Abstract
Objective
Methods
Results
Figures and Tables
Figure 1
A, Thermoforming machine (Biostar®; Scheu Dental, Iserlohn, Germany) and fabrication of specimens for evaluation of the effects of thermoforming on the mechanical and physical properties of different thermoplastic materials with varying thicknesses. B, Surface X was cut from the models and used as a specimen for analysis.

Figure 2
Comparison of water absorption (A) and solubility (B) before thermoforming (BT) and after thermoforming (AT) and among different thermoplastic materials. All tests were performed for 1.0-mm-thick Duran, Essix A+, Essix ACE, and 0.75-mm-thick eCligner. The same capital letters indicate no difference between materials at the 1% significance level. The same lower case letters indicate no difference between BT and AT at the 1% significance level.

Figure 3
Comparison of Knoop hardness values before thermoforming (BT) and after thermoforming (AT) and among different thermoplastic materials. All tests were performed for 1.0-mm-thick Duran, Essix A+, Essix ACE, and 0.75-mm-thick eCligner. The same capital letter indicates no difference between materials at the 1% significance level. The same lower case letters indicate no difference between BT and AT at the 1% significance level.

Table 1
Properties of thermoplastic materials used for the fabrication of transparent orthodontic aligners and the thermoforming conditions used in the present study

Table 2
Comparison of the transparency of different thermoplastic materials before thermoforming (BT) and after thermoforming (AT)
Values are presented as mean ± standard deviation.
A,B,CThe same capital letters in the vertical columns indicate no difference between materials at the 1% significance level. a,bThe same lower case letters in the horizontal rows indicate no difference between BT and AT at the 1% significance level.
See Table 1 for the manufacturer of each product.
Table 3
Comparison of the flexural forces and flexure moduli for different thermoplastic materials before thermoforming (BT) and after thermoforming (AT)

Values are presented as mean ± standard deviation.
A,B,CThe same capital letters in the vertical columns indicate no difference between materials at the 1% significance level. a,bThe same lower case letters in the horizontal rows indicate no difference between BT and AT at the 1% significance level.
See Table 1 for the manufacturer of each product.
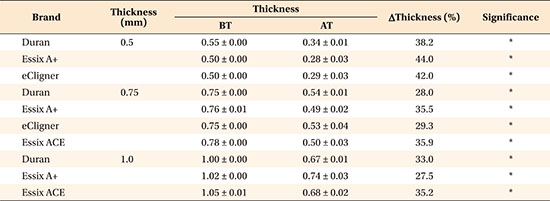
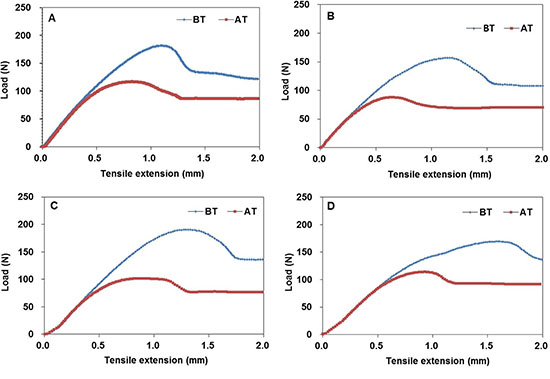
Table 4
Comparison of the tensile forces and elastic moduli for different thermoplastic materials before thermoforming (BT) and after thermoforming (AT)

Values are presented as mean ± standard deviation.
A,BThe same capital letters in the vertical columns indicate no difference between materials at the 1% significance level. a,bThe same lower case letters in the horizontal rows indicate no difference between BT and AT at the 1% significance level.
See Table 1 for the manufacturer of each product.
ACKNOWLEDGEMENTS
Notes
Appendices
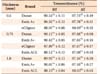
Appendix 1
Thickness variations for different thermoplastic materials used for the fabrication of transparent orthodontic aligners




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download