Abstract
PURPOSE
Fractures, occlusal adjustments, or marginal corrections after removing excess composite cements result in rough surfaces of all-ceramic FPDs. These have to be polished to prevent damage of the surrounding tissues. The aim of this study was to evaluate the roughness of zirconia, silicate-ceramic, and composite after polish with different systems for intraoral use.
MATERIALS AND METHODS
Each set of 50 plates was made of zirconia, silicate-ceramic, and composite. All plates were ground automatically and were divided into 15 groups according to the treatment. Groups Zgrit, Sgrit, and Cgrit received no further treatment. Groups Zlab and Slab received glaze-baking, and group Clab was polished with a polishing device. In the experimental groups Zv, Sv, Cv, Zk, Sk, Ck, Zb, Sb, and Cb, the specimens were polished with ceramic-polishing systems “v”, “k”, and “b” for intraoral use. Roughness was measured using profilometry. Statistical analysis was performed with ANOVA and Scheffé-procedure with the level of significance set at P=.05.
RESULTS
All systems reduced the roughness of zirconia, but the differences from the controls Zgrit and Zlab were not statistically significant (P>.907). Roughness of silicate ceramic was reduced only in group Sv, but it did not differ significantly from both controls (P>.580). Groups Cv, Ck, and Cb had a significantly rougher surface than that of group Clab (P<.003).
All-ceramic restorations, especially full-contour restorations made of zirconia or silicate-ceramics, attract the interest of clinicians as well as patients because of their high aesthetics and biocompatibility. All-ceramic restorations are good and long-living alternatives to metal-ceramic restorations, although a risk of failure exists, which can be seen at forces below 500 N.123 Chipping fractures are the most frequent technical failures of veneered restorations.4 They often can be repaired using composites, as modern 10-MDP-based adhesive systems allow sufficient bonding between zirconia or silicate-ceramic and composite.567 Sometimes small fractures result in rough surfaces, which need to be polished. Rough surfaces can also be shown after occlusal adjustments.8 Beside technical failures, biological failures can occur, such as loss of vitality of the abutment-teeth, caries, or periodontitis. Biological failures might be triggered by high plaque adhesion on rough surfaces, e.g. after composite repair or after the cementation processes.9 Plaque adhesion, especially at crown margins and in the area of the cement gap, can cause damage to the periodontal tissues or cause secondary caries. Literature shows that rough occlusal surfaces can also cause abrasive wear of the antagonistic teeth.1011 To reduce both the risk of technical and of biological failures, polishing of the rough areas on fixed partial dentures (FPD) is necessary. Before cementation, rough surfaces can be finished extraorally, but if rough surfaces occur on a cemented FPD, an intraoral polishing is necessary. In these cases, either one ceramic material has to be polished, or the boundary areas of different ceramic materials and/or composites have to be polished. It is technically not possible to polish each material selectively (Fig. 1).
The aim of the current study was to evaluate the effectivity of different diamond-containing polishing systems on zirconia, veneering ceramic, and composite material using surface profilometry. The null hypothesis was that there is no difference in the surface roughness on zirconia, silicate-ceramic, and composite after polishing with the tested polishing systems.
Each set of 50 ceramic plates were cut out of CAD/CAM blocks of zirconia (Z) (8.5 × 6.0 × 2.0 mm) (InCoris Maxi-S, Sirona, Bernsheim, Germany) and of silicate-ceramic (S) (12.5 × 10.5 × 2.0 mm) (Ivoclar Vivadent AG, Schaan, Liechtenstein) using a precision diamond saw (IsoMed 4000, Buehler GmbH, Düsseldorf, Deutschland). To produce 50 composite plates, silicone impressions of the zirconia plates were taken. In the resulting moulds, nano-hybrid composite (C) (GrandioSO, VOCO GmbH, Cuxhaven, Germany) was applied manually using incremental technique to mimic the handling of composite for a direct intraoral reparation technique of a chipping fracture. The composite material was light cured using a polymerization lamp with 1.200 mW/cm2 (Bluephase, Ivoclar Vivadent AG, Schaan, Liechtenstein). To ensure identical surface roughness of all materials, all specimens were ground automatically with 165 µm grit silicon carbide paper (English Abrasives & Chemicals Ltd., London, UK) with a force of 50 N under water cooling using a universal grinding and polishing machine (PowerPro 5000, Buehler GmbH, Düsseldorf, Deutschland).
No further treatment was performed after the grinding process in the control groups Zgrit, Sgrit, and Cgrit to simulate the surface roughness after the intraoral use of diamond burs. The ceramic specimens in control groups Zlab and Slab received ceramic glaze firing after the grinding process. The composite specimens in control group Clab received high-gloss polish with the universal polishing machine up to 9 µm grit silicon carbide paper (English Abrasives & Chemicals Ltd., London, UK) under water cooling. In the experimental groups, three different polishing systems for intraoral use were tested (Table 1). These specimens were polished by the same dentist with a handpiece at 6000 rpm and under water cooling for 30 seconds per polishing step to achieve a high gloss finish. In all experimental groups, the first step of the polish was performed with a contact pressure of 2 N for 30 seconds. In the second step, the high gloss finish was performed with a contact pressure of 1 N for 30 seconds. A scale was used to keep a constant contact pressure of the polishing points to the ceramic surface, and a 30-second timer was used to ensure the correct polishing time during the experiments. According to clinical practice, the polishing points were guided with shifting and rotating movements over the surface of the specimen.
In groups Zv, Sv, and Cv, the specimens were polished using Dimanto made by VOCO GmbH (Dimanto, VOCO GmbH, Cuxhaven, Germany). This system is a single-stage polisher. According to the manufacturer's instructions, the diamond-containing rubber point was to be used with high pressure for pre-polishing and with low pressure for high-gloss finishing. In groups Zk, Sk, and Ck, the specimens were polished using a two-stage system made by Komet Dental (Zirkonpoliersystem, Komet Dental Gebr. Brasseler GmbH & Co KG, Lemgo, Germany). In groups Zb, Sb, and Cb, a two-stage system made by Busch & Co (Zirkon-/Keramikpoliersystem, BUSCH & CO GmbH & Co KG, Engelskirchen, Germany) was used. These systems include one polishing point for pre-polishing and a second one for the high gloss finish.
All specimens were cleaned with alcohol and dried with oil-free compressed air. After that, the surface roughness was measured using a surface profiler (Dektak 150 Surface Profiler, Bruker Corporation, Billerica, MA, USA). To measure the surface roughness, 5 parallel lines with a distance of 0.5 mm and a length of 3600 µm were scanned mechanically with a vertical and horizontal resolution of 0.33 µm. To evaluate the surface roughness, the arithmetic mean of the absolute values (Ra) was calculated.
The statistical analysis of Ra was performed with SPSS Statistics (Version 24, SPSS Inc., Chicago, IL, USA) using Kolmogorov-Smirnov Test, Levene Analysis, ANOVA and Scheffé procedure. Thereby the level of significance was set at P = .05.
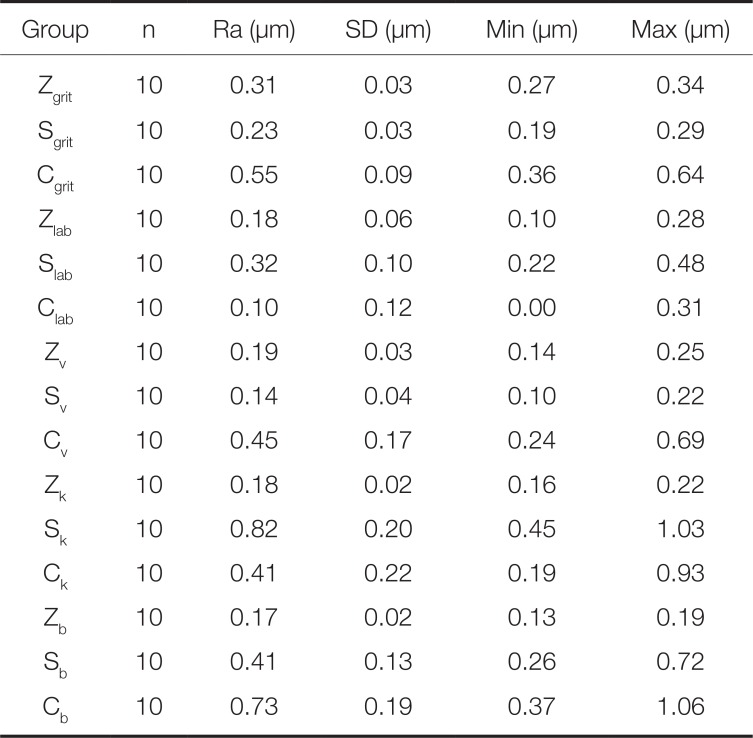
The data found by profilometry are shown in Table 2 and in Fig. 1. The Kolmogorov-Smirnov test showed a normal distribution of the data. Levene-Analysis proved homogeneity of the variances. ANOVA showed significant differences among the groups (P < .001). Scheffé procedure was used to identify significant differences in single comparisons.
At first, the surface roughness of the three materials after polishing with the different polishing-systems was compared.
It could be seen that all polishing systems were able to reduce the surface roughness of zirconia from originally 0.31 µm in group Zgrit to Ra-values below 0.20 µm in the test groups (Fig. 1). The differences to the control group Zgrit were statistically significant in the groups Zv (P < .001), Zk (P < .001), and Zb (P < .001). In comparison to the control group Zlab, the surface roughness of the groups Zv (P = .899), Zk (P = .987), and Zb (P = .986) did not differ significantly. Comparing the different polishing systems on silicate ceramic, the surface roughness after polishing with the VOCO-system in group Sv was significantly lower than after polishing with the Komet-system in group Sk (P < .001), with the Busch-system in group Sb (P < .001) and the control group Slab (P = .022). There was no significant difference between Sv and control group Sgrit (P = .487). The polishing with the Komet-system (Sk) resulted in a significantly increased surface roughness compared to the other groups Sgrit (P < .001), Slab (P < .001), Sv (P < .001) and Sb (P < .001). The surface roughness of silicate-ceramic after polishing with the Busch-system (Sb) was statistically different from those of groups Sv (P < .001), Sk (P < .001), and Sgrit (P = .032), but not from group Slab (P = .576). Having a closer look at the composite groups, no statistically significant differences were found between control group Cgrit and groups Cv (P = .790), Ck (P = .510), and Cb (P = .229). Compared to the lab-side polishing in group Clab, the surface roughness was significantly higher in groups Cv (P = .004), Ck (P = .014), and Cb (P < .001). Comparison between the polishing systems showed that the roughness in group Cv was significantly lower than that in group Cb (P = .015), but not than that in group Ck (P = .991). The surface roughness in group Cb was significantly higher than that in group Ck (P = .004). Roughnesses in groups Ck and Cv did not differ significantly (P = .991).
To get information about the possibility to polish interface areas between zirconia, silicate-ceramic, and composite, further comparisons between the different materials after polishing with the same polishing-systems are necessary.
Within the control groups Zgrit, Sgrit, and Cgrit, the surface roughness in group Cgrit was significantly higher than that in group Sgrit (P = .004), but not than that in group Zgrit (P = .182). Roughnesses in groups Zgrit and Sgrit did not differ (P > .999). Within the control groups Zlab, Slab, and Clab, the roughest surface was found in group Slab, and the smoothest surface was found in group Clab. The differences between the groups Zlab, Slab, and Clab were not statistically significant (P > .213). Data showed a high variation within the test groups in the surface roughness depending on the different polishing systems: After polishing with the VOCO System, the smoothest surface was found in group Sv followed by group Zv. The difference between Zv and Sv was not statistically significant (P > .999). The surface roughness in group Cv was significantly higher than that in group Sv (P = .004), but not than that in group Zv (P = .067). After the use of the Komet-system, the lowest surface roughness was found in group Zk followed by group Ck, but these two surfaces also showed no significant difference (P = .212). The surface roughness in group Sk was significantly higher than those in groups Zk (P < .001) and Ck (P < .001). After polishing with the Busch-system, the lowest surface roughness was found in group Zb followed by groups Sb and Cb. The comparisons between Zb and Cb (P < .001) and between Sb and Cb (P = .004) revealed statistically significant differences. The comparison between Zb and Sb did not show statistically significant result (P = .120).
In the current in-vitro study, some limiting factors have to be mentioned. A flat design of the specimens was chosen to guarantee an identical surface geometry for all materials at the beginning of the experiments. Further, the flat design was necessary for the profilometry. Unlike these experimental settings, most surfaces on crowns or bridges are curved. However, a flat surface design has been used in studies with similar aims.121314
Polishing of specimens in the test groups was performed manually. A dental handpiece was driven over the surfaces with shifting and rotating movements by an experienced dentist. This is in accordance to clinical practice because intraoral polishing always has to be done manually. The clinical outcome of intraoral polishing depends on various factors such as the contact pressure, the polishing time, and the rotation speed of the polishing points. To ensure comparable polishing conditions in all groups, the contact pressure of the polishing points and the polishing time were kept constant using a scale and a timer. All specimens were polished with water cooling at 50 ml/min and with 6000 rpm to reduce the risk of overheating followed by thermal induced phase transformation at the zirconia surfaces, which might lead to further surface roughness.
In the current study, a significant reduction of the roughness of the zirconia surface could be seen after polishing with all tested polishing systems. This is in line with the findings of Kou et al..12 The remaining surface roughness of zirconia is due to the mechanical properties and the mechanical hardness of densely sintered zirconia. For intraoral adjustments of zirconia surfaces, red (~46 µm grit) or yellow (~25 µm grit) diamond burs are normally used. These adjustments leave scratches on the surfaces, which have to be polished to avoid wear of the antagonist.15 The polishing of zirconia is not a classical polishing process, but it is rather a mechanical micro-abrasion of material peaks.16 Remaining micro scratches are not filled by plastified material as it can be seen during polishing of resin or metal. This means the surface quality depends on the hardness of the material and on the grit of the diamond particles in the polishing points. After labside glaze firing of ceramic specimens and after labside polish of composite specimens, the surface roughness in groups Zlab, Slab, and Clab could be reduced below 0.2 µm in average. In zirconia, all tested polishing systems left a surface roughness, which did not differ significantly from surface roughness after the glaze firing process. This is in line with Hmaidouch et al., who also found no difference between glazed zirconia and fine polished zirconia.14 Intraoral polishing of zirconia seems to be an alternative to glaze firing previous to cementation. Further, the results of this study show that it is possible to polish the surface of cemented zirconia restorations after intraoral adjustment with rotating diamond containing rubber points. This is in line with the current literature. Park et al. concluded that “zirconia polishing systems showed excellent ceramic surface polishing”.17
The effects of silicate-ceramic polishing differed significantly among the polishing systems. Only in group Sv the surface roughness was decreased in comparison to those of the control groups and in comparison to the surface roughness of zirconia in the corresponding group Zv. The other two polishing systems showed a significantly increased roughness compared to their corresponding zirconia groups, but different trends were shown in comparison to the composite groups. Surface polishing of silicate-ceramic is a combination of filling scratches with liquified glass matrix the polishing procedure and removing surface peaks with the diamond particles. Depending on the grit and on the contact pressure of the polishing points, the diamond particles might cause new scratches during the polishing process. These new scratches might be lower in group Sv because the polishing points of the single step system become blunter from use than polishing points of the two-step systems. This might be the reason for the higher surface roughness in two-step groups Sb and Sk in comparison to the lower surface roughness in the one-step group Sv.
Veneered ceramic restorations have interface areas between zirconia and silicate ceramic and after adhesive cementation between composite and zirconia (Fig. 2). If an intraoral repair of a chipping fracture with composite is necessary, interface areas between ceramic material and composite occur (Fig. 2). In these cases, it might be necessary to remove an excess of composite material after the hardening processes with rotating instruments. Remaining roughness, especially in the marginal areas, might cause a high plaque accumulation. For that reason, an accurate polishing of these interfaces is necessary. The results of the current study show that the surface roughness of composite after polishing with the tested systems differed. It can be assumed the reasons for this variation are the same as for the variation of the surface roughness of silicate-ceramics after polishing, which has been described in the previous paragraph.
The surface roughness after polishing of a ceramic or composite surface needs to be compared to the natural enamel roughness and to polishing results of other research groups. The surface roughness of natural enamel is reported to be 0.27 µm ± 0.19 µm.18 As all polishing system of the current study produced a similarly low surface roughness on zirconia, these systems can be absolutely recommended for surface treatment of zirconia. The same recommendation is justified for polishing silicate ceramic with the VOCO system. Exemplary polishing results of other studies show a surface roughness of 0.24 µm to 0.79 µm for silicate-ceramics and 0.12 µm to 0.2 µm for zirconia.192021 For composite, the reported data range from 0.14 µm to 0.86 µm.2223 In 1997 Bollen et al.24 showed a reduction of dental plaque adhesion to surfaces with surface roughness below 0.20 µm. The results of the current study (Table 2) are in line with these studies.
The null hypothesis that there was no difference of the surface roughness on zirconia, silicate-ceramic, and composite after polishing with the tested polishing systems has to be rejected: The surface roughness of silicate-ceramic and composite differed hugely after applying the same polishing system.
Within the limitations of this study, it can be concluded that all of the tested polishing systems were able to produce clinically acceptable surface qualities on zirconia with surface roughness comparable to natural enamel. It is possible to polish zirconia surfaces with modern diamond-containing polishing systems for intraoral use after occlusal adjustments. Concerning the interface areas between zirconia, veneering material, and composite material, polishing should be performed with diamond containing polishing systems for zirconia at first, followed by special polishing systems for veneering materials and for composite materials to achieve an optimal outcome. The data of this study suggests that the order of different polishing systems for different materials seems to have an immense influence on the result of intraoral polishing of interface areas between different materials for fixed partial dentures. Further research is necessary to find a suitable protocol for the clinical polishing process of interface areas between different materials for fixed partial dentures and their repairs and for adhesive luting cements.
References
1. Kassardjian V, Varma S, Andiappan M, Creugers NH, Bartlett D. A systematic review and meta analysis of the longevity of anterior and posterior all-ceramic crowns. J Dent. 2016; 55:1–6. PMID: 27594093.

2. Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs). Dent Mater. 2015; 31:603–623. PMID: 25842099.

3. Bömicke W, Rues S, Hlavacek V, Rammelsberg P, Schmitter M. Fracture Behavior of Minimally Invasive, Posterior, and Fixed Dental Prostheses Manufactured from Monolithic Zirconia. J Esthet Restor Dent. 2016; 28:367–381. PMID: 27562053.

4. Thoma DS, Sailer I, Ioannidis A, Zwahlen M, Makarov N, Pjetursson BE. A systematic review of the survival and complication rates of resin-bonded fixed dental prostheses after a mean observation period of at least 5 years. Clin Oral Implants Res. 2017; 28:1421–1432. PMID: 28191679.
5. Lee SJ, Cheong CW, Wright RF, Chang BM. Bond strength of the porcelain repair system to all-ceramic copings and porcelain. J Prosthodont. 2014; 23:112–116. PMID: 23725343.

6. Özcan M. Intraoral repair protocol for chipping or fracture of veneering ceramic in zirconia fixed dental prostheses. J Adhes Dent. 2015; 17:189–190. PMID: 25969842.
7. Pott PC, Stiesch M, Eisenburger M. Influence of artificial aging on the shear bond strength of zirconia composite interfaces after pretreatment with new 10-MDP adhesive systems. J Dent Mater Tech. 2016; 5:1–9.
8. Sarac D, Sarac YS, Yuzbasioglu E, Bal S. The effects of porcelain polishing systems on the color and surface texture of feldspathic porcelain. J Prosthet Dent. 2006; 96:122–128. PMID: 16911889.

9. Blank JT. Optimize finishing and polishing of posterior composites. Dent Today. 2014; 33:118120–121.
10. Hmaidouch R, Weigl P. Tooth wear against ceramic crowns in posterior region: a systematic literature review. Int J Oral Sci. 2013; 5:183–190. PMID: 24136675.

11. Stober T, Bermejo JL, Rammelsberg P, Schmitter M. Enamel wear caused by monolithic zirconia crowns after 6 months of clinical use. J Oral Rehabil. 2014; 41:314–322. PMID: 24447258.
12. Kou W, Molin M, Sjögren G. Surface roughness of five different dental ceramic core materials after grinding and polishing. J Oral Rehabil. 2006; 33:117–124. PMID: 16457671.

13. Subaşı MG, İnan Ö. Evaluation of the topographical surface changes and roughness of zirconia after different surface treatments. Lasers Med Sci. 2012; 27:735–742. PMID: 21786139.

14. Hmaidouch R, Müller WD, Lauer HC, Weigl P. Surface roughness of zirconia for full-contour crowns after clinically simulated grinding and polishing. Int J Oral Sci. 2014; 6:241–246. PMID: 25059249.

15. Sun S, Liang R, Ren J, Xu Y, Zhao Y, Meng H. Influence of polishing and glazing on the wear of zirconia and enamel. Zhonghua Kou Qiang Yi Xue Za Zhi. 2016; 51:300–304. PMID: 27220391.
16. Aghan RL, Samuels LE. Mechanism of abrasive polishing. Wear. 1970; 16:293–301.
17. Park C, Vang MS, Park SW, Lim HP. Effect of various polishing systems on the surface roughness and phase transformation of zirconia and the durability of the polishing systems. J Prosthet Dent. 2017; 117:430–437. PMID: 28088308.

18. Preis V, Behr M, Handel G, Schneider-Feyrer S, Hahnel S, Rosentritt M. Wear performance of dental ceramics after grinding and polishing treatments. J Mech Behav Biomed Mater. 2012; 10:13–22. PMID: 22520415.

19. Aravind P, Razak PA, Francis PG, Issac JK, Shanoj RP, Sasikumar TP. Comparative evaluation of the efficiency of four ceramic finishing systems. J Int Oral Health. 2013; 5:59–64.
20. Amer R, Kürklü D, Kateeb E, Seghi RR. Three-body wear potential of dental yttrium-stabilized zirconia ceramic after grinding, polishing, and glazing treatments. J Prosthet Dent. 2014; 112:1151–1155. PMID: 24836531.

21. Preis V, Schmalzbauer M, Bougeard D, Schneider-Feyrer S, Rosentritt M. Surface properties of monolithic zirconia after dental adjustment treatments and in vitro wear simulation. J Dent. 2015; 43:133–139. PMID: 25174949.

22. Rai R, Gupta R. In vitro evaluation of the effect of two finishing and polishing systems on four esthetic restorative materials. J Conserv Dent. 2013; 16:564–567. PMID: 24347895.

23. Kamonkhantikul K, Arksornnukit M, Takahashi H, Kanehira M, Finger WJ. Polishing and toothbrushing alters the surface roughness and gloss of composite resins. Dent Mater J. 2014; 33:599–606. PMID: 25273038.

24. Bollen CM, Lambrechts P, Quirynen M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: a review of the literature. Dent Mater. 1997; 13:258–269. PMID: 11696906.
Fig. 2
Possible localizations on partial restorations or crowns for intraoral polish (red lines) with varying number of involved materials. White = enamel, beige = silicate-ceramic, green = zirconia, purple = composite material.
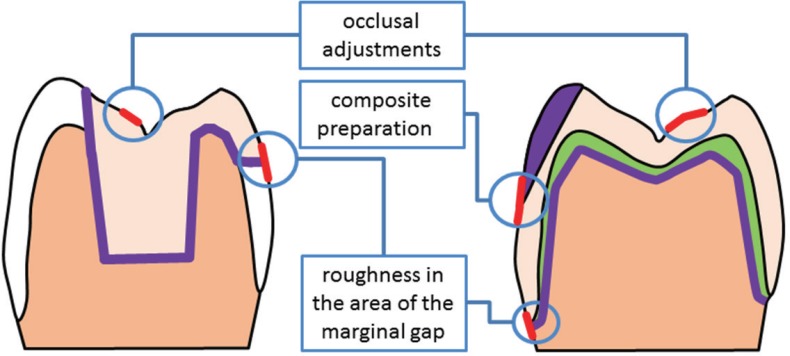
Table 1
overview over control groups and test groups
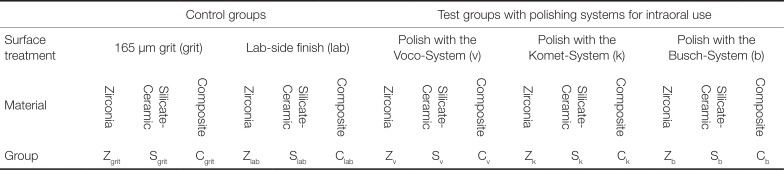
Table 2
Descriptive analysis of the data




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download