1. Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002; 347:1233–1241. PMID:
12393820.

2. Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002; 347:1227–1232. PMID:
12393819.

3. Singletary SE. Surgical margins in patients with early-stage breast cancer treated with breast conservation therapy. Am J Surg. 2002; 184:383–393. PMID:
12433599.

4. Houssami N, Macaskill P, Marinovich ML, Dixon JM, Irwig L, Brennan ME, et al. Meta-analysis of the impact of surgical margins on local recurrence in women with early-stage invasive breast cancer treated with breast-conserving therapy. Eur J Cancer. 2010; 46:3219–3232. PMID:
20817513.

5. Park AY, Seo BK. Real-time MRI navigated ultrasound for preoperative tumor evaluation in breast cancer patients: technique and clinical implementation. Korean J Radiol. 2016; 17:695–705. PMID:
27587958.

6. Azu M, Abrahamse P, Katz SJ, Jagsi R, Morrow M. What is an adequate margin for breast-conserving surgery? Surgeon attitudes and correlates. Ann Surg Oncol. 2010; 17:558–563. PMID:
19847566.

7. Bani MR, Lux MP, Heusinger K, Wenkel E, Magener A, Schulz-Wendtland R, et al. Factors correlating with reexcision after breast-conserving therapy. Eur J Surg Oncol. 2009; 35:32–37. PMID:
18539425.

8. Lovrics PJ, Cornacchi SD, Farrokhyar F, Garnett A, Chen V, Franic S, et al. The relationship between surgical factors and margin status after breast-conservation surgery for early stage breast cancer. Am J Surg. 2009; 197:740–746. PMID:
18789424.

9. Park S, Park HS, Kim SI, Koo JS, Park BW, Lee KS. The impact of a focally positive resection margin on the local control in patients treated with breast-conserving therapy. Jpn J Clin Oncol. 2011; 41:600–608. PMID:
21355001.

10. Melstrom LG, Melstrom KA, Wang EC, Pilewskie M, Winchester DJ. Ductal carcinoma in situ: size and resection volume predict margin status. Am J Clin Oncol. 2010; 33:438–442. PMID:
20023569.
11. Seo M, Cho N, Bae MS, Koo HR, Kim WH, Lee SH, et al. Features of undiagnosed breast cancers at screening breast MR imaging and potential utility of computer-aided evaluation. Korean J Radiol. 2016; 17:59–68. PMID:
26798217.

12. Chen SQ, Huang M, Shen YY, Liu CL, Xu CX. Abbreviated MRI protocols for detecting breast cancer in women with dense breasts. Korean J Radiol. 2017; 18:470–475. PMID:
28458599.

13. Chung A, Saouaf R, Scharre K, Phillips E. The impact of MRI on the treatment of DCIS. Am Surg. 2005; 71:705–710. PMID:
16468502.

14. Del Frate C, Borghese L, Cedolini C, Bestagno A, Puglisi F, Isola M, et al. Role of pre-surgical breast MRI in the management of invasive breast carcinoma. Breast. 2007; 16:469–481. PMID:
17433681.

15. Schnall M. MR imaging evaluation of cancer extent: is there clinical relevance? Magn Reson Imaging Clin N Am. 2006; 14:379–381. viiPMID:
17098178.

16. Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007; 25:118–145. PMID:
17159189.

17. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC cancer staging manual. 7th ed. New York, NY: Springer;2010.
18. D'Orsi CJ, Sickles EA, Mendelson EB, Morris EA. ACR BI-RADS atlas, breast imaging reporting and data system. Reston, VA: American College of Radiology;2013.
19. Camp ER, McAuliffe PF, Gilroy JS, Morris CG, Lind DS, Mendenhall NP, et al. Minimizing local recurrence after breast conserving therapy using intraoperative shaved margins to determine pathologic tumor clearance. J Am Coll Surg. 2005; 201:855–861. PMID:
16310688.

20. Turnbull L, Brown S, Harvey I, Olivier C, Drew P, Napp V, et al. Comparative effectiveness of MRI in breast cancer (COMICE) trial: a randomised controlled trial. Lancet. 2010; 375:563–571. PMID:
20159292.

21. Houssami N, Turner R, Morrow M. Preoperative magnetic resonance imaging in breast cancer: meta-analysis of surgical outcomes. Ann Surg. 2013; 257:249–255. PMID:
23187751.
22. Pengel KE, Loo CE, Teertstra HJ, Muller SH, Wesseling J, Peterse JL, et al. The impact of preoperative MRI on breast-conserving surgery of invasive cancer: a comparative cohort study. Breast Cancer Res Treat. 2009; 116:161–169. PMID:
18807269.

23. Mann RM, Loo CE, Wobbes T, Bult P, Barentsz JO, Gilhuijs KG, et al. The impact of preoperative breast MRI on the re-excision rate in invasive lobular carcinoma of the breast. Breast Cancer Res Treat. 2010; 119:415–422. PMID:
19885731.

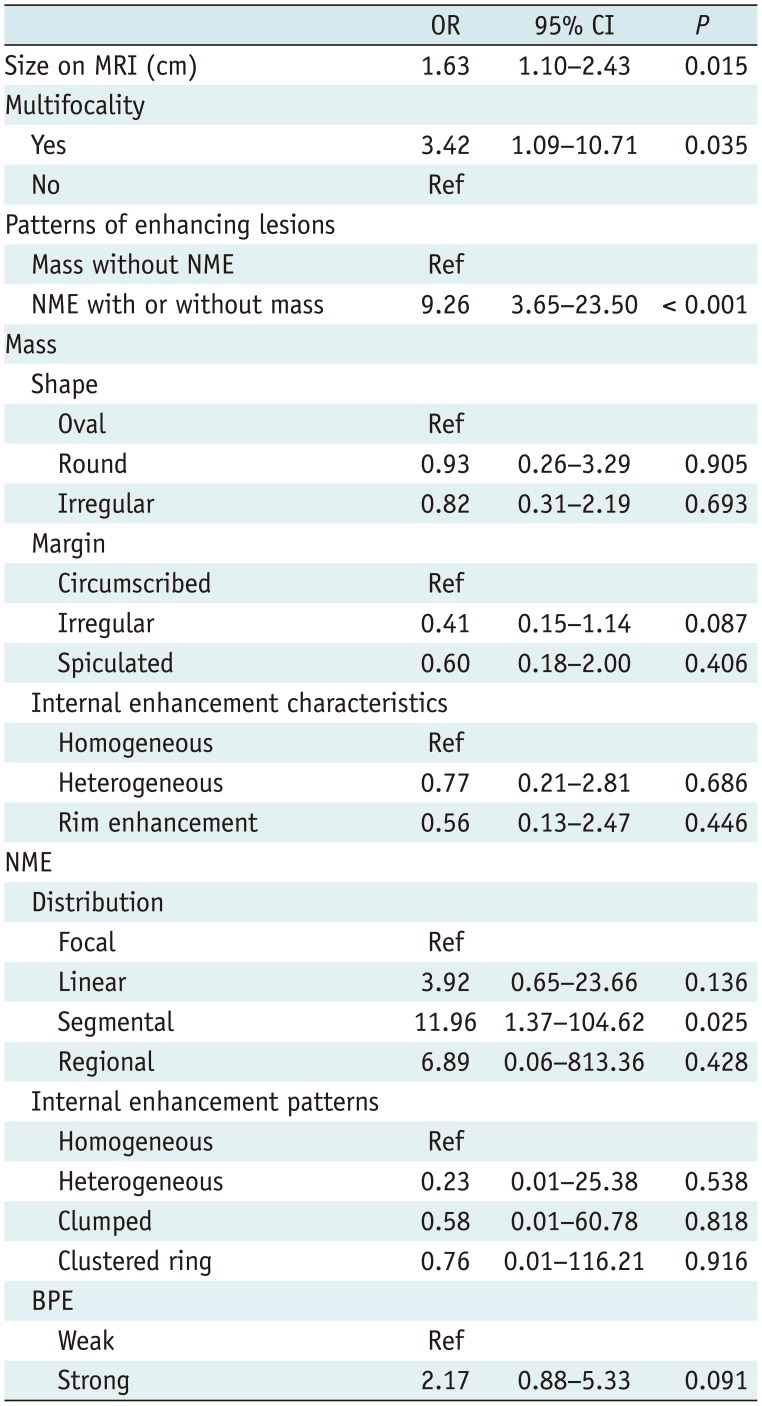
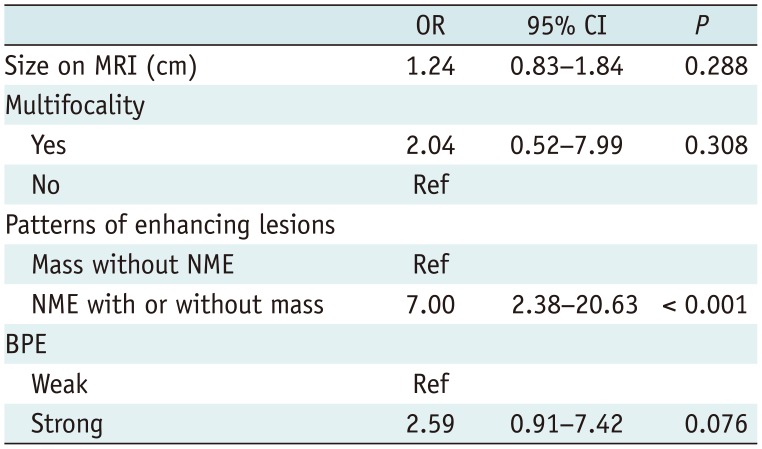
24. Kim OH, Kim SJ, Lee JS. Enhancing patterns of breast cancer on preoperative dynamic contrast-enhanced magnetic resonance imaging and resection margin in breast conserving therapy. Breast Dis. 2016; 36:27–35. PMID:
27177341.

25. Jang M, Kim SM, Yun BL, Kim SW, Kang EY, Park SY, et al. Magnetic resonance imaging factors predicting re-excision in breast cancer patients having undergone conserving therapy. J Korean Soc Magn Reson Med. 2014; 18:133–143.

26. Sakamoto N, Tozaki M, Higa K, Tsunoda Y, Ogawa T, Abe S, et al. Categorization of non-mass-like breast lesions detected by MRI. Breast Cancer. 2008; 15:241–246. PMID:
18224381.

27. Tozaki M, Fukuda K. High-spatial-resolution MRI of non-masslike breast lesions: interpretation model based on BI-RADS MRI descriptors. AJR Am J Roentgenol. 2006; 187:330–337. PMID:
16861534.

28. Vag T, Baltzer PA, Dietzel M, Benndorf M, Gajda M, Camara O, et al. Kinetic characteristics of ductal carcinoma in situ (DCIS) in dynamic breast MRI using computer-assisted analysis. Acta Radiol. 2010; 51:955–961. PMID:
20942728.

29. Dillon MF, Hill AD, Quinn CM, McDermott EW, O'Higgins N. A pathologic assessment of adequate margin status in breast-conserving therapy. Ann Surg Oncol. 2006; 13:333–339. PMID:
16474911.

30. Miller AR, Brandao G, Prihoda TJ, Hill C, Cruz AB Jr, Yeh IT. Positive margins following surgical resection of breast carcinoma: analysis of pathologic correlates. J Surg Oncol. 2004; 86:134–140. PMID:
15170651.

31. DiPiro PJ, Krajewski KM, Giardino AA, Braschi-Amirfarzan M, Ramaiya NH. Radiology consultation in the era of precision oncology: a review of consultation models and services in the tertiary setting. Korean J Radiol. 2017; 18:18–27. PMID:
28096715.

32. Seo M, Ryu JK, Jahng GH, Sohn YM, Rhee SJ, Oh JH, et al. Estimation of T2
* relaxation time of breast cancer: correlation with clinical, imaging and pathological features. Korean J Radiol. 2017; 18:238–248. PMID:
28096732.
33. Park SY, Kang DK, Kim TH. Does background parenchymal enhancement on MRI affect the rate of positive resection margin in breast cancer patients? Br J Radiol. 2015; 88:20140638. PMID:
25429418.

34. Millet I, Pages E, Hoa D, Merigeaud S, Curros Doyon F, Prat X, et al. Pearls and pitfalls in breast MRI. Br J Radiol. 2012; 85:197–207. PMID:
22128131.

35. Giess CS, Yeh ED, Raza S, Birdwell RL. Background parenchymal enhancement at breast MR imaging: normal patterns, diagnostic challenges, and potential for false-positive and false-negative interpretation. Radiographics. 2014; 34:234–247. PMID:
24428293.

36. Shimauchi A, Jansen SA, Abe H, Jaskowiak N, Schmidt RA, Newstead GM. Breast cancers not detected at MRI: review of false-negative lesions. AJR Am J Roentgenol. 2010; 194:1674–1679. PMID:
20489112.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download