Abstract
PURPOSE
The purpose of this study was to evaluate the effect of the zirconia surface architecturing technique (ZSAT) on the bond strength between veneering porcelain and zirconia ceramic.
MATERIALS AND METHODS
20 sintered zirconia ceramic specimens were used to determine the optimal surface treatment time, and were randomly divided into 4 groups based on treatment times of 0, 1, 2, and 3 hours. After etching with a special solution, the surface was observed under scanning electron microscope, and then the porcelain was veneered for scratch testing. Sixty 3 mol% yttria-stabilized tetragonal zirconia polycrystal ceramic blocks were used for tensile strength testing; 30 of these blocks were surface treated and the rest were not. Statistical analysis was performed using ANOVA, the Tukey post-hoc test, and independent t-test, and the level of significance was set at α=.05.
RESULTS
The surface treatment of the zirconia using ZSAT increased the surface roughness, and tensile strength test results showed that the ZSAT group significantly increased the bond strength between zirconia and veneering porcelain compared to the untreated group (36 MPa vs. 30 MPa). Optimal etching time was determined to be 2 hours based on the scratch test results.
Dental restorations must have optimal properties including biocompatibility, electrochemical stability, and aesthetics. A gradual increase in aesthetic requirements in dental applications has expanded the usage of zirconia, which is a high strength ceramic having excellent mechanical properties. Zirconia is used for both anterior and posterior areas, both of which require strong loads.123 The number of clinical research papers about zirconia has increased due to the increase in both interest and clinical applications of this new material456. However, there are few mid-term studies having results with more than five years of data.
In 2007, Sailer et al.7 published a 5-year follow-up study on 57 zirconia bridges (Cercon) cemented with resin cement. The results showed 12 failure cases due to secondary caries and abutment fracture. No zirconia framework fractures were observed except for one case of trauma. Molin and Karlsson8 reported a 100% success rate of 19 three-unit zirconia bridges over a 5-year period of observation. Another study by Sorrentino et al.9 showed a 100% survival rate of 48 three-unit zirconia bridges, and they found only three cases of minor chipping of veneering material without any decementation of the prosthesis or fracture of the framework. Not all studies showed a 100% survival rate. For example, Ortorp et al.10 reported an 88.8% success rate of 143 single zirconia crowns. Vigolo and Mutinelli compared conventional porcelain-fused to metal (PFM) and zirconia crowns (Procera, LAVA) on mandibular molars, and these showed no statistical differences among the groups. More clinical problems such as chipping of the veneering porcelain were observed in zirconia groups.11 In 2012, Raigrodski et al.12 reported the excellent function of 20 zirconia bridges despite four cases of veneer fracture in a 5-year follow-up study. Schmitter et al.13 confirmed the structural stability of zirconia as long as proper connector dimensions were secured. They reported two cases of zirconia framework fracture out of 36 long span bridges over a 5-year observation period; these fractures were attributed to reduced connector dimensions.
On the other hand, zirconia showed a relatively high frequency of veneer fracture compared to PFM prostheses.781011121314 Each zirconia system was developed with an optimized porcelain and framework design to minimize chipping of the veneering porcelain, but these designs are still incomplete. Another approach using heat pressing or sintering with computer aided design/computer aided manufacturing (CAD/CAM) lithium disilicate has been introduced. However, fractures were also reported and there is a lack of supporting data. Overall, chipping of veneering porcelain in zirconia prostheses is an ongoing problem with no clear solution at this moment.15 Therefore, there is a need to improve the surface characteristics of zirconia ceramics to provide better physical and chemical bond strength.
ZSAT is an etching technique that employs a mixed solution of nitric acid and fluoric acid provided by Bioden Inc.. ZSAT may increase bond strength between zirconia and veneering materials and be attributed to improvement in mechanical bonding due to micro-roughness.
The purpose of this investigation was to improve bond strength between porcelain and zirconia ceramics via chemical surface treatment on zirconia ceramics. The null hypothesis of this study was that the ZSAT surface treatment, regardless of treatment time, would not increase the bond strength between veneering porcelain and zirconia ceramic.
For surface treatment and scratch test, a total of 20 specimens of sintered zirconia ceramic (3Y-TZP, Acucera Inc., New York, NY, USA) were used for the experiments, and these were randomly divided into 4 groups. ZSAT is an etching technique that employs a 5:5 mixed solution of nitric acid and fluoric acid stock solution provided by Bioden Inc. (ZIRCOS-E etching solution, Lot. No. 1130312EJ50, Seoul, Korea). The etching was performed for 0, 1, 2, and 3 hours, and these groups were designated groups A, B, C, and D, respectively. After etching, the specimens were washed completely for 3 minutes.
After the surface treatment was done, an even thickness of porcelain powder was applied, and the final porcelain-fused zirconia specimen was finished with heat treatment. The final thickness of the porcelain was about 0.2 mm. The treated surface of the zirconia ceramic was observed under SEM (FESEM, JEOL JSM-6700F, Tokyo, Japan) with a magnification of 250×, and the bond strength between the zirconia ceramic and porcelain was measured using the scratch test method.
Another 60 rectangular column blocks (5 × 5 × 10 mm) were made with 3Y-TZP blocks (Acucera Inc., Pocheon, Korea) after sintering for 2 hours at 1550℃ for tensile strength test. Mirror surface finishing was performed, and then 30 blocks were treated with ZSAT for 2 hours at room temperature. A control group of another 30 specimens did not receive the surface treatment. Then, porcelain powders were applied, and these were fired for 30 seconds at 920℃. Tensile strength testing of the zirconia-porcelain binding area was performed using a push-pull tension gauge 5005 (Imada Co., Ltd., Toyohashi, Japan) (Fig. 1).
Quantile-quantile plots and Shapiro-Wilk tests were used to test the normality of dependent variables (adhesive strength and tensile strength). Data were observed near the diagonal in the Quantile-Quantile plot, and the Shapiro-Wilk tests showed normality (P > .05). Therefore, parametric statistics were applied, including analysis of variance (ANOVA), to evaluate the effects of etching time on bonding strength between the zirconia coping and the veneering porcelain. A Tukey post-hoc test was used to determine if significant results were found. An independent t-test was used to test the effect of etching on the tensile strength between zirconia coping and veneering porcelain. Statistical analyses were performed with a PASW 18.0 (IBM Co., New York, NY, USA), and the level of significance was set at α = .05.
Changes in the surface of the zirconia ceramics were observed over time, especially where the zirconia surface was etched by acid. Etching formed indentations on the surface, which were intensified as treatment time increased (Fig. 2).
In scratch test, the adhesive strengths (in MPa) between the zirconia ceramic and veneering porcelain were 30.22 ± 1.53, 32.55 ± 1.23, 36.50 ± 1.25, and 32.09 ± 1.84 for groups A, B, C, and D, respectively (Table 1). Based on this result, the optimal treatment time to achieve the best adhesive strength for ZSAT was 2 hours, which was applied for the next tensile strength test.
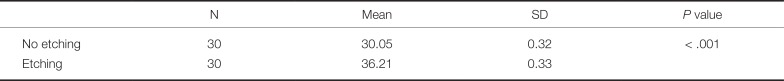
Tensile strength measurements of the zirconia ceramic and veneering porcelain bond showed better results in the etched experimental group (36.21 ± 0.33 MPa) than the non-etched control group (30.05 ± 0.32 MPa) (Table 2).
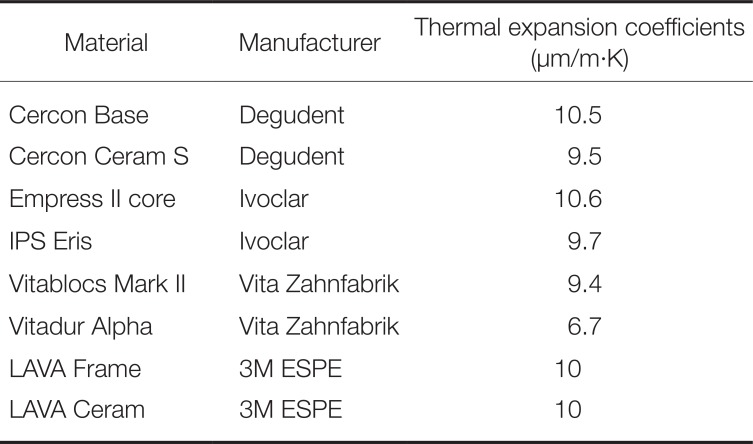
In order to understand the bonding between cores and veneering materials, we determined the thermal expansion coefficient of both materials and investigated the bond failure mode. Thermal expansion coefficients of the core and veneering materials should be similar, and the core must have slightly higher values than the veneering material for metal core-porcelain veneering. This suggests that relatively more shrinking must occur in the metal core, which induces a compressive residual stress that strengthens the veneering layer. If the difference in thermal expansion coefficients is large, the relatively brittle veneering material may fracture. The mode of fracture could be different depending on the mismatch in thermal expansion. If the thermal expansion coefficient of the metal is lower than the veneering material, the tensile force works on the veneering layer, which induces a tangential crack. On the other hand, in the opposite case, compressive stress will affect the veneering layer, inducing radial cracks. It is desirable that the difference in thermal expansion coefficient is less than 0.5 × 10−6/℃ for metal core-porcelain veneering.16
Unlike metal-porcelain bonding, there is not much known about zirconia-porcelain bonding. Several variables such as the surface condition of the zirconia core, residual stress due to the difference in thermal expansion coefficient, interfacial flaws or defects, and surface wettability and shrinkage of the veneering material may affect the bond strength of zirconia-veneering porcelain.17 To prevent fracture in the veneering material, a slight difference in thermal expansion coefficient could be used to induce light compressive forces on the veneer. However, Murphy et al.18 reported that a 2 × 10−6/K higher thermal expansion coefficient in the zirconia core could induce tensile forces on the veneering material, which results in fracture of the veneer. If there is a big difference in thermal expansion coefficients between the core and veneering material, a compressive or tensile stress will be applied to the veneering material. If the thermal expansion coefficient of the core material is the same as the veneer, the increased thermal expansion coefficient of the veneering material will increase the tensile stress on veneering material; similarly, a decrease in thermal expansion coefficient of the veneering material will increase compressive stress.19 Aboushelib et al.20 recommended that the difference in thermal expansion coefficients between zirconia and veneer should be as small as possible. At present, many manufacturers of zirconia have developed and sold their own veneering material, which have ideal thermal expansion coefficients for their corresponding zirconia cores. The components and names of these exclusive veneering materials have changed over the years, suggesting that efforts to find an optimal combination are still on-going. Thermal expansion coefficients of several cores and veneering materials are shown in Table 3.
An optimal combination does not merely mean that there is a match in thermal expansion coefficients. Fischer et al.21 reported that the glass transition temperature of the veneering material is also an important factor that influences the shear bond strength of the zirconia and veneering material. Another investigation showed that a slow cooling rate would reduce the possibility of interfacial separation.22
When considering the bond between zirconia-veneering materials, the possibility of chemical bonding must be considered in addition to mechanical bonding based on the difference in thermal expansion coefficients. Guazzato et al.23 found frequent crack extensions at the interface between the veneer and core in strength tests using a veneer-core bilayer. They concluded that strong stress was formed at the interface due to the differences in fracture toughness and moduli of elasticity. Other investigators have shown that the fracture origin and the fracture mode are greatly influenced by the test methodology and by the core thickness/veneer thickness ratio; other factors that determine the origin of fracture include the mechanical properties of the two layers, residual stresses induced by processing, environmental effects, and the properties of the interface.24252627 Another possibility is that crack propagation along the interface is better for stress release than a crack that penetrates the core.19
The fracture behavior of the zirconia-veneer bilayer was evaluated through shear bond strength testing. Cohesive failure of the veneering material itself resulted from the inferior physical properties of the veneering porcelain and the low bond strength between the veneer and zirconia core.27 Taskonak et al.28 reported fracture of the bilayer veneer due to residual stress, and this was reduced by controlling viscoelasticity through slow cooling after heating the core-veneer bilayer to its glass transition temperature. Fracture was observed near the interface between the zirconia and veneer, and some of the veneer layer remained in the zirconia. Some have interpreted this result as evidence for chemical bonding between zirconia and the veneer.29
Fischer et al.30 studied the effects of sandblasting, silica coating, and use of a liner on bond strength between several zirconia and veneering porcelains by measuring the shear bond strength. They showed that the surface treatment increased the surface profile significantly, but no improvement in shear bond strength was observed. Liner applications were the same, and all the fractures showed cohesive failures of the veneer, where the veneer layer remained in the zirconia. Based on these results, the authors concluded that zirconia-veneer bilayer bonding depended upon chemical bonding rather than mechanical bonding since an increase in mechanical roughness did not improve shear bond strength. They further concluded that development of improved veneer reinforcement is needed since cohesive failure of the veneer was the major cause of failure.
On the other hand, Nakamura et al.31 reported that sandblasting at a pressure of 0.4 MPa increased the bond strength between zirconia and colored veneer. However, unlike the tensile bond strength test, shear bond strength tests showed combined failure mixed with adhesive failure.32 However, the origin of the crack propagation was not consistent,33 which makes it difficult to draw concrete conclusions from the shear bond strength tests.
Failure was observed at the interface in microtensile bond strength tests, and this bond seems to be sensitive to the surface treatment and the types of core and veneer used. Aboushelib et al. proved that the interfacial bond strength was material dependent in testing using LAVA and Cercon. Although there was no significant difference in the chemical components of the core, the addition of a yellow coloring pigment showed different results than the standard white block. Furthermore, white blocks that were abraded using airborne particles showed higher bond strength than the milled block; this result was different from the shear bond strength tests conducted by Fischer et al.. On the other hand, airborne particle abraded yellow blocks showed decreased bond strength in both LAVA and Cercon tests, and the type of fracture varied with material and treatment. Interestingly, the use of a liner increased the frequency of interfacial failure in all materials and did not increase bond strength as in the results of Fischer et al.34 However, the same authors' previous experiment showed that liner application increased bond strength between the core and veneer, and failure occurred via complete detachment of the liner layer from the core. In other words, liner performance is very material dependent, especially when it is not compatible with the pressable veneer. Therefore, the liner must be very carefully selected and controlled to achieve the desired effects. Application of various veneers on the same core material (Cercon Base) showed significant differences depending on the kinds of veneering materials (manufacturers) and methods (i.e., layering or pressing) used.35
In previous studies, several testing methods (i.e., shear bond strength, 3-points flexural strength, 4-points flexural strength, and 2-axis flexural strength) were used for measuring core-veneer bond strength, and the values of bond strength depended on the test method employed. Even when using the same method, deviation, fracture mode, and related damage modes varied and depended on variables such as the size of the specimen. Therefore, it is hard to judge certain hypotheses using a single model.
Both core and veneer fractures were found in the Empress II crown; however, the core was intact and delamination of the veneer was the major mode of failure in zirconia crowns.36 Microtensile bond strength testing is difficult to conduct on metal-ceramic and ceramic-ceramic specimens.33 Therefore, tensile strength tests were used in this study, and scratch tests were applied beforehand to determine the optimal etching time. In scratch tests, the bond strength between the zirconia ceramic and porcelain increased as the surface treatment time increased up to 2 hours. However, the bond strength decreased after 3 hours of surface treatment. The increase in bond strength with increasing surface treatment time was attributed to the removal of surface impurities and the high bonding area of zirconia provided by indentations caused by the acid. The decrease in bond strength after 3 hours of surface treatment seems to be due to the decrease in zirconia surface strength itself due to excessive etching. Scratch test results suggested that 2 hours was an adequate etching time. A final experiment was performed to measure the tensile strength in 10 samples each of untreated and 2-hour-ZSAT-treated samples. Within the results of this limited study, the increase in bond strength between zirconia and veneering materials after ZSAT might be attributed to improvement in mechanical bonding due to micro-roughness, and further studies of the effect of low temperature degradation and physical properties are required.
The scratch test results showed that 2 hours of ZSAT provide the highest bond strength between zirconia and veneering materials compared to the 0 hour, 1 hour, and 3 hours treated samples. In tensile strength tests, the ZSAT group treated for 2 hours showed statistically higher tensile bond strength than the non-treated group (36 MPa vs. 30 MPa). In conclusion, ZSAT improves interfacial bond strength between zirconia/veneering materials by increasing the surface roughness of zirconia.
ACKNOWLEDGEMENTS
The authors would like to appreciate Prof. Bum-Sun Lim and Dr. Sung-Nae Cho for their contribution and support to this study.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
1. Piconi C, Maccauro G. Zirconia as a ceramic biomaterial. Biomaterials. 1999; 20:1–25. PMID: 9916767.

2. Chevalier J. What future for zirconia as a biomaterial? Biomaterials. 2006; 27:535–543. PMID: 16143387.

3. Koutayas SO, Vagkopoulou T, Pelekanos S, Koidis P, Strub JR. Zirconia in dentistry: part 2. Evidence-based clinical breakthrough. Eur J Esthet Dent. 2009; 4:348–380. PMID: 20111760.
4. Cho JH, Kim SJ, Shim JS, Lee KW. Effect of zirconia surface treatment using nitric acid-hydrofluoric acid on the shear bond strengths of resin cements. J Adv Prosthodont. 2017; 9:77–84. PMID: 28435615.

5. Su N, Yue L, Liao Y, Liu W, Zhang H, Li X, Wang H, Shen J. The effect of various sandblasting conditions on surface changes of dental zirconia and shear bond strength between zirconia core and indirect composite resin. J Adv Prosthodont. 2015; 7:214–223. PMID: 26140173.

6. Mosharraf R, Rismanchian M, Savabi O, Ashtiani AH. Influence of surface modification techniques on shear bond strength between different zirconia cores and veneering ceramics. J Adv Prosthodont. 2011; 3:221–228. PMID: 22259706.

7. Sailer I, Fehér A, Filser F, Gauckler LJ, Lüthy H, Hämmerle CH. Five-year clinical results of zirconia frameworks for posterior fixed partial dentures. Int J Prosthodont. 2007; 20:383–388. PMID: 17695869.
8. Molin MK, Karlsson SL. Five-year clinical prospective evaluation of zirconia-based Denzir 3-unit FPDs. Int J Prosthodont. 2008; 21:223–227. PMID: 18548960.
9. Sorrentino R, De Simone G, Tetè S, Russo S, Zarone F. Five-year prospective clinical study of posterior three-unit zirconia-based fixed dental prostheses. Clin Oral Investig. 2012; 16:977–985.

10. Ortorp A, Kihl ML, Carlsson GE. A 5-year retrospective study of survival of zirconia single crowns fitted in a private clinical setting. J Dent. 2012; 40:527–530. PMID: 22387979.
11. Vigolo P, Mutinelli S. Evaluation of zirconium-oxide-based ceramic single-unit posterior fixed dental prostheses (FDPs) generated with two CAD/CAM systems compared to porcelain-fused-to-metal single-unit posterior FDPs: a 5-year clinical prospective study. J Prosthodont. 2012; 21:265–269. PMID: 22339945.

12. Raigrodski AJ, Yu A, Chiche GJ, Hochstedler JL, Mancl LA, Mohamed SE. Clinical efficacy of veneered zirconium dioxide-based posterior partial fixed dental prostheses: five-year results. J Prosthet Dent. 2012; 108:214–222. PMID: 23031727.

13. Schmitter M, Mussotter K, Rammelsberg P, Gabbert O, Ohlmann B. Clinical performance of long-span zirconia frameworks for fixed dental prostheses: 5-year results. J Oral Rehabil. 2012; 39:552–557. PMID: 22574689.

14. Sax C, Hämmerle CH, Sailer I. 10-year clinical outcomes of fixed dental prostheses with zirconia frameworks. Int J Comput Dent. 2011; 14:183–202. PMID: 22141229.
15. Al-Amleh B, Lyons K, Swain M. Clinical trials in zirconia: a systematic review. J Oral Rehabil. 2010; 37:641–652. PMID: 20406352.

16. Mackert JR Jr. Effects of thermally induced changes on porcelain-metal compatibility. In : Preston JD, editor. Perspectives in dental ceramics. Proceedings of the fourth international symposium on ceramics. Chicago: Quintessence;1988. p. 53–64.
17. Isgrò G, Pallav P, van der Zel JM, Feilzer AJ. The influence of the veneering porcelain and different surface treatments on the biaxial flexural strength of a heat-pressed ceramic. J Prosthet Dent. 2003; 90:465–473. PMID: 14586311.

18. Murphy KM, Carter JM, Johnson RR, Sorensen SE. Determination of residual stresses in denture base polymers using the layer removal technique. J Biomed Mater Res. 1985; 19:971–980. PMID: 3880354.

19. de Kler M, de Jager N, Meegdes M, van der Zel JM. Influence of thermal expansion mismatch and fatigue loading on phase changes in porcelain veneered Y-TZP zirconia discs. J Oral Rehabil. 2007; 34:841–847. PMID: 17919251.

20. Aboushelib MN, Kleverlaan CJ, Feilzer AJ. Effect of zirconia type on its bond strength with different veneer ceramics. J Prosthodont. 2008; 17:401–408. PMID: 18355163.

21. Fischer J, Stawarzcyk B, Trottmann A, Hämmerle CH. Impact of thermal misfit on shear strength of veneering ceramic/zirconia composites. Dent Mater. 2009; 25:419–423. PMID: 18990436.

22. Göstemeyer G, Jendras M, Dittmer MP, Bach FW, Stiesch M, Kohorst P. Influence of cooling rate on zirconia/veneer interfacial adhesion. Acta Biomater. 2010; 6:4532–4538. PMID: 20601242.

23. Guazzato M, Proos K, Quach L, Swain MV. Strength, reliability and mode of fracture of bilayered porcelain/zirconia (Y-TZP) dental ceramics. Biomaterials. 2004; 25:5045–5052. PMID: 15109867.

24. White SN, Caputo AA, Vidjak FM, Seghi RR. Moduli of rupture of layered dental ceramics. Dent Mater. 1994; 10:52–58. PMID: 7995477.

25. Zeng K, Odén A, Rowcliffe D. Evaluation of mechanical properties of dental ceramic core materials in combination with porcelains. Int J Prosthodont. 1998; 11:183–189. PMID: 9709610.
26. Thompson GA. Influence of relative layer height and testing method on the failure mode and origin in a bilayered dental ceramic composite. Dent Mater. 2000; 16:235–243. PMID: 10831777.

27. Ozkurt Z, Kazazoğlu E. Clinical success of zirconia in dental applications. J Prosthodont. 2010; 19:64–68. PMID: 19754642.
28. Taskonak B, Borges GA, Mecholsky JJ Jr, Anusavice KJ, Moore BK, Yan J. The effects of viscoelastic parameters on residual stress development in a zirconia/glass bilayer dental ceramic. Dent Mater. 2008; 24:1149–1155. PMID: 18329705.

29. Al-Dohan HM, Yaman P, Dennison JB, Razzoog ME, Lang BR. Shear strength of core-veneer interface in bi-layered ceramics. J Prosthet Dent. 2004; 91:349–355. PMID: 15116036.

30. Fischer J, Grohmann P, Stawarczyk B. Effect of zirconia surface treatments on the shear strength of zirconia/veneering ceramic composites. Dent Mater J. 2008; 27:448–454. PMID: 18717175.

31. Nakamura T, Wakabayashi K, Zaima C, Nishida H, Kinuta S, Yatani H. Tensile bond strength between tooth-colored porcelain and sandblasted zirconia framework. J Prosthodont Res. 2009; 53:116–119. PMID: 19345663.

32. Ozkurt Z, Kazazoglu E, Unal A. In vitro evaluation of shear bond strength of veneering ceramics to zirconia. Dent Mater J. 2010; 29:138–146. PMID: 20379023.
33. Anusavice KJ, Kakar K, Ferree N. Which mechanical and physical testing methods are relevant for predicting the clinical performance of ceramic-based dental prostheses? Clin Oral Implants Res. 2007; 18:218–231. PMID: 17594384.

34. Fischer J, Grohmann P, Stawarczyk B. Effect of zirconia surface treatments on the shear strength of zirconia/veneering ceramic composites. Dent Mater J. 2008; 27:448–454. PMID: 18717175.

35. Aboushelib MN, Kleverlaan CJ, Feilzer AJ. Microtensile bond strength of different components of core veneered all-ceramic restorations. Part II: Zirconia veneering ceramics. Dent Mater. 2006; 22:857–863. PMID: 16376981.
36. Sundh A, Sjögren G. A comparison of fracture strength of yttrium-oxide-partially-stabilized zirconia ceramic crowns with varying core thickness, shapes and veneer ceramics. J Oral Rehabil. 2004; 31:682–688. PMID: 15210030.
Fig. 1
(A) Push-pull tension gauge 5005, (B) Specimen loaded for tensile strength test (See the line of bonded interface between two zirconia blocks).
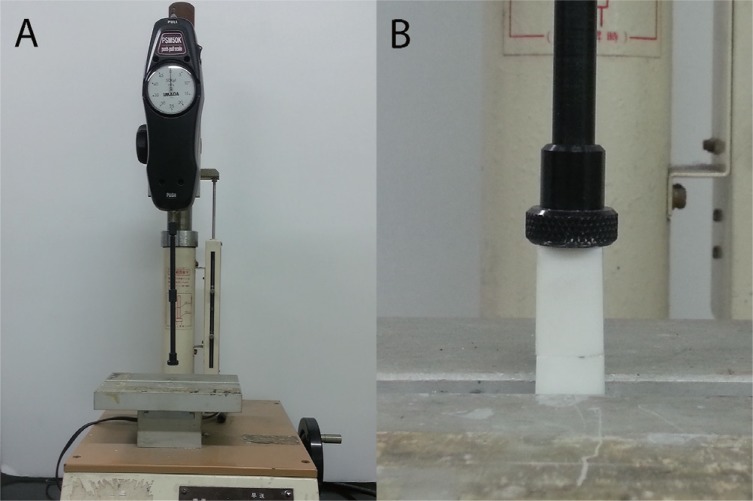
Fig. 2
(A) Zirconia surface before surface treatment, (B) Zirconia surface after surface treatment for 1 hour, (C) Zirconia surface after surface treatment for 2 hours, (D) Zirconia surface after surface treatment for 3 hours.
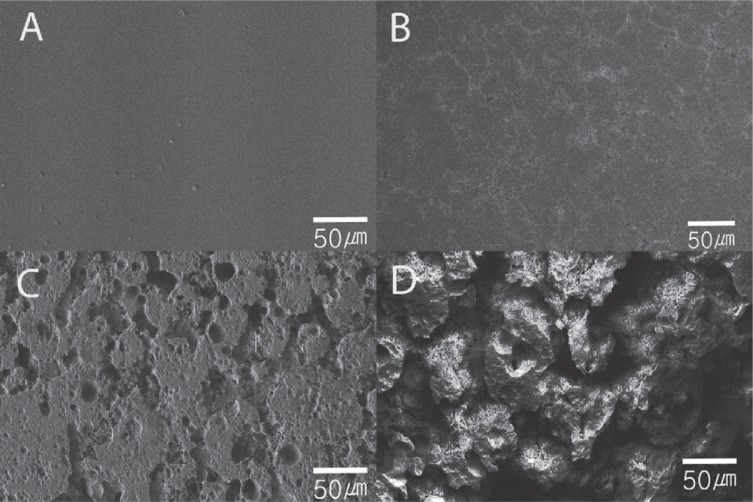
Table 1
Mean adhesive strength (in MPa) and standard deviation as a function of treatment time
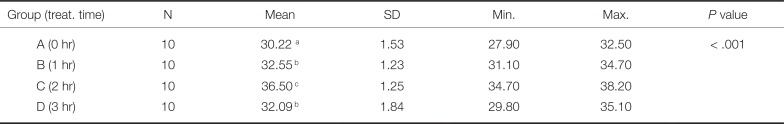
Table 2
Comparative mean tensile strength (in MPa) based on surface etching status
| N | Mean | SD | P value | |
|---|---|---|---|---|
| No etching | 30 | 30.05 | 0.32 | < .001 |
| Etching | 30 | 36.21 | 0.33 |
Table 3
Thermal expansion coefficients of several cores and veneering materials




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download