This article has been
cited by other articles in ScienceCentral.
Abstract
Objectives
This study aimed to investigate the prevalence of a separate distolingual root and to measure the thickness of the buccal cortical bone in mandibular first molars in Koreans using cone-beam computed tomography (CBCT) images.
Materials and Methods
High-quality CBCT data from 432 patients were analyzed in this study. The prevalence of a separate distolingual root of the mandibular first molar was investigated. The distance from the distobuccal and distolingual root apices to the outer surface of the buccal cortical bone was measured. We also evaluated the thickness of the buccal cortical bone.
Results
The prevalence of a separate distolingual root (2 separate distal roots with 1 canal in each root; 2R2C) was 23.26%. In mandibular first molars with 2R2C, the distance from the distobuccal root apex to the outer surface of the buccal cortical bone was 5.51 mm. Furthermore, the distance from the distolingual root apex to the outer surface of the buccal cortical bone was 12.09 mm. In mandibular first molars with 2R2C morphology, the thickness of the buccal cortical bone at the distobuccal root apex of the mandibular first molar was 3.30 mm. The buccal cortical bone at the distobuccal root apex was significantly thicker in the right side (3.38 mm) than the left side (3.09 mm) (p < 0.05).
Conclusions
A separate distolingual root is not rare in mandibular first molars in the Korean population. Anatomic and morphologic knowledge of the mandibular first molar can be useful in treatment planning, including surgical endodontic treatment.
Keywords: Cone-beam computed tomography, Cortical bone, Korean, Mandibular, Root
INTRODUCTION
Together with diagnosis and treatment planning, the knowledge of common root canal morphology is a basic requirement for the success of endodontic procedures. In addition, recognizing variations in root morphology is essential for dental procedures such as root canal treatment and surgical endodontic treatment. Permanent mandibular first molars usually have 2 roots, but occasionally have 3 roots. Although the presence of 2 separate distal roots is rare, in Asian populations, literature reviews have reported a high prevalence of 3-rooted mandibular first molars, ranging from 5% to more than 40% [
12345].
Nonsurgical endodontic treatment gives good results in most cases. However, surgical endodontic treatment, including apicoectomy and intentional replantation, may be indicated for teeth with persistent periradicular pathosis that have not responded to non-surgical approaches. More specifically, surgical approaches to the mandibular first molars are difficult due to their complex root morphology, shallow vestibule, and thick buccal cortical bone [
67].
In routine diagnostic periapical radiography, the central ray is placed perpendicular to the mandibular first molar and the film. Therefore, the image of the distolingual (DL) root can easily be superimposed on the distobuccal (DB) root, blurring the picture [
8]. As a form of noninvasive imaging involving 3-dimensional reconstruction, cone-beam computed tomography (CBCT) can be used to evaluate the morphology of the DL root of mandibular first molars. In addition, anatomic studies using CBCT can provide guidance for accessing the surgical site [
91011].
This study aimed to investigate the morphology and prevalence of a separate DL root and to measure the thickness of the buccal cortical bone of mandibular first molars in Koreans using CBCT images.
MATERIALS AND METHODS
The research protocol of this study was approved by the Institutional Review Board of the Chosun University Dental Hospital of Korea (CUDHIRB-1606-030). For the morphological analysis of mandibular first molars, CBCT images that had been taken from July 2012 to June 2013 at Chosun University Dental Hospital (Gwangju, Korea) for third molar extraction were screened and examined.
Fully erupted and completely root-formed mandibular first molars with no history of root canal treatment were selected. High-quality CBCT data from 432 patients (209 females and 223 males) were selected. The patients were aged from 11 to 62 years old, with the mean age of 24. Finally, a total of 864 mandibular first molars were examined retrospectively.
The CBCT images were taken using CB Mercuray (Hitachi Medical Corp., Tokyo, Japan) and the scan settings were a Ø10 cm scan field of view, 0.2 mm voxel size, 120 kVp, 15 mA, and a 10-second exposure time. The tomography sections were displayed using OnDemand3D software (Cybermed Inc., Seoul, Korea) in the axial, coronal, and sagittal planes. To ensure optimal visualization, the contrast and brightness of the images could be adjusted using the image processing tool of the software. The long axis of each mandibular first molar was determined, and cross-sectional images at the apical third of the root were examined by rolling the tool bar from the pulp chamber to the apex of the tooth. The type of distal root canal morphology and the prevalence of a separate DL root of the mandibular first molars were investigated through these procedures (
Figure 1). For a precise investigation of the distance from the root apices to the outer surface of the buccal cortical bone of mandibular first molars with 2 separate distal roots with 1 canal in each root (2R2C), fine adjustments were made on the CBCT images using OnDemand3D software.
Figure 1
Representative cone-beam computed tomography images. (A) Mandibular first molar with the morphology of 2 separate distal roots with 1 canal in each root (blue circle); (B) Mandibular first molar with the morphology of 1 distal root with 2 separate canals (blue circle).

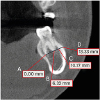
To investigate the distal root anatomy, in the axial view, the intersecting point was moved to the DL root of each mandibular first molar with 2R2C morphology. Then, in the axial and sagittal views, the coronal plane was set parallel to the 2 long axes of the DL and DB roots of the mandibular first molars with 2R2C morphology. In the coronal view, a horizontal line passing through the 2 points of the DL and DB root apices was drawn. The line was extended to the buccal cortical bone. On the coronal plane of the CBCT images, 4 points that intersected with the horizontal line were set and marked as A, B, C, and D, corresponding to the DL root apex, the DB root apex, the inner surface of the buccal cortical bone, and the outer surface of the buccal cortical bone, respectively (
Figure 2).
Figure 2
Representative measurements on the coronal plane of a cone-beam computed tomography image. Four points that intersected with the horizontal line crossing the apex of DB and DL root in a mandibular first molar with the morphology of 2 separate distal roots with 1 canal in each root were set up, as follows: (A) DL root apex; (B) DB root apex; (C) inner surface of the buccal cortical bone; (D) outer surface of the buccal cortical bone. The measurements at 4 points are the distances from point A.
DB, distobuccal; DL, distolingual.
The distance from the DL root apex to the outer surface of the buccal cortical bone (i.e., the distance between A and D) was measured, after which the distance was measured from the DB root apex to the outer surface of the buccal cortical bone (i.e., the distance between B and D). The thickness of the buccal cortical bone (i.e., the distance between C and D) was also measured.
As shown by our results, adjusting the CBCT scans so that the coronal plane ran through the mandibular first molars ensured precise measurements. The gender ratio, bilateral and unilateral occurrence, and the difference in the distances between right and left mandibular first molars were also analyzed. The difference between right and left mandibular first molars was statistically evaluated using the t test using SPSS software (version 12.0, SPSS Inc., Chicago, IL, USA). All statistical inferences were made within a 95% confidence interval (p < 0.05).
RESULTS
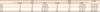
A total of 864 mandibular first molars from 432 patients were evaluated. The total prevalence of a separate DL root (2R2C) was 23.26%. The prevalence of 2R2C morphology was 19.90% on the left side and 26.62% on the right side. Furthermore, the total prevalence of mandibular first molars with 1 distal root with 2 separate canals (1R2C) was 25.69%. The prevalence of 1R2C morphology was 26.85% on the left side and 24.53% on the right side (
Table 1).
Table 1
Prevalence (%) of 2R2C and 1R2C morphology in the distal root of mandibular first molars
|
Left |
Right |
Overall |
|
Female |
Male |
Total |
Female |
Male |
Total |
|
2R2C |
37 |
49 |
86 (19.91) |
55 |
60 |
115 (26.62) |
201 (23.26) |
|
1R2C |
51 |
65 |
116 (26.85) |
49 |
57 |
106 (24.54) |
222 (25.69) |
|
1R1C |
121 |
109 |
230 (53.24) |
105 |
106 |
211 (48.84) |
441 (51.04) |
|
Total |
209 |
223 |
432 (100) |
209 |
223 |
432 (100) |
864 (100) |
Among the patients, 18.75% had concurrent bilateral 2R2C morphology. Furthermore, 5 patients (all females) had unilateral 2R2C morphology on the left side and 34 patients (14 females, 20 males) had unilateral 2R2C morphology on the right side (
Table 2).
Table 2
Unilateral and bilateral 2R2C morphology in mandibular first molars among Korean patients

|
Unilateral left |
Unilateral right |
Bilateral |
|
Female |
Male |
Total |
Female |
Male |
Total |
Female |
Male |
Total |
|
2R2C |
5 |
0 |
5 |
14 |
20 |
34 |
32 |
49 |
81 (18.75) |
In the mandibular first molars with 2R2C, the right mandibular first molar showed a significantly longer distance from DL root apex to the outer surface of buccal cortical bone (12.48 mm) than that of the left mandibular first molar (11.57 mm) (
p < 0.05). However, there was no statistically significant difference between the right side (5.70 mm) and the left side (5.27 mm) of the distance from DB root apex to outer surface of buccal cortical bone (
Table 3).
Table 3
The distance (mm) from the DB and DL root apices to the outer surface of the buccal cortical bone in mandibular first molars with 2R2C morphology

|
DB root to buccal bone |
DL root to buccal bone |
|
Left |
Right |
Total |
Left |
Right |
Total |
|
2R2C |
5.27 ± 1.73a
|
5.70 ± 2.01a
|
5.51 ± 1.90B
|
11.57 ± 2.07b
|
12.48 ± 2.38a
|
12.09 ± 2.29A
|
In the mandibular first molars with 2R2C morphology, the thickness of the buccal cortical bone at the DB root apex (distance from point C to point D) was significantly thicker in the right mandibular first molars (3.38 mm) than the left ones (3.09 mm) (
p < 0.05;
Table 4).
Table 4
Thickness (mm) of the buccal cortical bone in mandibular first molars with 2R2C morphology

|
Buccal cortical bone thickness |
|
Left |
Right |
Total |
|
2R2C |
3.09 ± 1.08b
|
3.38 ± 1.09a
|
3.30 ± 1.09 |
DISCUSSION
As the earliest permanent posterior teeth to erupt, the mandibular first molars frequently require dental therapy such as caries control, root canal treatment, and surgical endodontic treatment [
6]. They are often extensively restored and are subjected to heavy occlusal stress. Therefore, the pulp chamber frequently recedes or is calcified. The complex root anatomy of mandibular first molars makes it difficult to perform root canal treatment. Therefore, it is essential that dental clinicians be familiar with the anatomic complexity of mandibular first molars.
Mandibular first molars usually have 2 roots, located mesially and distally. However, as reported in numerous studies, a DL root is considered to be a normal morphologic variant of mandibular first molars in Asian populations [
12312]. In the present study, we found that 23.26% of mandibular first molars had 2R2C morphology. In addition, 25.69% of mandibular first molars had 1R2C morphology. Therefore, the results of the present study are consistent with previous researches. The topological predilection for the presence of a DL root in mandibular first molars is a controversial issue. Many studies have found right-side predominance [
13131415]. In contrast, some investigators have reported a predilection for the left side [
1617]. The results of the present study support the former tendency.
As suggested by our results, the prevalence of bilateral appearance of a DL root was 18.75%, which aligns with previously reported findings (18.38%, 17.64%) [
1819]. If the prevalence was calculated using 3-rooted molars as the common denominator, the proportion of bilateral DL roots increased to 80.59%. This is higher than the corresponding values that have been reported for patients in Taiwan (68.60%), Hong Kong (61.00%), and Korea (77.31%) [
31519]. The diversity in the outcomes of the previously mentioned studies might result from differences in methods, sample sizes, and subject inclusion criteria.
After conventional root canal treatment, a periapical lesion may occur in the DL root of mandibular first molars. In such cases, clinicians consider 3 kinds of treatment plans: re-treatment, apicoectomy, and intentional replantation. In an ideal situation, re-treatment is successful. However, when re-treatment fails or cannot be performed, surgical endodontic treatment, such as apicoectomy and intentional replantation, can be an option. When surgical endodontic treatment is planned, clinicians should carefully consider anatomic factors and variations. Evaluating the access to the surgical site is the most important step when opting for surgical endodontic treatment. Whereas the mesial root of the mandibular first molar appears close to the buccal cortical plate, the distal root is centrally located in the bone, and the roots of the second molar are significantly closer to the lingual cortical plate [
1920]. For that reason, access to the distal root is more difficult than access to the mesial root in surgical approaches to the mandibular first molar. According to our results, the presence of a DL root complicated surgical access. Therefore, to improve diagnosis and surgery, clinicians take CBCT images before surgical endodontic treatment. The results of this study will be helpful for estimating the anatomical distances of mandibular first molars in Koreans.
According to the results of a previous study using CBCT images with a voxel size of 0.4 mm, the distance from the DL canal to the buccal cortical bone was significantly different in 2R2C and 1R2C teeth [
19]. Specifically, in 2R2C teeth, the distance was longer than in 1R2C teeth. In contrast, the distance from the DB canal to the buccal cortical bone in 2R2C teeth was shorter than in 1R2C teeth. This means that access to the DL canal in 2R2C teeth is more difficult than in 1R2C teeth during apicoectomy, while access to the DB canal in 2R2C teeth is easier than in 1R2C teeth.
The present study was conducted based on CBCT data with better resolution than those used in the previous study due to a smaller voxel size (0.2 mm). Improved resolution has a strong impact on the accuracy of radiographic investigations. In addition, fine adjustment of CBCT images using the OnDemand3D software enabled us to more precisely measure anatomical distances.
In the present study, the tooth anatomy was compared between the right and left mandibular first molars with 2R2C morphology. The distance from the DL root apex to the outer surface of the buccal cortical bone and the buccal cortical bone thickness at the distal root apex showed a statistically significant difference between the right and left sides. In the future, it will be necessary to investigate the relationship between the anatomy of mandibular first molars and the mastication involved in unilateral chewing.
In surgical endodontic treatment of a mandibular first molar with a DL root, the distance between the outer surface of the buccal cortical bone and the DL root apex is important. The long distance makes it difficult to visualize and access the operating site of the DL root apex. In the present study, the distance from the outer surface of the buccal cortical bone to the DL root apex showed a statistically significant difference between the left (11.57 mm) and right (12.48 mm) sides. Furthermore, the thickness of the buccal cortical bone at the distal root apex in the mandibular first molars with 2R2C morphology, which must be removed for surgical endodontic treatment, showed a statistically significant difference between the left (3.09 mm) and right (3.38 mm) sides. According to these results of the present study, when apicoectomy of a DL root in a mandibular first molar with 2R2C morphology on the right side is performed, more time and concentration is required to make a bony window in the thick buccal cortical bone. During the process, heat generation should be minimized to preserve healthy hard tissue [
2122]. In addition, the long distance from the outer surface of the buccal cortical bone to the DL root apex makes it difficult to see the DL root apex. Therefore, for good visualization, clinicians may need a larger bony window for mandibular first molars with 2R2C morphology than for the other teeth.
With proper case selection, morphologic knowledge, and operating skill, surgical endodontic treatment for mandibular first molars with persistent periradicular disease at a separate DL root after nonsurgical re-treatment can be considered a predictable, cost-effective alternative to extraction and tooth replacement. Anatomic and morphologic knowledge of the mandibular first molar, such as the presence of a DL root, buccal cortical bone thickness, and the distance from the DL root apex to the outer surface of the buccal cortical bone, can be useful for treatment planning, including surgical endodontic treatment. Therefore, CBCT images should be considered when more information for diagnosis and treatment planning of a mandibular first molar is needed, before not only conventional root canal treatment, but also surgical endodontic microsurgery.
CONCLUSIONS
The prevalence of a separate distolingual root (2 separate distal roots with 1 canal in each root; 2R2C) was 23.26% in a Korean population. In mandibular first molars with 2R2C morphology, the mean distance from the distolingual root apex to the outer surface of the buccal cortical bone was 12.09 mm, and the buccal cortical bone at the distobuccal root apex was significantly thicker in the right side (3.38 mm) than the left side (3.09 mm). Anatomic and morphologic knowledge of the mandibular first molar can be useful in treatment planning, including surgical endodontic treatment.







 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download