This article has been
cited by other articles in ScienceCentral.
Abstract
PURPOSE
Conventional resin-bonded fixed partial dentures (RBFPDs) are usually made with a two-retainer design. Unlike conventional RBFPDs, cantilever resin-bonded fixed partial dentures (Cantilever RBFPDs) are, for their part, made with a single-retainer design. The aim of this study was to compare the effect of tooth surface preparation on the bond strength of zirconia cantilever single-retainer RBFPDs. The objective is to evaluate the shear bond strength of these single-retainer RBFPDs bonded on 3 different amount of tooth surface preparation.
MATERIALS AND METHODS
Thirty extracted bovine incisors were categorized to 3 groups (n=10), with different amounts of tooth surface preparations. Teeth were restored with single-retainer RBFPDs with different retainer surfaces: large retainer of 32 mm2; medium retainer of 22 mm2; no retainer and only a proximal connecting box of 12 mm2. All RBFPDs were made of zirconia and were bonded using an adhesive system without adhesive capacity. Shear forces were applied to these restorations until debonding.
RESULTS
Mean shear bond strength values for the groups I, II, and II were 2.39±0.53 MPa, 3.13±0.69 MPa, and 5.40±0.96 MPa, respectively. Statistical analyses were performed using a one-way ANOVA test with Bonferroni post-hoc test, at a significance level of 0.001. Failure modes were observed and showed a 100% adhesive fracture.
CONCLUSION
It can be concluded that the preparation of large tooth surface preparation might be irrelevant. For zirconia single-retainer RBFPD, only the preparation of a proximal connecting box seems to be a reliable and minimally invasive approach. The differences are statistically significant.
Keywords: Cantilever fixed partial denture, Shear force, Resin bonded fixed partial denture, Single-retainer, Zirconia
INTRODUCTION
The rehabilitation of a single missing anterior tooth has always been a challenge for the clinician. Several rehabilitation options are available, such as the use of dental implant, fixed partial denture, or removable partial denture.
First described in the 1970s, resin-bonded fixed partial denture (RBFPD) has long been a reliable and minimally invasive treatment option. RBFPDs can be made using a two-retainer configuration or a single-retainer configuration.
1
In a study of Kern,
1 the author reported an excellent clinical longevity for anterior ceramic RBFPDs. He reported a 5-year survival rate of 73.9% for the RBFPDs with a two-retainer design versus 92% for those with a single-retainer design. Other authors also reported high survival rates.
2
Even though RBFPDs were widely used for decades, it had suffered from some disadvantages, often related to frequent debonding, appearance of dramatic decays under the abutment teeth, and the unaesthetic use of metal for the infrastructure and retainer.
3 This is often due to a misunderstanding about the tooth preparation design, retainer design, choice of material, choice of adhesive system, and choice of abutment tooth.
Adhesive dentistry is a large part of our everyday practice. Non-precious metal is still the gold standard material for RBFPDs infrastructure and retainer, as it has adequate rigidity to the system.
4 However, the use of new ceramic material, such as zirconia, seems appealing. Proper recommendations for the use of these new materials are missing, leading to an increase in the failure rates.
The aim of this study was to compare the effect of tooth preparation surface on the bond strength of zirconia cantilever single-retainer RBFPDs to tooth structure. The objective of this study is to evaluate the shear bond strength of these single-retainer RBFPDs bonded on 3 different tooth surface preparations (large, medium, and small).
MATERIALS AND METHODS
Thirty extracted bovine incisors were observed under a stereomicroscope (×20 magnification) and then selected for their absence of decay, fracture, and crack. They were immediately stored in physiological serum after extraction (at room temperature).
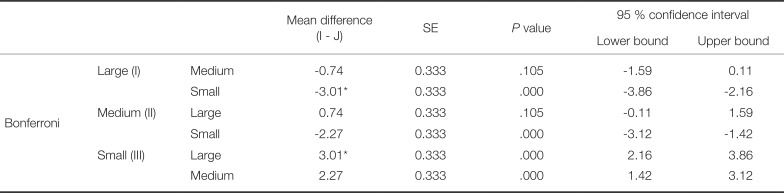
The teeth were randomly allocated into 3 groups (n = 10). For each group, 3 different amounts of tooth surface preparations were applied (
Fig. 1):
- Group I: retainer with a surface of 20 mm2 + proximal box with a surface of 12 mm2
- Group II: retainer with a surface of 10 mm2 + proximal box with a surface of 12 mm2
- Group III: no retainer and only a proximal box with a surface of 12 mm2
The preparations of the abutment teeth were performed according to a strict protocol.
1
Group I + II:
1. Preparation of a small chamfer (rounded internal shoulder) at the cervical level on a supra-gingival position, with a depth of 0.6 – 0.8 mm, using a Dumont chamfer bur 3850-016-3, which is a tapered round long bur with a head diameter of 1.6 mm. In order to standardize the depth of the preparations, only half of the bur length is penetrated in each tooth.
2. Preparation of an occlusal ledge (Dumont chamfer bur 8021-3.)
3. Preparation of an off-centerd macro-pit, which is located opposite to the edentulous area (Dumont round bur 023).
Group I + II + III:
4. Preparation of a connecting box next to the edentulous area, using a Dumont chamfer bur 3850-016-3 (tapered long round bur). This box is mandatory for ceramic RBFPDs (InCeram, Alumina, or Zirconia). The ideal dimension of the box for an anterior RBFPD is 4 mm height by 3 mm width, or a connecting area of 12 mm2.
Each tooth is placed in a rectangular mould. The root is dipped in a thermo-polymerizable resin (Orthocryl, Dentaurum, Germany) consisting of a powder and a liquid so that the tooth-prosthetic junction exceeds by 2 mm from the supporting resin. The specimens are placed in a pressure pan at 2.5 bars.
The RBFPDs are made using the Exocad software (Exocad GmbH, Darmstadt, Germany) and the sizes of retainers and connecting area were recorded with an optical impression using the Solutionix identitica SE scanner. The Exocad software gives access to the exact value of the contact surfaces, which were recorded for each element. All the retainers were made with a 1 mm thickness, and controlled using a caliper.
After the fabrication, the intaglio surfaces of each RBFPD were treated using airborne particle abrasion at 0.5 bar with 50 µm alumina oxide according to Kern et al.
5 protocol. RBFPD were bonded according to Panavia V5 manufacturer's instructions.
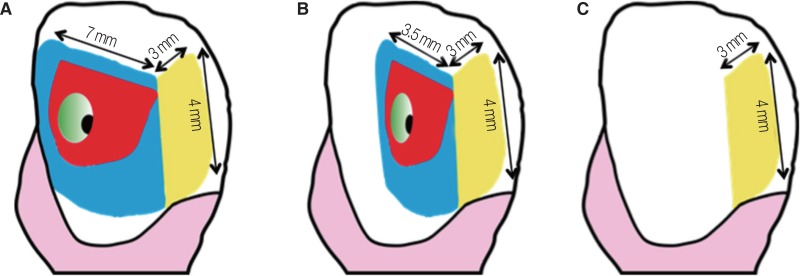
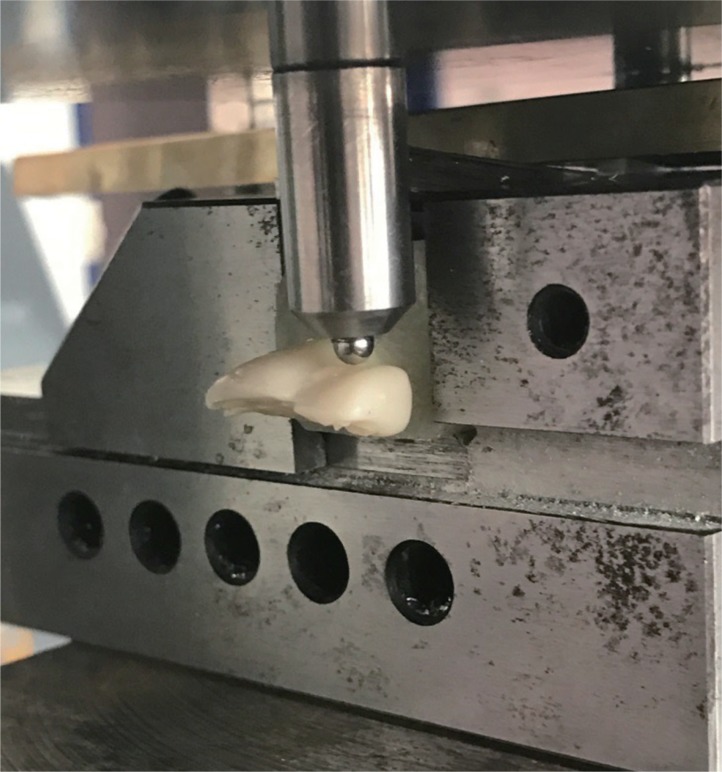
The restorations were subjected to shear bond test (
Fig. 2). The load was applied at a speed of 1 mm/min, on the center of the buccal surface of the RBFPD (the same point of application of the forces is used for all the samples;
Fig. 3) using a universal testing machine (Lloyd LRX, Largo, TX, USA). The each tooth was given an inclination of 90° to the vertical plane. The values obtained were recorded and analyzed with a one-way ANOVA using IBM SPSS Statistics software version 24 (Statistical Package for Social Sciences, SPSS Inc., Chicago, IL, USA), with Bonferroni post-hoc test.
After each test, the sample was analyzed under a stereomicroscope (at ×20 magnification) to determine the fracture mode.
RESULTS
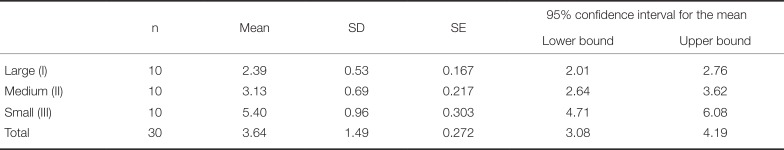
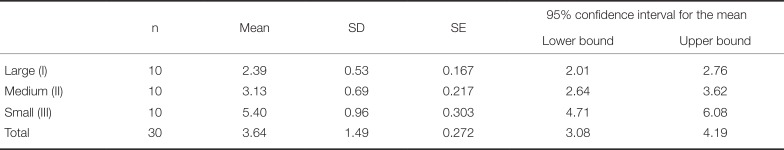
The mean shear bond strength values of zirconia RBFPD are shown in
Table 1.
The mean shear bond strengths for groups I, II, and III are 2.39 ± 0.53 MPa, 3.13 ± 0.69 MPa, and 5.40 ± 0.96 MPa. Mean shear bond strength values increases as the tooth surface preparation decreases. Group III (small surface area) shows higher mean shear bond strength compared to groups II (medium surface area) and I (large surface area).
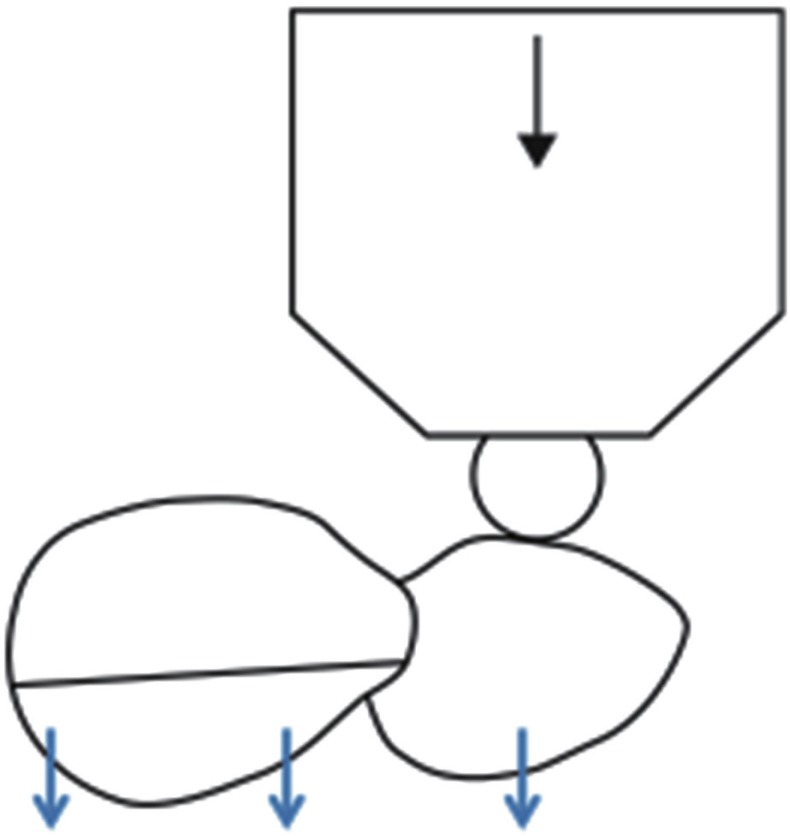
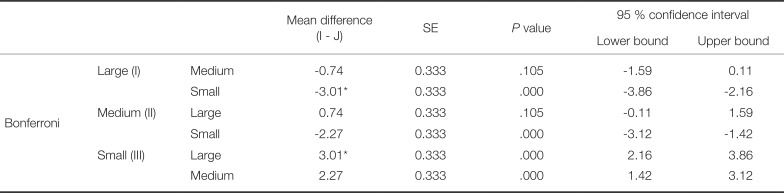
The statistical analysis was performed using a one-factor ANOVA test with Bonferroni post-hoc test and showed highly significant differences (
P < .001;
Table 2). The differences are highly significant (
P > .001). Group II shows higher shear bond strength compared to group I. However, the differences are not significant (
P = .105).
DISCUSSION
RBFPD is a very reliable option for the replacement of a missing tooth and presents many advantages, such as minimally invasive, cost effective, and less time consuming procedure.
4 However, it is a very technique-sensitive procedure, and it requires the clinician to be skilled and to properly plan the case.
23
RBFPDs are usually designed with two different configurations: two-retainer design and single-retainer design.
1 RBFPDs with two-retainer design have been used for decades. However, it presented some drawbacks such as frequent partial debonding on one of the two retainers.
6 When the patient is not aware of the debonding, it may lead to the appearance of dramatic decays under the debonded abutment tooth.
7 The debonding may be explained by different tooth mobility between the abutment teeth. During protrusion, whenever the force moves from the retainer to the abutment tooth surface, it creates a differential movement of that abutment tooth and a resistance from the other abutment tooth. This can lead to early partial debonding on one of the abutment teeth.
8910
To overcome this later complication, some authors have recommended the used of cantilever single-retainer RBFPD.
1478910 This will limit the partial debonding, which was reported as the main source of failure.
Due to advances in adhesive dentistry, new ceramic materials presenting upgraded mechanical properties, and increased demand from patients of aesthetic and metal-free procedures, the use of ceramo-ceramic RBFPDs such as zirconia has gained increased popularity.
In a study by Kern
1 in 2005, the author compared the clinical survival rate over a period of 10 years of ceramo-ceramic RBFPD (In-ceram and feldspathic stratification), presenting one- and two-retainer design. Kern observed that the number of cracks or debonding of the cantilever single-retainer design was lower compared to the conventional two-retainer design.
The success rate was evaluated by the in-situ presence of the restoration and the absence of fracture. The success rate for the two-retainer design was 67.3% compared to 92.3% for the single-retainer design.
111 This important difference highlighted the fact that cantilever single-retainer RBFPD is an alternative option to the conventional two-retainer design.
van Dalen et al.
12 carried out a review of the literature concerning the debonding rates of RBFPDs with two-retainer design and with single-retainer design. Their results were in accordance to those of Kern and Sasse.
11
Our study showed higher shear bond strength for the group 3, which present a small tooth preparation surface. These results are encouraging. In traditional thinking, an increased bonding surface would improve the adhesion. In his study, Kern advocated the preparation of a palatal/lingual veneer, a cingulum groove, and a box on the proximal surface on the side of the missing tooth. Within the limit of our results, it seems that the preparation of the only proximal box would confer enough bond strength. More researches are needed to confirm our findings. This would then create new clinical perspectives, as we could imagine preparing less abutment teeth, and perhaps even avoiding any preparation. The overall low SBS values obtained could be explained by our choice to apply the load in the centre of the buccal surface of the extended tooth, which is the most unfavourable situation. This does not reflect a normal clinical situation. However, this could happen in case of trauma on the anterior upper teeth.
The analysis of the failure modes showed 100% adhesive fractures at the adhesive-zirconia interface. In the case of alumina or zirconia ceramics, the glass phase is usually low or non-existent, and therefore it does not allow its adequate adhesion. However, has been observed satisfactory adhesion when using Panavia.
13 Panavia contains MDP groups, which has intrinsic adhesive potential to metal oxides such as aluminium and zirconium.
Usually, adhesive systems with adhesive capacity, such as Panavia F 2.0, contain adhesive monomer within the resin paste. These monomers tend to give the paste a bluish and opaque aspect. However, for Panavia V5, MDP monomers have been removed from the paste and left in the primer. This might have decreased the adhesive potential provided by the MDP monomer.
The advances in adhesive dentistry led us to reconsider the influence of the tooth preparation design on bond strength.
CONCLUSION
Zirconia cantilever single-retainer RBFPD can be considered as an aesthetic, reliable, minimally invasive, cost- and time-effective option for the rehabilitation of a missing single anterior tooth. It should be presented to the patient as a viable alternative to implant therapy.
Within the limit of our study, we could conclude that the preparation of a proximal surface would provide a better shear bond strength compared to larger tooth surface preparation.
Fig. 1
Picture of the teeth, where the future preparation surfaces are colored. The colors represent the different steps to prepare tooth. (A) Group I, (B) Group II, (C) Goup III.
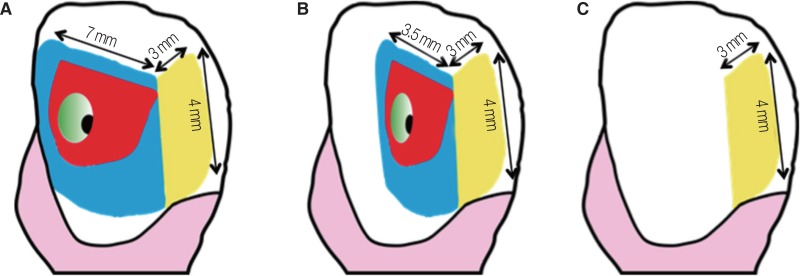
Fig. 2
Point of application of the shear forces and illustration of the device.
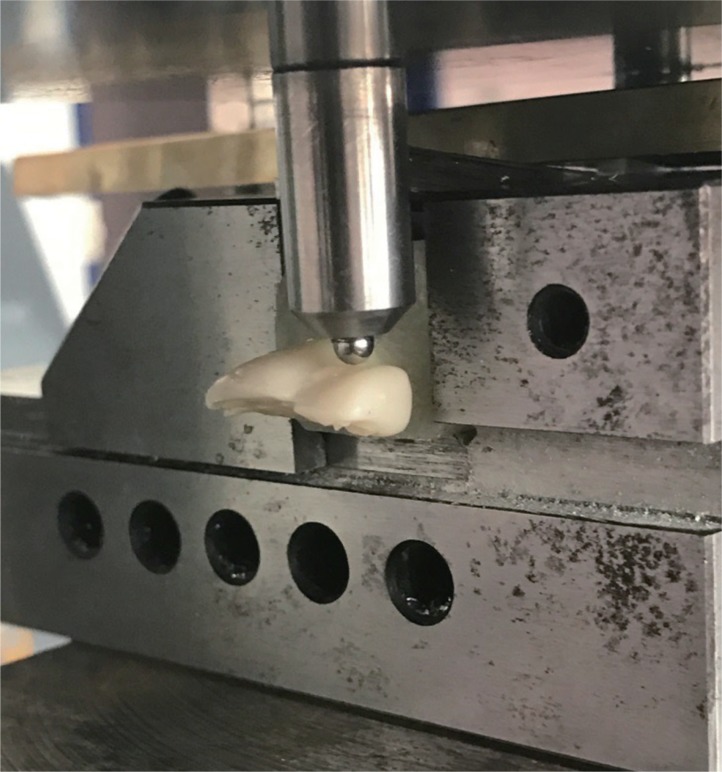
Fig. 3
Schematic representation of the shear forces applied on the buccal surface of the RBFPD. When the force is applied on the cantilever element (the right tooth) from the buccal side, teeth displacement is uniform and takes away the natural tooth bonded with the cantilever.
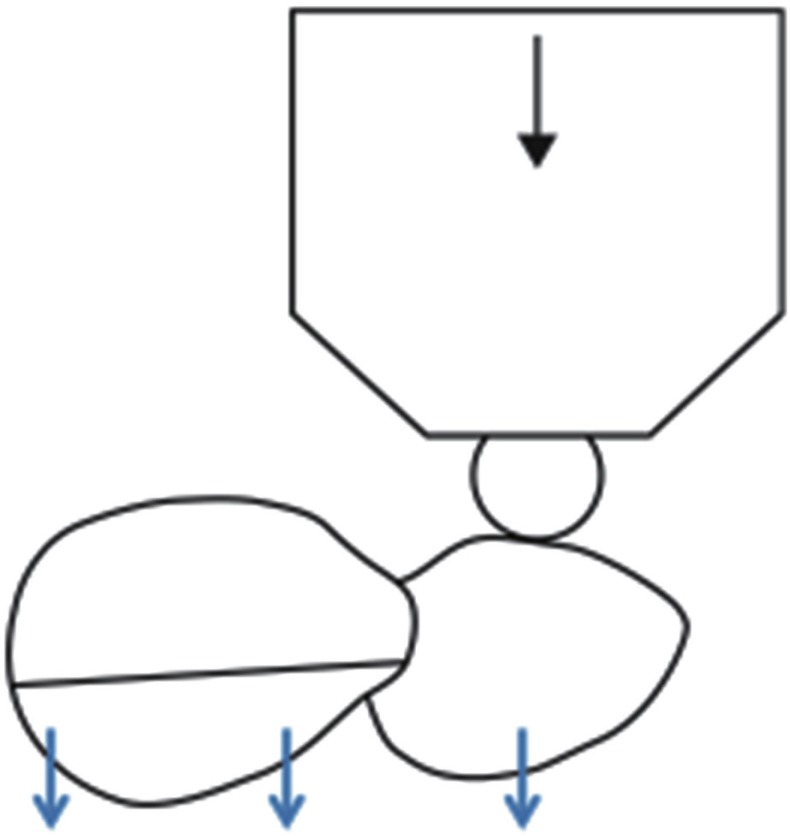
Table 1
Mean shear bond strength values (MPa)
|
n |
Mean |
SD |
SE |
95% confidence interval for the mean |
|
Lower bound |
Upper bound |
|
Large (I) |
10 |
2.39 |
0.53 |
0.167 |
2.01 |
2.76 |
|
Medium (II) |
10 |
3.13 |
0.69 |
0.217 |
2.64 |
3.62 |
|
Small (III) |
10 |
5.40 |
0.96 |
0.303 |
4.71 |
6.08 |
|
Total |
30 |
3.64 |
1.49 |
0.272 |
3.08 |
4.19 |
Table 2
Pairwise comparison of 3 different tooth surface preparations at 0.001 significance level
|
Mean difference (I - J) |
SE |
P value |
95 % confidence interval |
|
Lower bound |
Upper bound |
|
Bonferron |
Large (I) |
Medium |
−0.74 |
0.333 |
.105 |
−1.59 |
0.11 |
|
Small |
−3.01*
|
0.333 |
.000 |
−3.86 |
−2.16 |
|
Medium (II) |
Large |
0.74 |
0.333 |
.105 |
−0.11 |
1.59 |
|
Small |
−2.27 |
0.333 |
.000 |
−3.12 |
−1.42 |
|
Small (III) |
Large |
3.01*
|
0.333 |
.000 |
2.16 |
3.86 |
|
Medium |
2.27 |
0.333 |
.000 |
1.42 |
3.12 |




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download