Abstract
Purpose
To investigate the effect of surgically induced corneal astigmatism (SICA) and total corneal astigmatism (TCA) estimation on the anterior corneal astigmatism (ACA)-based toric intraocular lens (IOL) calculation.
Methods
Data from preoperative and postoperative corneal astigmatism, postoperative visual acuities, and refractive outcomes were collected. The incision was superior in with the rule anterior corneal astigmatism (WTRA) eyes and temporal in against the rule anterior corneal astigmatism eyes. The following five methods of calculating the toric IOL were compared: (1) ACA only and estimated SICA; (2) ACA with a fixed posterior corneal astigmatism (PCA) and estimated SICA; (3) ACA with a fixed PCA value and actual SICA; (4) and (5) TCA derived from the regression equations of ACA and actual SICA. The residual astigmatism was simulated. The Alpins method was used to analyze the astigmatism.
Results
Sixty eyes from 46 patients were enrolled. Thirty eyes had WTRA and the other thirty had against the rule anterior corneal astigmatism. The vector and arithmetic means of the difference vector decreased when the information regarding the actual SICA and PCA was added to the calculation (from 0.59 diopters [D] @ 87.5° to 0.15 D @ 48.5°, and from 0.95 ± 0.53 to 0.71 ± 0.63 D, respectively; p < 0.001). The mean difference vector across the whole sample was lowest using model 5. The correction index was significantly closest to 1.0 in the WTRA group.
The aim of modern refractive cataract surgery is not only to correct spherical errors but also to correct astigmatism. The prevalence of at least 1.0 diopter (D) pre-existing astigmatism is 36.2% to 45.0% [12]. Toric intraocular lens (IOL) implantation is an effective method to correct astigmatism at the time of cataract surgery [3456].
The main variables in the calculation of toric power of the IOL include preexisting corneal astigmatism and surgically induced corneal astigmatism (SICA). Total corneal astigmatism (TCA) is the sum of anterior and posterior corneal astigmatism (ACA and PCA). In most cases, ACA plays a vital role, because its magnitude tends to be much larger than that of PCA [7]. Recent studies have reported that the prevalence of against the rule (ATR) posterior corneal astigmatism is 59% to 73.9% and 96.6% to 97% in eyes with ATR anterior corneal astigmatism (ATRA) and with the rule anterior corneal astigmatism (WTRA), respectively [78]. Therefore, the toric IOL calculation using devices that only measure the anterior corneal surface lead to ATR errors, which results in overcorrection in WTRA eyes and undercorrection in ATRA eyes [910]. In order to overcome these errors when calculating the toric IOL, we assumed that the PCA was −0.3 D @ 90° in eyes with WTRA, and −0.2 D @ 90° in eyes with ATRA. These estimates are based on previous reports, and our own experience [911]. In this study, we performed vector analysis on the basis of our results. We re-calculated these values using the simulated models, and added information regarding the actual SICA and the PCA regression equations.
The study protocol followed the tenets of the Declaration of Helsinki. This study was approved by our institutional review and ethical board (1603-031-747). We retrospectively reviewed the medical records of patients who met the following inclusion criteria: patients who had implanted Tecnis toric IOL (ZCT 150, ZCT 225, ZCT 300, and ZCT 400; Abbott Medical Optics, Santa Ana, CA, USA) from August, 2013, through September, 2015 at Seoul National University Hospital; 20 years or older; regular corneal astigmatism between 1.0 and 3.63 D; requirement of a spherical equivalent lens power between +6.0 and +28.0 D. Patients with any of the following characteristics were excluded: irregular astigmatism, amblyopia, keratoconus, previous refractive or keratoplasty surgery, advanced glaucoma, corneal scarring, uveitis, significant macular disease, postoperative corrected distance visual acuity <20 / 40 or zonule/pupil abnormalities. Patients were also excluded if there were intraoperative complications, including posterior capsular rupture, vitreous loss, and zonular damage. According to the keratometric data, corneal astigmatism was defined by the presence of with the rule (60°–120°) and ATR (0°–30° or 150°–180°). Therefore, we only included patients who had WTRA or ATRA in this study.
Preoperatively, patients underwent a complete ophthalmic evaluation. This included uncorrected distance visual acuity and corrected distance visual acuity measurements, slit lamp examination, tonometry, and fundoscopy. Preoperative corneal keratometry was performed using three different devices, as follows: (1) autokeratorefractometer (KR-8900; Topcon, Tokyo, Japan), (2) IOL Master (Carl Zeiss Meditec, Dublin, CA, USA), and (3) Orbscan IIz topography (Bausch & Lomb, Claremont, CA, USA). Each examination was performed in triplicate and the results were averaged.
The selection of the IOL cylinder was determined using the IOL manufacturer's web-based calculator (http://www.amoeasy.com/calc), avoiding the axis flip. The biometry, keratometry, incision location, and surgeon's estimated SICA were entered into the calculator. The incision location was superior (90°) in WTRA eyes and temporal (0° or 180°) in ATRA eyes. The estimated SICA was used as −0.2 D. In order to overcome errors caused by posterior astigmatism, we assumed that the posterior astigmatism was −0.3 D @ 90° in WTRA eyes and −0.2 D @ 90° in ATRA eyes (model 2). Three keratometry values, derived from the three different devices, were entered. Three respective results were calculated. The most consistent, or median toricity, and the corresponding axis were selected.
We selected the toric IOL spherical power based on the IOL Master (Carl Zeiss Meditec). The target postoperative spherical equivalent was defined by the nearest negative emmetropic value or myopic value (range, −1.0 to −3.0 D) based on the patient's preoperative spherical equivalent refractive error and visual needs.
At one month postoperatively, manifest refraction was performed. We also measured corneal astigmatism at this time using an auto kerato refractometer. All refractive cylindrical errors were described as minus cylinder form. The refractive cylinder at the spectacle plane was converted into the corneal plane using a vertex distance of 12 mm for the astigmatism analysis.
The TECNIS toric IOLs are one-piece, aspheric, hydrophobic, foldable acrylic lenses. They have ultraviolet light absorbing clear IOLs [12]. The cylinder IOL power can be calculated using the manufacturer's web-based calculator based on the Holladay 1 formula. The IOL is available in spherical ranges of +5.0 to +34.0 D in 0.5-D increments. The toric cylinder power is +1.5 (ZCT 150), +2.25 (ZCT 225), +3.0 (ZCT 300), and +4.0 (ZCT 400) D measured at the IOL plane. These correspond to +1.03, +1.54, +2.06, and +2.74 D, respectively at the corneal plane of the average pseudophakic eye.
The same experienced surgeon (MKK) performed all of the surgeries using topical and subtenon anesthesia. Preoperatively, limbal reference marks were made under the slit lamp at the 3- and 9-o'clock meridians using an insulin needle with the patient sitting upright. During surgery, the axis was marked using a Mendez ring (K3-7900; Katena, Denville, NJ, USA) and a toric axis marker (K3-7910; Katena) at the preplaced reference marks. A 2.75-mm self-sealing 3-step clear corneal incision was made using a disposable metal blade (Alcon Laboratories, Fort Worth, TX, USA) on the superior (90°) or temporal (0° or 180°) eye according to the steep corneal meridian. Phacoemulsification was performed using the Ozil Infiniti Vision System (Alcon Laboratories). After toric IOL insertion, the IOL was placed approximately 20° counterclockwise from the planned axis. After the viscoelastic material was removed, the IOL was rotated clockwise and aligned to the intended axis.
All data were compared among the following five models. The predicted residual astigmatism values in model 1, and in models 3 to 5, were re-calculated from model 2. The PCA and SICA values were adjusted to correspond to each model.
Model 1: TCA = preoperative keratometric astigmatism (PKA; no consideration of PCA) and an estimated SICA of −0.2 D
Model 2: TCA = PKA + PCA values of −0.3 D @ 90° and −0.2 D @ 90° for WTRA and ATRA, respectively; an estimated SICA of −0.2 D
Model 3: TCA = PKA + PCA values of −0.3 D @ 90° and −0.2 D @ 90° for WTRA and ATRA, respectively; the actual (not estimated) average SICA
Model 4: TCA = adjustment of PKA according to the Baylor nomogram, which is calculated using the published regression equations [91113]: subtracting (0.1005 × PKA + 0.221) or adding (−0.011 × PKA + 0.225) to PKA for WTRA and ATRA, respectively; the actual mean SICA
Model 5: TCA = PKA + a PCA that is estimated on the basis of the regression model reported by Eom et al. [14]: −(0.15 × PKA + 0.22) D @ 90° and −0.27 D @ 90° for WTRA and ATRA, respectively; the actual mean SICA
The results obtained 1 month after surgery were analyzed. TCA was used as the preoperative corneal astigmatism value. All calculations were performed using vector analysis [15]. For astigmatism analysis, Alpins method [1617] was used, as follows. (1) Surgically induced astigmatism vector (SIA), which is actually an induced cylinder vector by surgery. (2) Target induced astigmatism vector (TIA), which is an intended cylinder vector for astigmatism surgery. (3) Difference vector (DV), which is a vector from the achieved astigmatism to the target astigmatism. The DV is an absolute value of success. Therefore, its ideal value is zero. Clinically, the DV is the vector difference between the postoperative refractive cylinder error (achieved astigmatism) and the residual astigmatism suggested by the calculation (intended astigmatism). In this study, the DV was the main factor determining the accuracy of the toric IOL calculation. (4) Correction index (CI), which is the ratio of the SIA to the TIA (calculated by dividing SIA by TIA). A CI >1.0 and <1.0 refer to overcorrection and undercorrection, respectively. (5) Angle of error, which is the angle difference between the SIA and TIA. Positive and negative values of angle of error refer to mean counterclockwise and clockwise rotation from its intended axis, respectively.
Categorical variables were compared using the Fisher exact test or the chi-square exact test, as appropriate. For differences between continuous variables, the independent t-test was used. In order to compare the five models, we used repeated-measure one-way analysis of variance with a post hoc Bonferroni correction. All analyses were performed using IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA). Double-angle plots with 95% confidence ellipses were obtained using Sigmaplot ver. 12.5 (Systat Software Inc., San Jose, CA, USA) and R ver. 3.3.1 (R Foundation, Vienna, Austria). A p-value <0.05 was considered statistically significant.
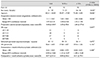
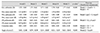
The study enrolled a total of 60 eyes from 46 patients. Thirty eyes had WTRA, while the other 30 eyes had ATRA. Table 1 summarizes the demographic, preoperative biometric, implanted IOL, and postoperative results. The mean age of the WTRA group (52.47 ± 17.29) was significantly younger than that of the ATRA group (71.00 ± 8.92). The mean preoperative astigmatism was 2.12 ± 0.62 D. The WTRA group (2.43 ± 0.63 D) had more astigmatism than did the ATRA group (1.80 ± 0.44 D). The difference was significant (p < 0.001); however, the type of IOL toricity was not significantly different between the two groups (p = 0.065). The mean refractive cylinders of all patients, the WTRA group, and ATRA group were −0.82 ± 0.63, −0.84 ± 0.73, and −0.80 ± 0.52 D, respectively, at one month postoperatively. These differences were not statistically significant between the two groups (p = 0.800).The changes in corneal astigmatism between the preoperative and one month postoperative values (actual mean SICA) were 0.53 D @ 102.9° in the WTRA group (superior incision) and 0.20 D @ 4.4° in the ATRA group (temporal incision). Table 2 shows the results of the five models throughout the whole sample. The vector and arithmetic means of the DV in model 1 were significantly larger than were those in the other models (p < 0.001). There were further improvements in DV when the actual mean SICA (model 3) was used. The mean vector of the DV was lowest in model 5 (0.15 D @ 48.5°), although the arithmetic mean of the DV was not significantly different between models 3 through 5. The CI in models 4 and 5 was significantly better than those in the other models. Table 3 shows the results of the five models in eyes with WTRA. The vector and arithmetic means of the DV in model 1 were significantly larger than those of the other models (p ≤ 0.001). The mean vector of the DV was similar in models 3 to 5. The arithmetic means of the DV were not significantly different between models 3 through 5. The CI progressively decreased from models 1 through 5; this was a significant trend, indicating that the PCA obtained using the regression model and the actual mean SICA had improved the problem of overcorrection.
Table 4 shows the results of the five models in eyes with ATRA. The vector and arithmetic means of the DV in model 1 were significantly larger than were those of other models (p < 0.001). The mean vector of the DV was lowest in model 5 (0.19 D @ 81.0°), although the arithmetic mean of the DV was not significantly different across models 2 through 5. The CI showed a significantly increasing trend in models 1 through 5. This result indicates that both PCA obtained using the regression model and the actual mean SICA had improved the problem of undercorrection.
Fig. 1 shows the double-angle plots with the 95% confidence ellipses of the DV in the WTRA and ATRA groups. Generally, the ellipses and centers in models 1 through 5 are positioned closer to the origin as the number of the model increases.
The accurate calculation of toric IOL implantation requires precise measurements. This study investigated how to improve the accuracy of toric IOL calculations, and particularly ACA-based calculations. The accuracy of the calculation improved when we considered the presumed effect of the PCA (estimated using regression models). It also improved when we used the mean of the actual SICA.
The real TCA can be calculated from 3-dimensional anterior segment optical coherence tomography [18] and Scheimpflug corneal topography [710]. The calculation using these devices would more predictable than that using ACA only [1019]. However, Reitblat et al. [20] reported that the mean vector of the refractive error is lowest in the Baylor toric nomogram. This nomogram estimates PCA on the basis of ACA. However, the arithmetic mean of the refractive error was lowest when using the vector summation method, which employs the PCA measured using the Scheimpflug camera. The researchers recommended using the vector summation method, or the Baylor toric nomogram, which accounts for the effect of PCA. These results are similar to those of the present study. The arithmetic and mean vectors of the DV in models 2 to 5, in which PCA was considered, were better than those in model 1, in which PCA was not considered. Many clinical facilities do not have devices that can calculate PCA. Therefore, it is necessary to analyze how to improve the accuracy of ACA only-based toric IOL calculations.
In order to predict the PCA on the basis of the ACA, many studies have used the regression equation method [7111314]. The regression equation used in model 4 was derived from 715 subjects. This equation was used to estimate the absolute PCA value. The TCA was calculated by directly subtracting or adding the estimated absolute PCA to the ACA [1113]. The regression equation used in model 5 was derived from 928 subjects. It estimated the PCA values on the 90° axis. The TCA was calculated by adding the estimated PCA to the ACA [14]. This regression model used a fixed PCA in eyes with ATRA because regression analysis was not significant. This finding corroborates those of Miyake et al. [7], who reported that the magnitude of PCA is related to the magnitude of anterior astigmatism in eyes with WTRA, but not in those with ATRA.
The mean vector of the DV was lowest in model 5, although the arithmetic mean was not significantly different across models 3 through 5. In model 5, the CI was closest to 1.0 in the WTRA group. Taken together, the results indicate that model 5 may have yielded the best results, for several reasons. For instance, the regression used in model 5 is derived from a larger sample of subjects than was that in the other models. In addition, the regression equation used in model 5 was applied to the same ethnic group as in this study.
In this study, the mean age of the ATRA group was older than that of the WTRA group. This finding is in line with previous studies, which have shown that corneal astigmatism changes toward ATRA with age. PCA also changes to ATR with age, although this change is small and/or insignificant [1121]. The regression equations in this study only used ACA to obtain PCA. Therefore, their accuracy might be enhanced by considering age.
Tejedor and Perez-Rodriguez [22] evaluated 110 patients who received a 2.8-mm clear corneal incisions. The group found that a superior corneal incision (0.53 D) results in higher surgically induced refractive change than do temporal incisions (0.21 D). Rho and Joo [23] also evaluated 95 patients who underwent 3.0-mm clear corneal incision, and reported that the SICA is 0.46 D in superior and 0.28 D in temporal incisions. These results corroborate those of our study, in which the actual mean SICA was 0.53 D @ 102.9° with a superior incision, and 0.20 D @ 4.4° with a temporal incision. The explanation for this finding is currently unclear. However, one possible reason for the difference may be the distance between the optical center and the incision location, which is longer with temporal incisions than it is with superior incisions [24].
The DV and CI tended to be better when using the actual mean SICA (model 3) rather than the estimated SICA (model 2). This outcome agrees with that of a previous study, in which error was reduced when the IOL was recalculated using the actual mean SICA in subjects who had undergone toric IOL implantation [19]. The SICA is different depending on the operator; therefore, the expected SICA should be tailored to each surgeon's experience. This study has several limitations. These include its retrospective design, small sample size and short follow-up period. In addition, we were unable to examine the axis of the toric IOL postoperatively. Nevertheless, the angle of error ranged from −1.21° to 0.71° in this study. The rotation of the TECNIS toric IOL has been reported to range from 2.7° to 3.4° [12252627]. A final limitation is that we included patients with myopic spherical equivalent targets.
In summary, the mean vector of the DV improved from 0.59 D @ 87.5° to 0.15 D @ 48.5° when using (1) the actual mean SICA, and (2) the TCA calculated by adding the PCA derived from the ACA regression equation. Our study confirms the results of previous studies, in which the toric IOL calculation (neglecting PCA) resulted in overcorrection and undercorrection in eyes with WTRA and ATRA, respectively. The actual mean SICA (calculated on the basis of real surgical results), and a TCA that accounts for PCA, would improve the accuracy of the toric IOL calculation. In order to predict PCA, it is advisable to use a regression equation model derived from a large number of subjects. Our results will be meaningful for surgeons who calculate the toric IOL on the basis of the anterior corneal surface only.
Figures and Tables
Fig. 1
Double-angle plots of the difference vector with 95% confidence ellipses in eyes with with the rule anterior corneal astigmatism (red) and those with against the rule anterior corneal astigmatism (blue) in models 1 through 5.

Notes
References
1. Pan CW, Klein BE, Cotch MF, et al. Racial variations in the prevalence of refractive errors in the United States: the multi-ethnic study of atherosclerosis. Am J Ophthalmol. 2013; 155:1129–1138.

2. Vitale S, Ellwein L, Cotch MF, et al. Prevalence of refractive error in the United States, 1999–2004. Arch Ophthalmol. 2008; 126:1111–1119.

3. Lam DK, Chow VW, Ye C, et al. Comparative evaluation of aspheric toric intraocular lens implantation and limbal relaxing incisions in eyes with cataracts and ≤3 dioptres of astigmatism. Br J Ophthalmol. 2016; 100:258–262.

4. Mingo-Botin D, Munoz-Negrete FJ, Won Kim HR, et al. Comparison of toric intraocular lenses and peripheral corneal relaxing incisions to treat astigmatism during cataract surgery. J Cataract Refract Surg. 2010; 36:1700–1708.
5. Nagpal R, Sharma N, Vasavada V, et al. Toric intraocular lens versus monofocal intraocular lens implantation and photorefractive keratectomy: a randomized controlled trial. Am J Ophthalmol. 2015; 160:479–486.

6. Titiyal JS, Khatik M, Sharma N, et al. Toric intraocular lens implantation versus astigmatic keratotomy to correct astigmatism during phacoemulsification. J Cataract Refract Surg. 2014; 40:741–747.

7. Miyake T, Shimizu K, Kamiya K. Distribution of posterior corneal astigmatism according to axis orientation of anterior corneal astigmatism. PLoS One. 2015; 10:e0117194.

8. Tonn B, Klaproth OK, Kohnen T. Anterior surface-based keratometry compared with Scheimpf lug tomography-based total corneal astigmatism. Invest Ophthalmol Vis Sci. 2014; 56:291–298.
9. Koch DD, Jenkins RB, Weikert MP, et al. Correcting astigmatism with toric intraocular lenses: effect of posterior corneal astigmatism. J Cataract Refract Surg. 2013; 39:1803–1809.

10. Zhang L, Sy ME, Mai H, et al. Effect of posterior corneal astigmatism on refractive outcomes after toric intraocular lens implantation. J Cataract Refract Surg. 2015; 41:84–89.

11. Koch DD, Ali SF, Weikert MP, et al. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012; 38:2080–2087.

12. Waltz KL, Featherstone K, Tsai L, Trentacost D. Clinical outcomes of TECNIS toric intraocular lens implantation after cataract removal in patients with corneal astigmatism. Ophthalmology. 2015; 122:39–47.
13. Abulafia A, Barrett GD, Kleinmann G, et al. Prediction of refractive outcomes with toric intraocular lens implantation. J Cataract Refract Surg. 2015; 41:936–944.

14. Eom Y, Rhim JW, Kang SY, et al. Toric intraocular lens calculations using ratio of anterior to posterior corneal cylinder power. Am J Ophthalmol. 2015; 160:717–724.

15. Holladay JT, Moran JR, Kezirian GM. Analysis of aggregate surgically induced refractive change, prediction error, and intraocular astigmatism. J Cataract Refract Surg. 2001; 27:61–79.

17. Alpins NA, Goggin M. Practical astigmatism analysis for refractive outcomes in cataract and refractive surgery. Surv Ophthalmol. 2004; 49:109–122.

18. Ueno Y, Hiraoka T, Miyazaki M, et al. Corneal thickness profile and posterior corneal astigmatism in normal corneas. Ophthalmology. 2015; 122:1072–1078.

19. Savini G, Naeser K. An analysis of the factors influencing the residual refractive astigmatism after cataract surgery with toric intraocular lenses. Invest Ophthalmol Vis Sci. 2015; 56:827–835.

20. Reitblat O, Levy A, Kleinmann G, et al. Effect of posterior corneal astigmatism on power calculation and alignment of toric intraocular lenses: comparison of methodologies. J Cataract Refract Surg. 2016; 42:217–225.

21. Ho JD, Liou SW, Tsai RJ, Tsai CY. Effects of aging on anterior and posterior corneal astigmatism. Cornea. 2010; 29:632–637.

22. Tejedor J, Perez-Rodriguez JA. Astigmatic change induced by 2.8-mm corneal incisions for cataract surgery. Invest Ophthalmol Vis Sci. 2009; 50:989–994.

23. Rho CR, Joo CK. Effects of steep meridian incision on corneal astigmatism in phacoemulsification cataract surgery. J Cataract Refract Surg. 2012; 38:666–671.

24. Cillino S, Morreale D, Mauceri A, et al. Temporal versus superior approach phacoemulsification: short-term postoperative astigmatism. J Cataract Refract Surg. 1997; 23:267–271.

25. Sheppard AL, Wolffsohn JS, Bhatt U, et al. Clinical outcomes after implantation of a new hydrophobic acrylic toric IOL during routine cataract surgery. J Cataract Refract Surg. 2013; 39:41–47.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download