Abstract
Purpose
To compare the characteristics of patients with surgically overcorrected intermittent exotropia treated with alternate patching.
Methods
The medical records of 51 patients who underwent bilateral lateral rectus muscle recession for intermittent exotropia and required alternate patching to correct postoperative overcorrection were retrospectively reviewed. Patients with postoperative esodeviation ≥18 prism diopters (PD) were started on alternate patching on postoperative day 1, whereas those with postoperative esodeviation of 10 to 17 PD were started after 2 weeks. Postoperative esodeviation <10 PD was considered as slight intentional overcorrection after exotropia surgery. Patients not responsive to alternate patching treatment were defined as those with postoperative esodeviation ≥10 PD after 3 months of treatment. Sex, family history, age, refractive error, amblyopia, stereopsis, suppression, type of exotropia, surgical method, preoperative and postoperative angle of deviation, and start time of alternate patching were compared.
Results
Among 51 patients, 29 patients responded to alternate patching and 22 patients did not respond. Female sex (p = 0.04), larger preoperative exodeviation at distance (p = 0.04), late onset of postoperative maximal esodeviation (p < 0.01), larger postoperative maximal esodeviation at near (p = 0.02), and late initiation of alternate patching (p = 0.01) were associated with patients in the non-responsive group. Although postoperative angle of deviation was similar for 2 weeks, the angle of postoperative esodeviation was significantly larger in the non-responsive group than in the responsive group, beginning at 1 month postoperatively.
Intermittent exotropia (IXT) is an ocular condition encountered more often in Asian countries than in Western ones [12]. It remains under discussion which alignment right after surgery for IXT (orthotropia vs. slight esotropia) yields better long-term results [34]. Most surgeons treating IXT overcorrect the deviation slightly by 10 prism diopters (PD) to 15 PD to allow for the natural exodrift that has been shown to occur post-surgically [567]. Thus, several guidelines recommend waiting for two weeks after surgery in patients with overcorrection without limitations in ocular movement [891011]. However, an overcorrection of more than 17 PD immediately after surgery has been found to increase the risk of persistent consecutive esotropia; thus, an overcorrection of more than 20 PD is not recommended [8121314]. Excessive overcorrection and consecutive esotropia after surgery for IXT can cause diplopia. In children it can also lead to worsening stereopsis and amblyopia, indicating the need for timely and proper treatment [1516].
Overcorrection can be treated surgically or non-surgically. However, it is difficult to predict the long-term outcomes of surgical treatment; moreover, the operation itself and the use of general anesthesia can be burdensome to both the operator and patients. Therefore, non-surgical methods should be considered prior to second surgery, except in cases of severe limitation in ocular movement [717181920]. Among the non-surgical treatment methods are alternate patching, correction of hyperopia, bifocal glasses, prism glasses, and injection of botulinum toxin [11181920].
Alternate patching is considered a primary modality because it is easily performed and prevents amblyopia. The exact effect of alternate patching has not been clearly identified, but it has been reported to be effective in reducing the size of the suppression scotoma and anomalous retinal correspondence and in improving the fusional amplitude by restricting binocular stimulation [21]. However, a second surgery should be considered in patients who experience >15 PD esodeviation for longer than 6 months, a condition known as consecutive esotropia, despite the use of non-surgical treatment [11].
Several studies have compared risk factors in patients who are responsive or resistant to alternate patching treatment with prism glasses prescription [79]. This current study, however, compared factors in patients responsive and non-responsive to alternate patching treatment alone for overcorrection after surgery for IXT.
The medical records of 505 patients who underwent bilateral lateral rectus muscle (BLR) recession for IXT performed by a single surgeon between February 2005 and December 2014 and who were followed for more than 6 months were reviewed retrospectively. Of the 505 patients, 51 (10.1%) patients who required alternate patching to correct postoperative overcorrection were included in this study. The study protocol was approved by the institutional review board of Inje University Haeundae Paik Hospital (129792-2015-108) and informed consent was waived due to retrospective design. The study followed the tenets of the Declaration of Helsinki.
Because the risk of consecutive esotropia is increased if postoperative overcorrection exceeds 17 PD immediately following surgery [8], patients with postoperative esodeviation ≥18 PD were started on alternate patching treatment the day after their operation; otherwise, patients with postoperative esodeviation of 10 to 17 PD at distance or near were started on alternate patching treatment at 2 weeks or later postoperative, while postoperative esodeviation <10 PD was considered to represent slight intentional overcorrection after exotropia surgery [11]. The responsive group was defined as patients who responded to alternate patching and who showed a postoperative esodeviation of <10 PD at distance and near after at least 3 months of patching, whereas the non-responsive group was defined as patients with constant esotropia ≥10 PD remaining after 3 months of alternate patching treatment.
To analyze the effects of pure alternate patching treatment, patients who were prescribed prism glasses within six months after surgery were excluded from this study. Furthermore, patients who had undergone additional strabismus surgery, had eye diseases such as cataracts and/or retinal disorders other than strabismus, or who had neurologic diseases such as mental retardation or cerebral palsy, were also excluded. Lastly, those who underwent unilateral lateral rectus muscle recession and medial rectus muscle resection for IXT were excluded to reduce bias.
Factors compared in the responsive and non-responsive groups included sex, family history of strabismus, ages at diagnosis and surgery, preoperative observation period, refractive error, anisometropia, spherical equivalent after cycloplegic refraction, and high myopia (i.e., ≥−6.00 D). Amblyopia was defined as a difference between eyes with respect to best-corrected visual acuity of two or more lines on Snellen visual acuity charts or best-corrected visual acuity of lower than 20 / 30. Amblyopia treatment included wearing an eye patch over the unaffected eye. Notably, any occlusion therapy for amblyopia was completed more than 1 year before exotropia surgery; thus, it is unlikely to have affected the alternate patching outcomes after surgery. Patients who had recovered from amblyopia and who thus did not require further occlusion therapy before surgery were included in the non-amblyopia group.
When possible, sensory status was evaluated preoperatively. Preoperative suppression was evaluated with the Worth 4-dot test at distance and near. Stereopsis was measured using the Titmus test at near and defined as good when stereoacuity was ≤100 arc/sec; this value is a minimal index of fine and useful central stereoacuity [1922].
The preoperative deviation was evaluated by alternate prism cover test at 33 cm for near and at 6 m for distance while wearing glasses, if glasses were required. The classification of exotropia, lateral incomitance, vertical deviation, and the presence of A or V patterns were also evaluated.
Subjects included in the analysis were either basic, convergence insufficient, pseudo-divergence excess, or true divergence excess IXT. When the distance deviation was nearly equal to the near deviation <10 PD, it was defined as basic IXT. Convergence insufficient IXT was characterized by a greater exodeviation at near than at distance of by 10 PD or more. When the prism cover test showed that the exodeviation was significantly larger at distance than at near, by 10 PD or more but, with 30-minute patching test or +3.0 D spherical test, deviation at near was equal to distance, it was defined as pseudo-divergence excess IXT. If deviation at near remained as less than 10 PD or more after 30 minutes of patching, true divergence excess IXT was diagnosed.
Lateral incomitance was defined as incomitance when the deviation on the lateral gaze differed more than 20% from the angle of deviation in the primary position. Comitant vertical deviation was defined as a vertical deviation ≥5 PD in the primary position without variation in the gazes. The surgical extent of BLR was based on the amount suggested by Raab and Parks [8].
Postoperative factors compared in the responsive and non-responsive groups included the time of initiation of alternate patching treatment, change of deviation, onset time, and angle of maximum postoperative esodeviation. In each patient, the maximum postoperative esodeviation was defined as one single maximum angle of esodeviation during the observation period after surgery.
Deviation was measured at one day; 1 and 2 weeks; and 1, 2, 3, and 6 months after surgery, respectively. At the beginning of alternate patching, the patch was applied for the full time of the patient being awake. If esodeviation was reduced to <10 PD, patching times were reduced to 8 hours, 4 to 6 hours, and then 2 hours, in a gradual fashion. If there was no improvement in esodeviation, alternate patching was maintained full-time. If the esodeviation did not resolve after one month, cycloplegic refraction was performed to identify any residual hyperopia ≥+1.50 D. There was no case requiring the addition of hyperopic correction postoperatively found in this study. Patients who began patching 2 weeks following surgery were also started on full-time alternate patching. Compliance of the alternate patching regimen was made by creating a schedule table and checked by the patient and their parents together when they reached the goal.
SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. Continuous variables were compared using Mann-Whitney U-tests and discrete variables were compared using chi-squared tests and Fisher exact tests. A p-value less than 0.05 was considered statistically significant.
Of 51 patients who required alternate patching to correct postoperative overcorrection, 29 (56.9%) improved following alternate patching (i.e., those in the responsive group) and 22 (43.1%) did not (i.e., those in the non-responsive group).
The mean follow-up period of the 51 patients was 31.1 ± 16.9 months (range, 6 to 61 months). There was no difference in mean follow-up period for each group (responsive group vs. non-responsive group: 31.1 ± 18.2 months vs. 31.1 ± 16.6 months, p = 0.30).
A comparison of preoperative factors in the two groups showed a significant difference in sex distribution, with the percentage of female patients being higher in the non-responsive than in the responsive group (responsive group vs. non-responsive group: 48.3% vs. 77.3%, p = 0.04) (Table 1). There were no significant differences between groups regarding family history of strabismus, age at diagnosis and surgery, interval from diagnosis to surgery, spherical equivalent, anisometropia, and high myopia. There were also no differences in the presence of amblyopia, suppression, and stereopsis. Preoperative exodeviation at distance was significantly larger in the non-responsive group (responsive group vs. non-responsive group: 25.3 ± 4.4 vs. 27.0 ± 6.0 PD, p = 0.04). There were no significant differences between the two groups in classifications of exotropia (i.e., basic, convergence insufficient, pseudo-divergence excess, true-divergence excess IXT); lateral incomitance; vertical deviation (inferior oblique overaction, dissociated vertical deviation, and comitant vertical deviation); or the presence of an A or V pattern.
A comparison of postoperative factors in the two groups showed that the mean start time of alternate patching was significantly later (responsive group vs. non-responsive group: 10.2 ± 9.6 vs. 23.6 ± 25.6 days, p = 0.01) and that the percentage of patients starting alternate patching within the first 2 weeks after surgery was significantly lower (responsive group vs. non-responsive group: 86.2% vs. 45.5%, p < 0.01) in the non-responsive group than in the responsive group (Table 2). Although the angle of postoperative maximal esodeviation at distance did not differ significantly in the two groups, postoperative maximal esodeviation at near was significantly greater in the non-responsive group (responsive group vs. non-responsive group: −14.7 ± 8.5 vs. −20.0±6.9 PD, p = 0.02). The onset times of postoperative maximal esodeviation at distance (responsive group vs. non-responsive group: 0.3 ± 0.2 vs. 2.3 ± 2.1 months, p < 0.01) and at near (responsive group vs. non-responsive group: 0.4 ± 0.3 vs. 3.4 ± 4.1 months, p < 0.01) were significantly later in the non-responsive group than in the responsive group.
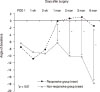
Regarding change in postoperative angle of deviation, there were no significant differences in either the angle of deviation at distance, the angle of deviation at near, or the difference between distance and near deviation in the first 2 weeks after surgery. However, beginning 1 month after surgery, the angle of esodeviation was larger in the non-responsive group, both at distance (Fig. 1) and at near (Fig. 2). In the responsive group, the average deviation recovered close to orthotropia at both distance and at near after 1 month. In the non-responsive group, although esodeviation was smaller at 1 month than at 2 weeks postoperatively in both at distance and near, there was no significant difference in findings between at 2 weeks and at 1 month postoperatively with regard to at distance (p = 0.20) and near (p = 0.21). However, esodeviation was significantly higher at both distance and near (p = 0.04 each) after 2 months versus after 1 month in the non-responsive group.
Of the 22 patients in the non-responsive group, 14 underwent a second operation because they demonstrated esodeviation ≥10 PD for more than 6 months and did not want prism glasses; following this second surgery, 12 of these 14 patients recovered to orthotropia. Of the two patients who showed persistent esodeviation after the second surgery, one exhibited an esodeviation of 12 PD and showed improvements in esotropia with prism glasses and the second experienced a recurrence of esotropia of 30 PD but recovered to orthotropia after a third operation. Of the eight patients who did not undergo a second operation for esotropia, two showed improvements in esotropia with prism glasses, five were lost to follow-up, and one is awaiting a second operation.
Mild surgical overcorrection immediately after IXT surgery can be transient because of the exodrift that typically occurs with time [7121523]. Consecutive esotropia, however, can result from persistent overcorrection. One study involving patients who experienced overcorrection immediately after exotropia surgery found that, at last follow-up, 36% of these patients were orthotropic, 24% were undercorrected, and 40% were overcorrected [2425]. Although excellent alignment outcomes can result from early overcorrection after surgery, the rate of consecutive esotropia was also higher in patients who were overcorrected than in those who were orthotropic after surgery. Thus, it is difficult to predict final outcomes in patients who experience early overcorrection after exotropia surgery. Also, it is difficult to predict long-term motor outcomes [26] or the onset and progress of consecutive esotropia [17] using the initial angle of postsurgical overcorrection.
Many studies have assessed the risk factors and treatments of consecutive esotropia after surgery for IXT. Our previous study found that risk factors for consecutive esotropia included high myopia, amblyopia, the presence of 25 to 40 PD of preoperative exotropia at distance, a >10 PD difference between distance and near deviation, lateral incomitance, tenacious proximal convergence fusion type, and rectus muscle resection surgery [23]. Another study reported that risk factors for consecutive esotropia included divergence excess type exotropia, BLR, amblyopia, young age at diagnosis and surgery, short follow-up period from the onset of exotropia to surgery, and ≥20 PD overcorrection on the first day after surgery [7]. The present study is different from previous studies in that it compared patients with postoperative esodeviation who were responsive and non-responsive to alternate patching. According to our findings, the risk factors for being non-responsive to alternate patching were female sex, large preoperative exodeviation at distance, large esodeviation 1 month after surgery, and late initiation of alternate patching.
Non-surgical treatments of consecutive esotropia usually include alternate patching treatment with or without prism glasses if necessary. Patients non-responsive to these non-surgical treatments may require surgery. One study found that when patients were divided into surgical and non-surgical groups (alternate patching and/or with prism glasses), there were no significant differences between the group in terms of ages at diagnosis and surgery; preoperative factors such as preoperative angle of deviation, lateral incomitance and refractive errors; and degree of overcorrection after one day [9]. However, esodeviation at distance after one month was significantly higher in those who were surgically treated, similarly to what was seen in the results of our study.
Another comparison of patients treated surgically and non-surgically for consecutive esotropia found no differences in angles of deviation after one day and one week and also indicated that younger patients were more responsive to non-surgical treatment, although they were more prone to consecutive esotropia [7]. The study concluded that it was impossible to predict the need for surgery to correct consecutive esotropia based on the deviation angle 1 to 2 weeks after surgery.
In analyzing the effects of alternate patching treatment alone, sex distribution differed significantly, with more female patients being present in the non-responsive group than in the responsive group. Notably, previous studies pointed out no significant difference in sex distribution in consecutive esotropia [9]. The results of our study may be contributed to by the higher prevalence of exotropia in females in Korea, which may have led to the higher prevalence of consecutive esotropia in females shown in our study. A larger preoperative exodeviation at distance also predisposed patients to refractoriness, but none of the other preoperative factors differed significantly between the responsive and non-responsive groups.
Assessments of postoperative factors in these two groups found no differences in angle of deviation for the first 2 weeks after surgery. Thus, it is difficult to predict the occurrence of and recovery from consecutive esotropia based on the degree of overcorrection immediately after surgery. One month after surgery, the average deviation in the responsive group had recovered close to orthotropia, with this group showing significant differences as compared with the non-responsive group at distance and near. The difference in angle of deviation between these two groups also increased gradually. The most important factor influencing the decision to perform surgery in patients with consecutive esotropia has been reported to be a large esodeviation 1 month after surgery [927].
In our study, alternate patching was started significantly later in the non-responsive group than in the responsive group, suggesting that the earlier initiation of alternate patching may increase its effectiveness. We recommend initiate patching earlier even in cases of small postoperative esodeviation, since the immediate postoperative angle of deviation isn't predictive of responsiveness and those patients who begin alternate patching earlier demonstrate better response rates. Early intervention may restore and improve binocular visual function, because esodeviation is apt to persist if it remains at a level higher than 10 PD 2 months after surgery [28].
The postoperative esodeviation increased in the non-responsive group despite alternate patching treatment and maximum esodeviations appeared after 2.3 ± 2.1 months at distance and after 3.4 ± 4.1 months at near. In contrast, postoperative esodeviations decreased gradually in the responsive group, with maximum esodeviations appearing after 0.3 ± 0.2 months at distance and 0.4 ± 0.3 months at near. The increased esodeviation in the non-responsive group, which appeared despite the use of alternate patching treatment, is thought to be due to decompensation of the convergence-divergence mechanism [10]. Even the patients who maintain orthotropia after surgery for a certain period may later develop consecutive esotropia. Woo and Choi [27] reported ten patients with delayed consecutive esotropia. The patients demonstrated 21 PD of esotropia at an average time of 4 months postoperatively. Delayed consecutive esotropia was at its most prevalent 2 to 4 months after surgery. These patients generally respond poorly to non-surgical treatments, such as alternate patching and Fresnel prism. Six of the ten patients recovered to orthotropia or esotropia within 10 PD, but the other four required surgical corrections because the esotropia persisted or doubled in severity [27].
Similar results were observed in the non-responsive group in this study. Two patients in this study showed delayed consecutive esotropia at 2 and 3 months, respectively, after surgery. Both of these individuals required surgery because alternate patching was not effective. Thus, despite improvements in postoperative overcorrection, close follow-up is needed because consecutive esotropia can develop at a later time and esodeviation may increase.
The operation for consecutive esotropia should be considered and performed at 6 months after surgery in patients who are non-responsive to alternate patching treatment. Thus, the follow-up period for determining the pure effectiveness of alternate patching treatment in patients with overcorrected IXT is limited to 6 months at minimum.
Our study has several limitations that call for further research. First, our study was retrospective in nature. Prospective studies that strictly control for other factors are needed to confirm our results. Second, there was no control group included in our study. In the case of a relatively small angle for esodeviation, especially in the responsive group, it is possible that the esodeviation may disappear over time without any special treatment such as alternate patching. Third, the relatively short follow-up of a minimum of 6 months after surgery for IXT may be another limiting factor for this study. Fourth, there is also an issue of control scores. In our study, control scores for IXT were not included, which possibly related to treatment and prognosis of IXT. However, we supposed that most patients who have undergone IXT surgery had bad control scores.
In conclusion, patients of the female sex with a large preoperative exodeviation at distance and a large angle and late onset of postoperative maximal esodeviation are less responsive to alternate patching treatment for managing overcorrection after IXT surgery. The patients will respond poorly to further alternate patching treatment if esodeviation does not recover close to orthotropia after alternate patching treatment for one month after surgery. In these patients, surgery rather than alternate patching should be considered earlier, potentially in conjunction with additional treatments such as prism glasses.
Figures and Tables
 | Fig. 1Postoperative changes in the mean angle of deviation at distance in patients responsive and nonresponsive to alternate patching treatment. There were significant differences between the two groups, with esodeviation nearly recovering in the responsive group after 1 month. (−) means esodeviation and (+) means exodeviation. POD = postoperative day. |
 | Fig. 2Postoperative changes in the mean angle of deviation at near in patients responsive and nonresponsive to alternate patching treatment. There were significant differences between the two groups after 1 month. (−) means esodeviation and (+) means exodeviation. POD = postoperative day. |
Table 1
Preoperative factors in groups of patients with overcorrected IXT who were responsive and non-responsive to alternate patching treatment

Values are presented as number (%) or mean ± standard deviation (range); (−) means esodeviation and (+) means exodeviation.
IXT = intermittent exotropia; D = diopter; PD = prism diopter; IOOA = inferior oblique overaction; DVD = dissociated vertical deviation.
*Fisher's exact test; †Mann-Whitney U-test; ‡Chi-squared test.
Notes
References
1. Park H, Kim WJ, Kim MM. The stabilization of postoperative exo-drift in intermittent exotropia after surgical treatment. Korean J Ophthalmol. 2016; 30:60–65.

2. Yang M, Chen J, Shen T, et al. Clinical characteristics and surgical outcomes in patients with intermittent exotropia: a large sample study in south China. Medicine (Baltimore). 2016; 95:e2590.
3. Campos E. Surgical correction and outcome of exotropia. Asia Pac J Ophthalmol (Phila). 2015; 4:185–186.

4. Chang YH, Melvin P, Dagi LR. Goal-determined metrics to assess outcomes of exotropia surgery. J AAPOS. 2015; 19:304–310.
5. Clarke WN, Noel LP. Surgical results in intermittent exotropia. Can J Ophthalmol. 1981; 16:66–69.
7. Kim HJ, Choi DG. Consecutive esotropia after surgery for intermittent exotropia: the clinical course and factors associated with the onset. Br J Ophthalmol. 2014; 98:871–875.

8. Raab EL, Parks MM. Recession of the lateral recti: early and late postoperative alignments. Arch Ophthalmol. 1969; 82:203–208.
9. Choi YM, Lee JY, Jung JH, et al. Risk factors predicting the need for additional surgery in consecutive esotropia. J Pediatr Ophthalmol Strabismus. 2013; 50:335–339.

10. von Noorden GK. Binocular vision and ocular motility. St. Louis: CV Mosby;1994. p. 438–442.
11. Hardesty HH. Treatment of overcorrected intermittent exotropia. Am J Ophthalmol. 1968; 66:80–86.

12. Park KH, Kim SY. Clinical characteristics of patients that experience different rates of exodrift after strabismus surgery for intermittent exotropia and the effect of the rate of exodrift on final ocular alignment. J AAPOS. 2013; 17:54–58.
13. Wagner RS. Consecutive esotropia following surgery for intermittent exotropia. J Pediatr Ophthalmol Strabismus. 2013; 50:334.

14. Souza-Dias C. Postoperative evolution of the planned initial overcorrection in intermittent exotropia: 61 cases. Binocul Vis Eye Muscle Surg Q. 1993; 8:141–148.
15. Kim DW, Han S, Kim US, Baek SH. Results of conservative management for consecutive esotropia after intermittent exotropia surgery. Eye (Lond). 2015; 29:776–782.

16. Pineles SL, Ela-Dalman N, Zvansky AG, et al. Long-term results of the surgical management of intermittent exotropia. J AAPOS. 2010; 14:298–304.

17. Kim YH, Choi MY. The effect of fresnel prism treatment in consecutive esotropia. J Korean Ophthalmol Soc. 2006; 47:1623–1629.
18. Lee EK, Hwang JM. Prismatic correction of consecutive esotropia in children after a unilateral recession and resection procedure. Ophthalmology. 2013; 120:504–511.

19. Lee EK, Yang HK, Hwang JM. Long-term outcome of prismatic correction in children with consecutive esotropia after bilateral lateral rectus recession. Br J Ophthalmol. 2015; 99:342–345.

20. Dawson EL, Marshman WE, Lee JP. Role of botulinum toxin A in surgically overcorrected exotropia. J AAPOS. 1999; 3:269–271.

21. von Noorden GK, Campos EC. Principles of nonsurgical treatment. 5th ed. St. Louis: Mosby-Year Book;1996. p. 503.
22. Na KI, Lee JY. Consecutive esotropia after lateral rectus muscle recession for intermittent exotropia. J Korean Ophthalmol Soc. 2012; 53:1318–1323.

23. Jang JH, Park JM, Lee SJ. Factors predisposing to consecutive esotropia after surgery to correct intermittent exotropia. Graefes Arch Clin Exp Ophthalmol. 2012; 250:1485–1490.

24. Buck D, Powell CJ, Sloper JJ, et al. Surgical intervention in childhood intermittent exotropia: current practice and clinical outcomes from an observational cohort study. Br J Ophthalmol. 2012; 96:1291–1295.

25. Buck D, Powell C, Sloper J, et al. Authors' response: after intermittent exotropia surgery, consecutive esotropia: good or bad? by K K Shoaib. Br J Ophthalmol. 2013; 97:797–798.

26. Choi J, Kim SJ, Yu YS. Initial postoperative deviation as a predictor of long-term outcome after surgery for intermittent exotropia. J AAPOS. 2011; 15:224–229.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download