0.999) (Fig. 3, Fig. 4).
During the shear bond tests, all specimens showed adhesive failures at the zirconia-composite interface. Cohesive failures within the composite did not occur. In groups G_FBU_SE_A and G_FBMD_SE_A, all samples failed previous to the shear bond test during the aging process.
Literatures show that mechanical surface treatment can increase bond strength between zirconia and different types of luting agents. Therefore, roughening of the zirconia surface using rotating instruments or air abrasion by sandblasting are well described and established, but mechanical surface treatment might cause microdamage of the zirconia structures.1617 Different reasons for the failure of all-ceramic FPDs are discussed in literature, including loss of primary stability of the zirconia caused by phase transformation, micro leakage caused by polymerization shrinkage, or differential thermal expansion of the materials.18192021 Hydrolytic processes might cause decreasing SBS.222324
Surface pretreatment with nonthermal plasma activation seems to be a promising possibility for further improvement of bond strength between zirconia and composite in addition or alternatively to mechanical surface treatment.1112131425 Park et al.26 showed that SBS between resin cement and precolored zirconia was improved after the use of nonthermal atmospheric pressure plasma. Liu et al.27 identified nonthermal plasma as a cost effective method for surface modification to improve bond strength for clinical and dental laboratory use. Henningsen et al.28 showed that treatment of zirconia with nonthermal plasma improves the wettability and the physicochemical surface conditions of zirconia and titanium.
In the current study, the influence of nonthermal plasma activation on the SBS between luting resin and zirconia was analyzed. Therefore, a flat zirconia specimen design was chosen to ensure a reproducible method, and the specimens were ground with diamond containing SC-abrasive paper under water cooling to simulate surface roughness after CAD/CAM milling processes with diamond burs. Nonthermal argon plasma was applied on the zirconia surface in the experimental groups with a handpiece with a distance of 10 mm ± 1.0 mm for 30 seconds. This is according to clinical practice, because intraorally it is not possible to ensure a constant distance between cramic surface of FPDs and the working tip of the plasma handpiece because of the uneven outershape of the FPDs. Further, the distance between ceramic surface and plasma handpiece would be limited by surrounding tissues such as the planum buccale or the tongue, especially in the posterior area. In literature, there is no consensus about the ideal working distance or the ideal application time of the plasma beam.
The current study showed that pretreatment of the zirconia surface with nonthermal argon plasma did not increase the SBS to the tested luting composites, irrespective of the type of 10-MDP adhesive system. Therefore, the first hypothesis, that treatment with nonthermal argon-plasma improves the SBS of zirconia-composite interfaces significantly, had to be rejected. 10-MDP adhesives have been chosen because of the findings of other studies, which proved that 10-MPD primers improve the bond strength between zirconia and composite after mechanical pretreatment.2930 The use of the universal luting material BifixQM revealed significantly higher bond strength after artificial aging than the self-etch luting material BifixSE, which is in line with the findings of previous studies.78 Between the correlating groups, the use of nonthermal plasma did not resolve the decrease of SBS after artificial aging significantly. Therefore the second hypothesis, that treatment with nonthermal argon-plasma improves the hydrostability of zirconia-composite interfaces significantly, also had to be rejected.
The number of articles in the current literature on the bond between zirconia and resin after nonthermal plasma treatment is very small. Searching for relevant literature in ‘pubmed.gov’ database using search terms “zirconia”, “resin”, and “plasma” revealed 24 articles in total. Only 9 of these articles were comparable in their content. Because these studies have used highly different research methods, comparison of the current study with literature is very difficult. Most of these nine studies found increased bond strength between zirconia and resin material after the use of plasma,11131425262731 while only two studies could not find any effect on the bond strength.1232 In the current study, no significant improvement of the SBS of zirconia-composite interfaces could be found. However, a trend of increasing SBS could be seen when Bifix SE was used, especially in combination with Futurabond M+ and Futurabond M + DCA.
Based on the findings of the current study and on the results of existing literature, it can be concluded that the use of nonthermal plasma might have a positive effect on the SBS between zirconia and resin materials, but further research is necessary to identify effects of influencing factors, such as varying parameters of the plasma beam or different chemical compositions of the resin materials or adhesive systems.
Within the limitations of the current study, the following conclusions can be drawn: the surface pretreatment with nonthermal argon plasma did not improve SBS between zirconia and resin in comparison to surface grinding. Artificial aging decreased SBS in the groups without plasma activation and in the groups with plasma activation. In combination with self-etch resin materials, the bond strength trended to decrease less after the use of nonthermal plasma, but without showing significant differences.
References
1. Rosentritt M, Behr M, Scharnagl P, Handel G, Kolbeck C. Influence of resilient support of abutment teeth on fracture resistance of all-ceramic fixed partial dentures: an in vitro study. Int J Prosthodont. 2011; 24:465–468. PMID: 21909489.
2. Aladağ A, Elter B, Çömlekoğlu E, Kanat B, Sonugelen M, Kesercioğlu A, Özcan M. Effect of different cleaning regimens on the adhesion of resin to saliva-contaminated ceramics. J Prosthodont. 2015; 24:136–145. PMID: 24919532.

3. Kohorst P, Herzog TJ, Borchers L, Stiesch-Scholz M. Load-bearing capacity of all-ceramic posterior four-unit fixed partial dentures with different zirconia frameworks. Eur J Oral Sci. 2007; 115:161–166. PMID: 17451508.

4. Zhang Y, Lee JJ, Srikanth R, Lawn BR. Edge chipping and flexural resistance of monolithic ceramics. Dent Mater. 2013; 29:1201–1208. PMID: 24139756.

5. Chen L, Suh BI, Kim J, Tay FR. Evaluation of silica-coating techniques for zirconia bonding. Am J Dent. 2011; 24:79–84. PMID: 21698986.
6. Külünk T, Külünk S, Baba S, Oztürk O, Danişman S, Savaş S. The effect of alumina and aluminium nitride coating by reactive magnetron sputtering on the resin bond strength to zirconia core. J Adv Prosthodont. 2013; 5:382–387. PMID: 24353874.

7. Pott PC, Stiesch M, Eisenburger M. Influence of 10-MDP adhesive system on shear bond strength of zirconia-composite interfaces. J Dent Mater Tech. 2015; 4:117–126.
8. Pott PC, Stiesch M, Eisenburger M. Influence of artificial aging on the shear bond strength of zirconiacomposite interfaces after pretreatment with new 10-MDP adhesive systems. J Dent Mater Tech. 2016; 5:1–9.
9. Koizumi H, Nakayama D, Komine F, Blatz MB, Matsumura H. Bonding of resin-based luting cements to zirconia with and without the use of ceramic priming agents. J Adhes Dent. 2012; 14:385–392. PMID: 22282752.
10. Saker S, Ibrahim F, Ozcan M. Effect of different surface treatments on adhesion of In-Ceram Zirconia to enamel and dentin substrates. J Adhes Dent. 2013; 15:369–376. PMID: 23534029.
11. Canullo L, Micarelli C, Bettazzoni L, Koçi B, Baldissara P. Zirconia-composite bonding after plasma of argon treatment. Int J Prosthodont. 2014; 27:267–269. PMID: 24905269.

12. Noro A, Kameyama A, Haruyama A, Takahashi T. Influence of hydrophilic pre-treatment on resin bonding to zirconia ceramics. Bull Tokyo Dent Coll. 2015; 56:33–39. PMID: 25765573.

13. Wu CC, Wei CK, Ho CC, Ding SJ. Enhanced hydrophilicity and biocompatibility of dental zirconia ceramics by oxygen plasma treatment. Materials (Basel). 2015; 8:684–699. PMID: 28787965.
14. Tabari K, Hosseinpour S, Mohammad-Rahimi H. The impact of plasma treatment of Cercon zirconia ceramics on adhesion to resin composite cements and surface properties. J Laser Med Sci. 2017; 8:S56–S61.

15. dos Santos DM, Vechiato-Filho AJ, da Silva EV, Goiato MC, Cesar PF, Rangel EC, da Cruz NC. Aging effect of atmospheric air on zirconia surfaces treated by nonthermal plasma. J Adhes Dent. 2015; 17:413–419. PMID: 26525005.
16. Casucci A, Mazzitelli C, Monticelli F, Toledano M, Osorio R, Osorio E, Papacchini F, Ferrari M. Morphological analysis of three zirconium oxide ceramics: Effect of surface treatments. Dent Mater. 2010; 26:751–760. PMID: 20471073.

17. Denry IL, Holloway JA. Microstructural and crystallographic surface changes after grinding zirconia-based dental ceramics. J Biomed Mater Res B Appl Biomater. 2006; 76:440–448. PMID: 16184529.

18. Kawai Y, Uo M, Wang Y, Kono S, Ohnuki S, Watari F. Phase transformation of zirconia ceramics by hydrothermal degradation. Dent Mater J. 2011; 30:286–292. PMID: 21597215.

19. Nakamura T, Usami H, Ohnishi H, Takeuchi M, Nishida H, Sekino T, Yatani H. The effect of adding silica to zirconia to counteract zirconia's tendency to degrade at low temperatures. Dent Mater J. 2011; 30:330–335. PMID: 21597219.

20. de Gee AF, Feilzer AJ, Davidson CL. True linear polymerization shrinkage of unfilled resins and composites determined with a linometer. Dent Mater. 1993; 9:11–14. PMID: 8299861.

21. Göstemeyer G, Jendras M, Dittmer MP, Bach FW, Stiesch M, Kohorst P. Influence of cooling rate on zirconia/veneer interfacial adhesion. Acta Biomater. 2010; 6:4532–4538. PMID: 20601242.

22. Ernst CP, Aksoy E, Stender E, Willershausen B. Influence of different luting concepts on long term retentive strength of zirconia crowns. Am J Dent. 2009; 22:122–128. PMID: 19626977.
23. Lindgren J, Smeds J, Sjögren G. Effect of surface treatments and aging in water on bond strength to zirconia. Oper Dent. 2008; 33:675–681. PMID: 19051861.

24. Ozcan M, Nijhuis H, Valandro LF. Effect of various surface conditioning methods on the adhesion of dual-cure resin cement with MDP functional monomer to zirconia after thermal aging. Dent Mater J. 2008; 27:99–104. PMID: 18309618.
25. Valverde GB, Coelho PG, Janal MN, Lorenzoni FC, Carvalho RM, Thompson VP, Weltemann KD, Silva NR. Surface characterisation and bonding of Y-TZP following non-thermal plasma treatment. J Dent. 2013; 41:51–59. PMID: 23044388.

26. Park C, Yoo SH, Park SW, Yun KD, Ji MK, Shin JH, Lim HP. The effect of plasma on shear bond strength between resin cement and colored zirconia. J Adv Prosthodont. 2017; 9:118–123. PMID: 28435621.

27. Liu T, Hong L, Hottel T, Dong X, Yu Q, Chen M. Non-thermal plasma enhanced bonding of resin cement to zirconia ceramic. Clin Plasma Med. 2016; 4:50–55. PMID: 28239541.

28. Henningsen A, Smeets R, Heuberger R, Jung OT, Hanken H, Heiland M, Cacaci C, Precht C. Changes in surface characteristics of titanium and zirconia after surface treatment with ultraviolet light or non-thermal plasma. Eur J Oral Sci. 2018; 126:126–134. PMID: 29336070.

29. Kitayama S, Nikaido T, Takahashi R, Zhu L, Ikeda M, Foxton RM, Sadr A, Tagami J. Effect of primer treatment on bonding of resin cements to zirconia ceramic. Dent Mater. 2010; 26:426–432. PMID: 20102781.

30. Foxton RM, Cavalcanti AN, Nakajima M, Pilecki P, Sherriff M, Melo L, Watson TF. Durability of resin cement bond to aluminium oxide and zirconia ceramics after air abrasion and laser treatment. J Prosthodont. 2011; 20:84–92. PMID: 21284762.

31. Ito Y, Okawa T, Fukumoto T, Tsurumi A, Tatsuta M, Fujii T, Tanaka J, Tanaka M. Influence of atmospheric pressure low-temperature plasma treatment on the shear bond strength between zirconia and resin cement. J Prosthodont Res. 2016; 60:289–293. PMID: 26948430.

32. Hallmann L, Ulmer P, Lehmann F, Wille S, Polonskyi O, Johannes M, Köbel S, Trottenberg T, Bornholdt S, Haase F, Kersten H, Kern M. Effect of surface modifications on the bond strength of zirconia ceramic with resin cement resin. Dent Mater. 2016; 32:631–639. PMID: 26898723.

Fig. 1
Plasma activation of the surface of an embedded zirconia specimen previous to adhesive treatment.

Fig. 3
Boxplot showing SBS with the corresponding groups without artificial aging next to each other.
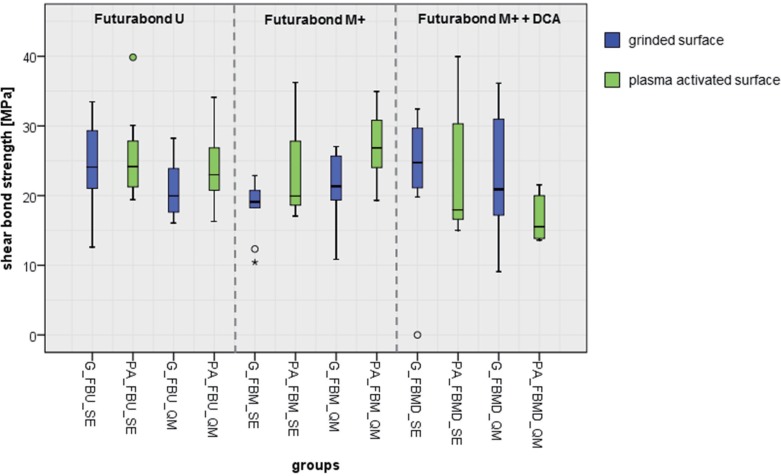
Fig. 4
Boxplot showing SBS with the corresponding groups after artificial aging next to each other.
Corresponding groups with BifixSE are accentuated with dotted boxes.
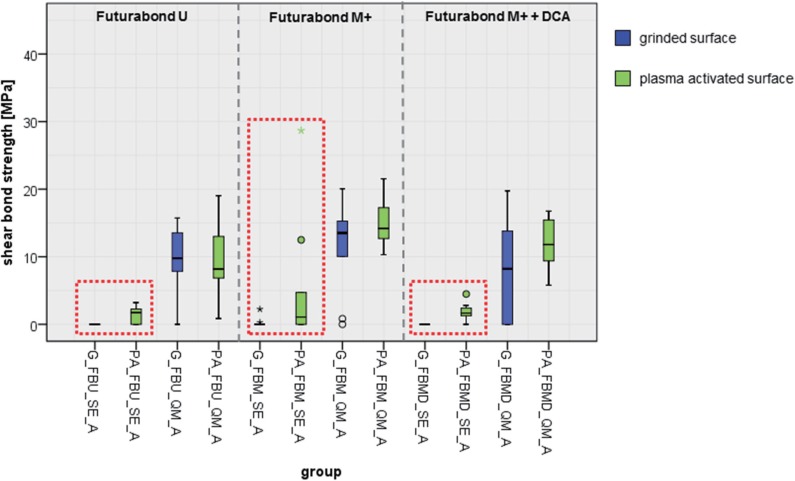
Table 1
Shear bond strength (SBS) of specimens with surface pretreatment by grinding (G) or plasma activation (PA), in combination with different adhesive systems and resin materials without artificial aging
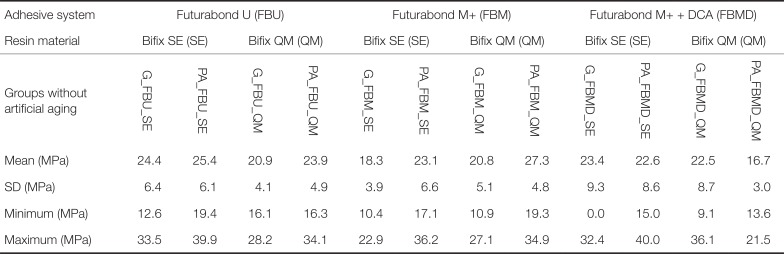
Table 2
Shear bond strength (SBS) of specimens with surface pretreatment by grinding (G) or plasma activation (PA), in combination with different adhesive systems and resin materials after artificial aging (A)




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download