Abstract
Purpose
To evaluate the prevalence of anterior type diabetic retinopathy (DR) using ultra-widefield fluorescein angiography and to identify the factors associated with anterior type DR incidence.
Methods
A retrospective case review was used in this study. Patients with non-proliferative diabetic retinopathy (NPDR) underwent examination by ultra-widefield fluorescein angiography, and were classified into anterior, posterior, or diffuse DR groups. Anterior DR was defined if diabetic retinal changes were noted only at the location anterior to the imaginary circle bordered by the Early Treatment Diabetic Retinopathy Study seven-standard fields. Correlations between demographic data, as well as systemic and ocular factors, and the incidence of NPDR types were evaluated.
Results
Among the 234 eyes of 234 patients with NPDR, 25 eyes (10.7%) demonstrated anterior DR. Anterior DR was observed in 10 eyes (30.3%) of patients having mild NPDR, three eyes (4.8%) of moderate NPDR patients, and in 12 eyes (7.1%) of severe NPDR patients (p < 0.001). The incidence of anterior DR positively correlated with lower hemoglobin A1c levels and with greater high-density lipoprotein levels following multiple logistic regression analysis (p < 0.001). The mean hemoglobin A1c level was 7.03 ± 0.99% in anterior DR, 7.99 ± 1.74% in posterior DR, and 7.94 ± 1.39% in diffuse DR patients (p = 0.003). The mean high-density lipoprotein level was 51.2 ± 12.5 mg/dL in anterior, 49.7 ± 15.2 mg/dL in posterior, and 45.2 ± 13.1 mg/dL in diffuse DR patients (p = 0.010).
As the prevalence of diabetes increases, diabetic retinopathy (DR) has become one of the most prominent diabetic complications and has increased the morbidity and social costs related to the disease. Currently, the results of the Diabetic Retinopathy Study, an epochal study that began in 1971, have guided much of the management of DR patients [1].
Over the past 30 years, improvements in retinal imaging technology have led to the emergence of diagnostic imaging as a key investigative tool that continues to play a vital role in DR management. Under optimal conditions, traditional fluorescein angiography provides a view of up to 40 degrees of the retina with a single image. The seven standard fields protocol, proposed by the Early Treatment Diabetic Retinopathy Study (ETDRS), allows for an approximately 75-degree view of the fundus [1]. However, the fields are limited in their capabilities for providing angiographic information on the remaining peripheral retina. Recent developments in scanning laser ophthalmoscope technology allow for consistently reproducible high-resolution angiographic images of the peripheral retina. For example, ultra-widefield fluorescein angiography (UWFA) provides visualization of up to 200 degrees [2], and enables pan-retinal angiographic assessment of retinal vascular perfusion without having to make image montages, which are obtained by combining multiple non-simultaneous angiographic views [3]. Several previous studies have evaluated peripheral retinal pathology in DR using UWFA. Wessel et al. [4] reported that, compared with conventional seven-standard field imaging, UWFA identified significantly more retinal vascular pathology in DR patients. Patel et al. [3] demonstrated the association between peripheral retinal capillary non-perfusion and recalcitrant diabetic macular edema (DME). Following the introduction of UWFA, it has become feasible to identify diabetic microvascular changes appearing only in the peripheral retina, that is, anterior DR. Thus, improved visualization of the peripheral retina could alter the classification of DR and enable the refinement of follow-up and treatment protocols for diabetic patients. However, there has been no study to address the clinical significance of these anterior lesions in DR. The aim of the current study is to establish the anterior type DR as a new entity and to identify the factors related to anterior DR incidence.
We conducted a retrospective review of all patients with DR diagnosed at the Department of Ophthalmology, Samsung Medical Center, over a 1-year period (April 2012 to May 2013). Ethics approval was obtained from the Samsung Medical Center institutional review board (no. 2013-06-114). Patient care was in accordance with the Declaration of Helsinki.
All diabetic patients with a diagnosis of non-proliferative diabetic retinopathy (NPDR) based on funduscopic examination, and who underwent UWFA (Optomap P200MA; Optos, Dunfermline, UK) were included in this study. Patients with non-diabetic retinal pathology, including vessel occlusions, uveitis, infective retinopathy, choroidal tumor, and/or significant media opacity (vitreous hemorrhage, cataract) that precluded accurate evaluation of the angiogram, were excluded.
One experienced physician (SWK) performed fundus examination in all patients and determined NPDR stage according to the diagnostic criteria of the ETDRS.
UWFA images were obtained according to standard protocol. Angiography was performed after intravenous injection of 5 mL of 10% sodium fluorescein. One representative image showing the arteriovenous filling phase was chosen for each eye. Images were digitally captured and subsequently compressed into high-quality JPEG (Joint Photographic coding Experts Group) files.
Using the protocol for seven-standard field images, as described by the ETDRS [1], 30-degree circles were combined to create a digital seven-standard field template. This template was then laid over the UWFA image to identify the potential viewable area of the seven-standard fields, and an overlaying circle with a radius equal to the distance between the optic nerve head and the outermost point from the optic nerve head was drawn to include the entire seven-standard field area (Fig. 1). The resulting overlaid circle was regarded as a boundary line for the classification of anterior or posterior DR types.
One reader (THK) who was blinded to the study results analyzed each image for the presence of the three distinct DR types: anterior, posterior, and diffuse. In the UWFA images, diabetic intraretinal microvascular changes including retinal were noted in both sides of the overlaying circle, and a diffuse DR classification was assigned. Examples of each NPDR type, based on UWFA finding, are shown in Fig. 2A-2C. Using fundus and UWFA images, all NPDR patients were classified according to NPDR type. In this study, the original definition of DR staging from ETDRS research was cited.
Follow-up funduscopic examination was performed at 3- to 6-month intervals, according to NPDR stage. Data on hemorrhage, retinal non-perfusion or capillary dropout, microaneurysm, intraretinal microvascular abnormality, and venous beading were noted. If retinal changes were located only outside the overlaying circle, anterior DR was assigned. Conversely, when microvascular changes were found within the overlaying circle, posterior type DR was assigned. Several patient parameters were collected: diabetic retinal changes gender, age, duration of diabetes, best-corrected visual acuity, fasting glucose level, total cholesterol, blood urine nitrogen, creatinine, glomerular filtration rate, triglyceride, high-density lipoprotein-cholesterol (HDL-C), low-density lipoprotein-cholesterol (LDL-C), and percentage hemoglobin A1c (HbA1c). A urine test, including evaluation of proteinuria, albuminuria, and urine albumin to creatinine ratio was also performed. Data on insulin use, oral medication for glucose control, lipid-lowering agents including statins and fenofibrate, history of ocular infection and surgery, and other ocular pathology were obtained. The presence of diabetic nephropathy and the relationship between diabetic nephropathy and DR type were also analyzed. Diabetic nephropathy in this study was characterized by macroalbuminuria (defined as urinary albumin to creatinine ratio >300 or urinary albumin excretion >0.5 g/day) or decreased glomerular filtration rate (<60 mL/min/m2) [5]. The presence of DME was assessed using spectral-domain optical coherence tomography (Spectralis HRA-OCT; Heidelberg Engineering, Heidelberg, Germany). DME was defined as a central macular thickness larger than 300 µm.
Statistical analyses were performed using Pearson's chi-square test and an ANOVA test with linear regression (SPSS ver. 20.0; IBM Co., Armonk, NY, USA). A p-value less than 0.05 was considered significant. Multiple logistic regression analyses were conducted for each participant.
Two hundred and thirty-four eyes of 234 individuals with NPDR were included in this study (151 men and 83 women). Only one eye from each individual was randomly selected for analysis. All participants were Korean, with a mean age of 63.0 ± 19.7 years (range, 20 to 90 years). The mean logarithm of the minimum angle of resolution best corrected visual acuity was 0.10 ± 0.13 in anterior type DR, 0.08 ± 0.13 in posterior type DR, and 0.10 ± 0.13 in diffuse type DR. None of the patients included in the study had a history of vitreoretinal surgery or pan-retinal photocoagulation. Among the eyes studied, mild NPDR was noted in 33 eyes (14.1%), moderate NPDR in 62 eyes (26.5%), and severe NPDR in 139 eyes (59.4%) (Fig. 3A-3D). Regarding the DR types, 25 eyes (10.7%) were classified as the anterior type, 90 eyes (38.5%) as the posterior type, and 119 eyes (50.8%) as the diffuse type. Mean duration of diabetes was 18.7 years in anterior DR, 16.3 years in posterior DR, and 17.4 years in diffuse DR. The patient demographic characteristics are summarized in Table 1. Among eyes with mild NPDR, 10 (30.3%) were of the anterior type, eight (24.2%) were of the diffuse type, and 15 (45.5%) were of the posterior type. Among eyes with moderate NPDR, three (4.8%) were of the anterior type, 33 (53.2%) were of the diffuse type, and 26 (42%) were of the posterior type. Among eyes with severe NPDR, 12 (7.1%) were of the anterior type, 78 (46.2%) were of the diffuse type, and 49 (46.7%) were of the posterior type (Fig. 4). The proportion of anterior DR was significantly higher in earlier stages of NPDR, and the proportion showed a decreasing trend from mild to moderate to severe NPDR (Pearson's chi-square test, p < 0.001).
Nine eyes had an epiretinal membrane; four (44.4%) of these had anterior DR, three (33.3%) had diffuse DR, and two (22.3%) had posterior DR. Cataract extraction had been conducted in 49 eyes. Seven of the 49 eyes (14.3%) with a prior cataract extraction had anterior DR, 18 (36.7%) had posterior DR, and 24 (49%) had diffuse DR. Among the 206 eyes that had undergone OCT examination, DME was noted in 23 eyes (11.2%), of which 15 (65.2%) had posterior DR and the remaining eight (34.8%) had diffuse DR (Table 2).
Multiple logistic regression analysis including the variables age, sex, and body mass index indicated that there were significant differences in HbA1c and HDL-C between the three NPDR types (p = 0.027 and p = 0.017, respectively) (Table 1). HbA1c was significantly lower in patients with anterior DR than in patients with posterior or diffuse DR (p = 0.005 and p < 0.001, respectively), with mean HbA1c levels equal to 7.03 ± 0.99% in anterior DR, 7.99 ± 1.74% in posterior DR, and 7.94 ± 1.39% in diffuse DR. The HDL-C level was significantly higher in patients with anterior DR than in diffuse DR patients (p = 0.036), with mean HDL-C levels equal to 51.20 ± 12.50 mg/dL in anterior, 49.66 ± 15.21 mg/dL in posterior, and 45.23 ± 13.09 mg/dL in diffuse DR patients. There were no significant differences in best corrected visual acuity, fasting glucose levels, cholesterol, triglyceride, LDL-C, blood urine nitrogen, creatinine, glomerular filtration rate, urine albumin to creatinine ratio, hypertension, the proportion of diabetic nephropathy, use of insulin, or oral medication for diabetes between the three NPDR types (p > 0.05). Regarding intake of lipid lowering agents, the proportion of statin use was 21.7% in anterior DR, 57.9% in posterior DR, and 43.6% in diffuse DR individuals. The proportion was significantly lower in anterior DR patients (p = 0.005), when compared with the other DR types. Multiple logistic regression analysis also revealed that the proportion of males with posterior DR was approximately twice that of males with diffuse DR (p = 0.037; odds ratio, 2.1).
The prevalence of DME detected by OCT was also different between diffuse and posterior DR patients. The incidence of DME was 0% in anterior DR, 16.7% in posterior DR, and 6.7% in diffuse DR (Table 2). The presence of DME was observed more frequently in patients with posterior than those with diffuse DR (p = 0.025; odds ratio, 3.3).
Prior research has established that early diabetic retinal changes are detected primarily at the posterior pole. In our study, we focused on the anterior and posterior locational aspects of diabetic retinal changes, and demonstrated the presence of an anterior DR. There have been no reports that classify the types of DR according to location and that identify anterior DR as a separate entity.
The current study established that anterior DR was observed in approximately 10% of NPDR cases. Further, anterior DR was detected more frequently in cases of mild NPDR than in cases of moderate or severe NPDR. However, we suspect that the actual proportion of the anterior DR in the general diabetic population may be greater than the 10% reported in this study, because milder stages of DR could be more prevalent in the general diabetic population as opposed to the hospital-based diabetic patients in our study.
Anterior DR was not observed as frequently in moderate or severe cases of NPDR. A likely explanation for this observation is that the majority of anterior DR in mild cases of NPDR might have progressed to the diffuse type during advancement to moderate or severe NPDR. A separate possibility is that rapidly progressing DR is likely to present as posterior or diffuse DR, thereby skipping the mild NPDR stage. In the severe NPDR group, the proportion of anterior DR was 7%. According to the criteria described by ETDRS, severe NPDR is defined by the presence of venous beading and intraretinal microvascular abnormality in the standard photograph of the post pole. Thus, we should take into account the inherent discordance in the diagnosis of anterior DR in eyes with severe NPDR. In this study, a diagnosis of anterior DR in cases of severe NPDR was made when diabetic retinal changes corresponding to severe stage were only noted outside the overlaying circle. Patients with proliferative DR were not included, because it was relatively difficult to find cases of proliferative DR without a history of macular photocoagulation, pan-retinal photocoagulation, or anti-vascular endothelial growth factor treatment before examination with UWFA. All of the aforementioned conditions could potentially influence the incidence or identification of anterior DR. However, although the data are not presented, it was relatively difficult to identify proliferative diabetic changes limited to the outside of the overlaying circle. Thus, we presume that the prevalence of anterior DR in the proliferative stage of DR would be low.
One of the major findings of the current study was the relationship between anterior DR and blood profile components, including HbA1c and HDL-C levels. Even after adjusting for other factors, including duration of diabetes, age, sex, body mass index, and the results of other laboratory blood tests, anterior DR was significantly correlated with favorable blood sugar and lipid profile components, specifically low HbA1c levels and high HDL-C levels. Use of lipid-lowering agents, especially statins, which have a small effect on raising HDL-C levels, was also significantly lower in anterior DR patients.
The relationship between increased plasma lipoprotein levels and DR has been reported, and it has been hypothesized that lipoproteins cause vessel damage through lipoprotein oxidation and associated anti-fibrinolytic and prothrombotic effects [6]. Similarly, the Diabetes Control and Complications Trial group investigated the association of DR severity and retinal hard exudates with serum lipids [7]. As for glycemia, there was an apparent 35% to 40% reduction in retinopathy progression risk for every 10% decrease in HbA1c [89]. Epidemiologic analysis of the UK Prospective Diabetes Study data also revealed a continuous relationship between the risk of microvascular complication and glycemia [1011]. Elevated serum levels of LDL-C and triglyceride as well as low levels of HDL-C were also reported to be strongly associated with increased risk for macrovascular events, including ischemic stroke and coronary disease in patients with type 2 diabetes mellitus [1112]. Moreover, the Action to Control Cardiovascular Risk in Diabetes group of studies found significantly reduced DR progression rates in patients who received fenofibrate versus those who received a placebo [13]. Collectively, these studies showed that intensive control of blood sugar and lipid reduces the risk of DR development and progression of the disease as well as other complications, but does not prevent them completely. Other systemic factors, including hypertension and diabetic nephropathy, as measured by albuminuria, proteinuria, or urine albumin to creatinine ratio, have also been reported to affect DR progression [1415]. Some studies have reported that diabetic nephropathy was a risk factor associated with DR progression [151617]. It should be mentioned that all the above clinical studies were concerned about the stages of DR identified within seven-standard ETDRS fields.
Caution must be exercised when interpreting the results pertaining to the incidence of anterior DR and the apparent association with lower HbA1c or higher HDL-C levels. The results should not be used to assert that improved glycemic control or higher blood HDL levels aggravate any particular type of DR. Some studies have reported that a favorable lipid profile has protective effects on the development or DR progression and reduces the risk of vision loss. However, anterior DR may have been overlooked in these studies employing conventional imaging techniques that mainly enable a posterior view of the retina. Thus, we suspect that in some cases, which were not considered as DR in previous studies, anterior DR was likely present, especially in cases with favorable blood sugar or lipid profiles.
It is interesting to note that the duration of diabetes was not significantly related to the DR type. It has been maintained, based on the Diabetes Control and Complications Trial results, that the time course of DR development is a direct consequence of long-term hyperglycemia, and is therefore related to the duration of diabetes [8]. The current study suggests that respective diabetic patients have a predetermined DR development point, regardless of systemic control. However, DR would manifest first as the anterior type under well-controlled systemic conditions. In this case, it is highly suspected that peripheral diabetic changes are overlooked and assumed to be normal conditions. Because this study focused primarily on the identification of anterior DR and associated factors, the underlying pathogenesis related to the association between low HbA1c and high HDL-C levels and increased identification rates of anterior DR is beyond the scope of this study. However, based on observations that peripheral non-perfusion is frequently noted by UWFA in both normal and myopic eyes [18], we hypothesize that microvascular changes induced by diabetes may develop primarily in the periphery, where the retinal tissue is relatively vulnerable to low perfusion pressure or occlusive microangiopathies.
In the prior study of UWFA by Patel et al. [3], a larger extent of peripheral ischemia was related to the most recalcitrant form of DME. However, the current study showed that the incidence of DME was higher in posterior DR than those having diffuse DR. DME was not observed in anterior DR patients due to the definition of anterior DR in our study. The discrepancy between the two studies could be explained by the fact that the previous study did not classify retinal ischemia according to location, included PDR patients, and focused on the incidence of 'recalcitrant' DME without including simple DME.
The current study had several limitations. First, the results were derived from a limited number of cases. Second, besides the nature of retrospective study designs, patient enrollment from a tertiary hospital might have altered the proportion of early NPDR patients and thus, potential selection bias could not be eliminated. For a similar reason, OCT scans were not conducted in some cases, but the results were sufficient to analyze and compare the prevalence since there was no difference in data loss from OCT scans in each group. However, this study could represent the first step in describing anterior DR, which has not been previously reported. Long-term longitudinal observations are required to clarify further the clinical significance of anterior DR.
In conclusion, diabetic retinal changes limited only to anterior location were more frequently noted in the earlier stages of NPDR. Furthermore, the identification of anterior DR was significantly associated with relatively favorable blood sugar and lipid profiles in diabetic patients. Last, the results established that UWFA was a useful tool for the evaluation of this new DR type that has previously been overlooked.
Figures and Tables
Fig. 1
The overlaying circle used for classification of the diabetic retinopathy locational type. The circle is presented as a dotted line, encompassing the conventional seven-standard Early Treatment Diabetic Retinopathy Study fields. This case represents moderate non-proliferative diabetic retinopathy with diffuse involvement.

Fig. 2
The three types of non-proliferative diabetic retinopathy (DR): the anterior type of DR (A), the posterior type of DR (B), and the diffuse type of DR (C). If retinal changes were located only outside the overlaying circle, anterior type DR (A) was noted. Conversely, when microvascular changes were limited within the overlaying circle, posterior type DR (B) was assigned. If diabetic retinal changes were noted in both sides of the overlaying circle, diffuse type DR (C) was assigned. Imaginary boundary line (dotted line), which was encompassing the conventional seven-standard Early Treatment Diabetic Retinopathy Study fields (solid line), was used for the classification of anterior or posterior type of diabetic retinopathy.

Fig. 3
Anterior diabetic retinopathy (DR) stages: mild non-proliferative anterior DR (A), moderate non-proliferative anterior DR (B), severe non-proliferative anterior DR (C), and proliferative DR with anterior type DR (D). Proliferative DR (D) patients were not enrolled in this study.

Fig. 4
The proportion of the diabetic retinopathy types according to stage of non-proliferative diabetic retinopathy (NPDR).

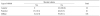
Table 1
Baseline characteristics of the eyes of study participants with non-proliferative diabetic retinopathy according to retinopathy type

Values are presented as mean ± standard deviation unless otherwise indicated.
logMAR = logarithm of the minimum angle of resolution; BCVA = best-corrected visual acuity; HDL-C = high-density lipoprotein-cholesterol; LDL-C = low-density lipoprotein-cholesterol; HbA1c = hemoglobin A1c; GFR= glomerular filtration rate; BUN = blood urine nitrogen; ACR = albumin to creatinine ratio.
References
1. Fundus photographic risk factors for progression of diabetic retinopathy: ETDRS report number 12. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991; 98:5 Suppl. 823–833.
2. Manivannan A, Plskova J, Farrow A, et al. Ultra-wide-field fluorescein angiography of the ocular fundus. Am J Ophthalmol. 2005; 140:525–527.
3. Patel RD, Messner LV, Teitelbaum B, et al. Characterization of ischemic index using ultra-widefield fluorescein angiography in patients with focal and diffuse recalcitrant diabetic macular edema. Am J Ophthalmol. 2013; 155:1038–1044.e2.
4. Wessel MM, Aaker GD, Parlitsis G, et al. Ultra-wide-field angiography improves the detection and classification of diabetic retinopathy. Retina. 2012; 32:785–791.
5. Ruilope LM, Segura J. Losartan and other angiotensin II antagonists for nephropathy in type 2 diabetes mellitus: a review of the clinical trial evidence. Clin Ther. 2003; 25:3044–3064.
6. Malaguarnera G, Gagliano C, Bucolo C, et al. Lipoprotein(a) serum levels in diabetic patients with retinopathy. Biomed Res Int. 2013; 2013:943505.
7. Lyons TJ, Jenkins AJ, Zheng D, et al. Diabetic retinopathy and serum lipoprotein subclasses in the DCCT/EDIC cohort. Invest Ophthalmol Vis Sci. 2004; 45:910–918.
8. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus: the Diabetes Control and Complications Trial Research Group. N Engl J Med. 1993; 329:977–986.
9. The absence of a glycemic threshold for the development of long-term complications: the perspective of the Diabetes Control and Complications Trial. Diabetes. 1996; 45:1289–1298.
10. The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the diabetes control and complications trial. Diabetes. 1995; 44:968–983.
11. Klein R, Klein BE, Moss SE. Relation of glycemic control to diabetic microvascular complications in diabetes mellitus. Ann Intern Med. 1996; 124(1 Pt 2):90–96.
12. Toth PP, Simko RJ, Palli SR, et al. The impact of serum lipids on risk for microangiopathy in patients with type 2 diabetes mellitus. Cardiovasc Diabetol. 2012; 11:109.
13. ACCORD Study Group. ACCORD Eye Study Group. Chew EY, et al. Effects of medical therapies on retinopathy progression in type 2 diabetes. N Engl J Med. 2010; 363:233–244.
14. Knowler WC, Bennett PH, Ballintine EJ. Increased incidence of retinopathy in diabetics with elevated blood pressure: a six-year follow-up study in Pima Indians. N Engl J Med. 1980; 302:645–650.
15. Rand LI, Prud'homme GJ, Ederer F, Canner PL. Factors influencing the development of visual loss in advanced diabetic retinopathy: Diabetic Retinopathy Study (DRS) report No. 10. Invest Ophthalmol Vis Sci. 1985; 26:983–991.
16. Janka HU, Warram JH, Rand LI, Krolewski AS. Risk factors for progression of background retinopathy in long-standing IDDM. Diabetes. 1989; 38:460–464.
17. Chew EY, Klein ML, Ferris FL 3rd, et al. Association of elevated serum lipid levels with retinal hard exudate in diabetic retinopathy: Early Treatment Diabetic Retinopathy Study (ETDRS) Report 22. Arch Ophthalmol. 1996; 114:1079–1084.
18. Kaneko Y, Moriyama M, Hirahara S, et al. Areas of nonperfusion in peripheral retina of eyes with pathologic myopia detected by ultra-widefield fluorescein angiography. Invest Ophthalmol Vis Sci. 2014; 55:1432–1439.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download