Abstract
Purpose
To evaluate the incidence and risk factors for ocular hypertension (OHT) in traumatic hyphema within 7 days after trauma.
Methods
A retrospective case series study of 265 traumatic hyphema inpatients from 2010–2016. OHT was defined as intraocular pressure (IOP) that exceeded 21 mmHg using two consecutive measurements by a Goldmann applanation tonometer within 7 days after trauma. The subjects were divided into two groups (OHT group and non-OHT group). Age, sex, best-corrected visual acuity (BCVA), IOP, hyphema grade, presence of systemic disease, and past history of glaucoma were compared between the two groups.
Results
Of the 265 patients, 95 (35.8%) developed OHT after traumatic hyphema. Of those 95 patients, 70 (73.7%) developed OHT within 1 day after trauma; 18 (18.9%) developed OHT 2–3 days after trauma; and 7 (7.4%) developed OHT 4–7 days after trauma. Compared to the non-OHT group, the OHT group had a lower visual acuity (p = 0.018) and higher IOP (p < 0.001). In addition. if the hyphema grade was higher the incidence of OHT was significantly higher (p = 0.017). Using multivariate logistic regression analysis, the BCVA (p = 0.045) and hyphema grade (p = 0.006) were associated with the incidence of OHT in traumatic hyphema within 7 days after trauma.
Figures and Tables
Figure 1
Incidence of ocular hypertension during hospitalization in traumatic hyphema. 73.7% developed ocular hypertension within 1 day after trauma, 18.9% developed between 2–3 days, and 7.4% developed between 4–7 days.
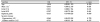
Table 2
Comparison between ocular hypertension (OHT) group and non-OHT group

Values are presented as the mean ± standard deviation or n (%) unless otherwise indicated.
V/A = visual acuity; IOP = intraocular pressure.
*Pearson chi-square test. Statistical significance: p < 0.005; †Student t-test. Statistical significance: p < 0.005; ‡Linear-by-Linear assosiation. Statistical significance: p < 0.005.
References
1. Ghafari AB, Siamian H, Aligolbandi K, Vahedi M. Hyphema caused by trauma. Med Arch. 2013; 67:354–356.

2. Arentsen JJ, Green WR. Melanoma of the iris: report of 72 cases treated surgically. Ophthalmic Surg. 1975; 6:23–37.
3. Blanksma LJ, Hooijmans JM. Vascular tufts of the pupillary border causing a spontaneous hyphaema. Ophthalmologica. 1979; 178:297–302.

4. Kurz GH, Zimmerman LE. Spontaneous hyphema and acute glaucoma as initial signs of recurrent iris melanoma. Arch Ophthalmol. 1963; 69:581–582.

5. Türkcü FM, Yüksel H, Sahin A, et al. Demographic and etiological characteristics of children with traumatic serious hyphema. Ulus Travma Acil Cerrahi Derg. 2013; 19:357–362.
6. Crouch ER, Williams PB. Trauma: ruptures and bleeding. In : Tasmani W, Jager EM, editors. Duane's Clinical Ophthalmology. 1st ed. Philadelphia: Lippincott Williams & Wilkins;1993. p. 1–18.
7. Coles WH. Traumatic hyphema: an analysis of 235 cases. South Med J. 1968; 61:813–816.
8. Fong LP. Secondary hemorrhage in traumatic hyphema. Predictive factors for selective prophylaxis. Ophthalmology. 1994; 101:1583–1588.
10. Read J, Goldberg MF. Comparison of medical treatment for traumatic hyphema. Trans Am Acad Ophthalmol Otolaryngol. 1974; 78:799.
11. Turalba AV, Shah AS, Andreoli MT, et al. Predictors and outcomes of ocular hypertension after open-globe injury. J Glaucoma. 2014; 23:5–10.

12. Bojikian KD, Stein AL, Slabaugh MA, Chen PP. Incidence and risk factors for traumatic intraocular pressure elevation and traumatic glaucoma after open-globe injury. Eye (Lond). 2015; 29:1579–1584.

13. Sihota R, Kumar S, Gupta V, et al. Early predictors of traumatic glaucoma after closed globe injury: trabecular pigmentation, widened angle recess, and higher baseline intraocular pressure. Arch Ophthalmol. 2008; 126:921–926.
14. Bansal S, Gunasekeran DV, Ang B, et al. Controversies in the pathophysiology and management of hyphema. Surv Ophthalmol. 2016; 61:297–308.
15. Roth DB, Verma V, Realini T, et al. Long-term incidence and timing of intraocular hypertension after intravitreal triamcinolone acetonide injection. Ophthalmology. 2009; 116:455–460.

18. Girkin CA, McGwin G Jr, Long C, et al. Glaucoma after ocular contusion: a cohort study of the United States Eye Injury Registry. J Glaucoma. 2005; 14:470–473.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download