Abstract
Purpose
We report a case of a young female patient who was diagnosed with a marginal zone B-cell lymphoma of the mucosa-associated lymphoid tissue (MALT lymphoma) of the lacrimal sac which mimicked dacrocystitis.
Case summary
A 23-year-old female suffered from epiphora for 3 years in the right eye. She had swelling and a painful lesion at the lacrimal sac 4 months prior and was referred to our hospital due to nasolacrimal duct obstruction and dacryocystitis. Lacrimal irrigation was performed with no passing and regurgitation with mucoid discharge. We performed orbital computed tomography and magnetic resonance imaging which showed a suspected tumor of the lacrimal sac in the right eye. We then performed excision and biopsy of the tumor through the skin approach. The patient was diagnosed with a MALT lymphoma with no systemic involvement. After six cycles of chemotherapy involving rituximab with cyclophosphamide, vincristine, and prednisone, the lesion of the mass and the painful symptoms decreased, which was regarded as a complete response. However, epiphora and eye discharge persisted, showing a nasolacrimal duct obstruction, so we performed endoscopic dacryocystorhinostomy with a lacrimal sac biopsy. The histological examination showed chronic inflammation, but not lymphoma. There was no recurrence of lymphoma at one year postoperatively.
Figures and Tables
Figure 1
External photograph of 23-year-old female patient. The patient had epiphora and mild swelling at right lacrimal sac area.

Figure 2
Orbit computed tomography scan. (A) Non-enhance axial computed tomography images show ill-defined hyperdense mass (black arrow) at right lacrimal sac. (B) Expansion of nasolacrimal duct (white arrow).

Figure 3
Orbit magnetic resonance imaging. (A) Axial T2 weighted image shows homogeneous relatively hyper-intensity in right lacrimal sac (white arrowhead). (B) Contrast-enhanced axial T1 weighted image demonstrates iso signal intensity tubular structure with rim enhancement in the right lacrimal sac (white arrow). (C) Axial T2 weighted image after systemic chemotheraphy showed no mass leision in lacrimal sac. (D) Contrast-enhanced axial T1 weighted image after systemic chemotheraphy showed no enhancing mass leision.
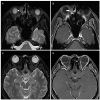
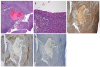
Figure 4
Histopathologic findings of the surgical specimen. (A) Dense, monotonous neoplastic lymphoid cells surround the lacrimal sac (hematoxylin & eosin stain [H&E], ×40). (B) Lymphoepithelial lesions are identified (H&E ×400). (C) CD20 staining positivity demonstrates extensive B cell infiltration (CD20, ×40). (D) Lymphoid cells showing cystoplasmic kappa light chain positivity (kappa in situ hybridization, ×40). (E) A few lymphoid cells showing cystoplasmic lambda light chain positivity (lambda in situ hybridization, ×40). Kappa light chain predominates over lambda chain, demonstrating monoclonality.
References
2. Bartley GB. Acquired lacrimal drainage obstruction: an etiologic classification system, case reports, and a review of the literature. Part 1. Ophthalmic Plast Reconstr Surg. 1992; 8:237–242.
3. Nakamura K, Uehara S, Omagari J, et al. Primary non-Hodgkin lymphoma of the lacrimal sac: a case report and review of the literature. Cancer. 1997; 80:2151–2155.
4. Erickson BA, Massaro BM, Mark LP, Harris GJ. Lacrimal collecting system lymphomas: integration of magnetic resonance imaging and therapeutic irradiation. Int J Radiat Oncol Biol Phys. 1994; 29:1095–1103.

5. Knowles DM 2nd, Jakobiec FA. Ocular adnexal lymphoid neoplasms: clinical, histopathologic, electron microscopic, and immunologic characteristics. Hum Pathol. 1982; 13:148–162.

6. Park SJ, Lee WS, Yang JW. The effect of rituximab, cyclophosphamide, vincristine, and prednisolone (R-CVP) chemotherapy in patients with ocular adnexal extranodal marginal zone B cell lymphoma of the mucosa-associated lymphoid tissue (MALT) lymphoma. Korean J Ophthalmol Soc. 2013; 54:1157–1164.

7. Sjö LD, Ralfkiaer E, Juhl BR, et al. Primary lymphoma of the lacrimal sac: an EORTC ophthalmic oncology task force study. Br J Ophthalmol. 2006; 90:1004–1009.

8. Kitaguchi Y, Takahashi Y, Mupas-Uy J, et al. Primary marginal zone B-cell lymphoma of the mucosa-associated lymphoid tissue of the lacrimal sac found with epiphora: a case report. Case Rep Ophthalmol. 2016; 7:148–154. eCollection 2016 Sep-Dec.

9. Maharajah KR, Hussein A, Mohamad H, et al. Primary non-Hodgkins lymphoma of the lacrimal sac: mortality-related epiphora. Orbit. 2009; 28:306–308.

10. Schefler AC, Shields CL, Shields JA, et al. Lacrimal sac lymphoma in a child. Arch Ophthalmol. 2003; 121:1330–1333.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download