Abstract
Objective
Methods
Results
Figures and Tables
 | Figure 1Experimental protocol used in the present study. Immediately after implantation, the miniscrews on the left side were loaded. At 3 weeks after implantation, the miniscrews on the right side were loaded and the force on the left side was reactivated. At 4 weeks after implantation, the animals received intravenous tetracycline for fluorescence microscopy. At 6 weeks, the animals were sacrificed.TC, Tetracycline; IV, intravenous.
|
 | Figure 2Miniscrews placed in interradicular spaces in the posterior mandible of beagle dogs. An orthodontic force is applied using an elastomeric chain.U, No loading group (screw placed between the second and third premolars); L, loading groups (one screw is placed between the third and fourth premolars, while another is placed between the fourth premolar and first molar).
|
 | Figure 3Classification of orthodontic miniscrews according to the proximity to the adjacent tooth roots using hematoxylin and eosin-stained sections (12.5×). A, High root proximity group. The miniscrew is in contact with the adjacent tooth root. B, Low root proximity group. The miniscrew is touching the bundle bone or the periodontal ligament but not contacting the adjacent root. C, Safe distance group. The miniscrew is placed in the interradicular septum, without any contact with the bundle bone. |
 | Figure 4Root proximity of an orthodontic miniscrew without orthodontic loading and low root proximity, with atrophic changes in the adjacent periodontal ligament. A, A hematoxylin and eosin-stained section (50×). The arrow indicates a miniscrew thread touching the bundle bone. The distance from the miniscrew to the root surface is 0.494 mm. Narrowing of the periodontal ligament space can be observed (area in the box, shown in B). B, A fluorescence microscopy image with high magnification (100×). Active bone deposition can be observed as a bright green line (arrow) at the alveolar bone surface facing the periodontal ligament space. |
 | Figure 5Effects of the proximity of an orthodontic miniscrew body to the bundle bone on the surrounding bone. The images show hematoxylin and eosin-stained sections. A and C, These are miniscrews with low root proximity. The miniscrew threads are invading the bundle bone (boxes, 12.5×). The miniscrew in A was loaded immediately after insertion, whereas the miniscrew in C was loaded at 3 weeks after insertion. The area in the box in A is shown in B, while the area in the box in C is shown in D. B and D, There is no direct bone–implant contact around the threads within the bundle bone (yellow arrows, 100×). Resorption of the adjacent tooth root can be observed (blue arrows). |
Table 1
Comparison of BIC (%) values among three root proximity groups of orthodontic miniscrews placed in the posterior mandible of beagle dogs
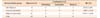
Values are presented as number only or mean ± standard deviation.
Unloading, Screws without orthodontic loading; Immediate, screws with immediate orthodontic loading; Delayed, screws with delayed orthodontic loading.
Differences among groups were determined by Kruskal–Wallis and post-hoc tests (Mann–Whitney U-test). *p < 0.05. Bone–implant contact (BIC [%]) is significantly different among the three root proximity groups (p = 0.000). Post-hoc tests show that BIC (%) is significantly lower in the high root proximity group than in the low root proximity (p = 0.001) and safe distance (p = 0.000) groups.
Table 2
Comparison of BIC (%) values among three loading times for orthodontic miniscrews in the posterior mandible of beagle dogs

Values are presented as number only or mean ± standard deviation.
The immediate loading group included the failed miniscrew with no bone–implant contact (BIC [%]).
High, Screws with high root proximity; Low, screws with low root proximity; Safe, screws at a safe distance from the adjacent tooth roots.
Differences among groups were examined by Kruskal–Wallis tests (p < 0.05).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download