1. Dubey JP. The history of Toxoplasma gondii: the first 100 years. J Eukaryot Microbiol. 2008; 55:467–475. PMID:
19120791.
2. Foroutan M, Dalvand S, Daryani A, et al. Rolling up the pieces of a puzzle: a systematic review and meta-analysis of the prevalence of toxoplasmosis in Iran. Alexandria J Med. 2017; 6. 23. [Epub]. DOI:
10.1016/j.ajme.2017.06.003.

3. Rostami A, Riahi SM, Fakhri Y, et al. The global seroprevalence of Toxoplasma gondii among wild boars: a systematic review and meta-analysis. Vet Parasitol. 2017; 244:12–20. PMID:
28917302.

4. Foroutan-Rad M, Majidiani H, Dalvand S, et al. Toxoplasmosis in blood sonors: a systematic review and meta-analysis. Transfus Med Rev. 2016; 30:116–122. PMID:
27145927.
5. Wang ZD, Liu HH, Ma ZX, et al. Toxoplasma gondii infection in immunocompromised patients: a systematic review and meta-analysis. Front Microbiol. 2017; 8:389. PMID:
28337191.

6. Pappas G, Roussos N, Falagas ME. Toxoplasmosis snapshots: global status of Toxoplasma gondii seroprevalence and implications for pregnancy and congenital toxoplasmosis. Int J Parasitol. 2009; 39:1385–1394. PMID:
19433092.

7. Khademvatan S, Foroutan M, Hazrati-Tappeh K, et al. Toxoplasmosis in rodents: a systematic review and meta-analysis in Iran. J Infect Public Health. 2017; 10:487–493. PMID:
28237696.

8. Foroutan M, Majidiani H. Toxoplasma gondii: are there any implications for routine blood screening? Int J Infect. 2018; 5:e62886.

9. Khademvatan S, Saki J, Yousefi E, Abdizadeh R. Detection and genotyping of Toxoplasma gondii strains isolated from birds in the southwest of Iran. Br Poult Sci. 2013; 54:76–80. PMID:
23444856.
10. Nasiri V, Teymurzadeh S, Karimi G, Nasiri M. Molecular detection of Toxoplasma gondii in snakes. Exp Parasitol. 2016; 169:102–106. PMID:
27522027.

11. Wei HX, He C, Yang PL, Lindsay DS, Peng HJ. Relationship between cat contact and infection by Toxoplasma gondii in humans: a meta-analysis. Comp Parasitol. 2016; 83:11–19.

12. Belluco S, Mancin M, Conficoni D, Simonato G, Pietrobelli M, Ricci A. Investigating the determinants of Toxoplasma gondii prevalence in meat: a systematic review and meta-regression. PLoS One. 2016; 11:e0153856. PMID:
27082633.

13. Majidiani H, Dalvand S, Daryani A, Galvan-Ramirez ML, Foroutan-Rad M. Is chronic toxoplasmosis a risk factor for diabetes mellitus? A systematic review and meta-analysis of case-control studies. Braz J Infect Dis. 2016; 20:605–609. PMID:
27768900.

14. Foroutan M, Rostami A, Majidiani H, et al. A systematic review and meta-analysis of the prevalence of toxoplasmosis in hemodialysis patients in Iran. Epidemiol Health. 2018; 40:e2018016. PMID:
29748456.

15. Yousefi E, Foroutan M, Salehi R, Khademvatan S. Detection of acute and chronic toxoplasmosis amongst multi-transfused thalassemia patients in southwest of Iran. J Acute Dis. 2017; 6:120–125.

16. Foroutan-Rad M, Khademvatan S, Majidiani H, Aryamand S, Rahim F, Malehi AS. Seroprevalence of Toxoplasma gondii in the Iranian pregnant women: a systematic review and meta-analysis. Acta Trop. 2016; 158:160–169. PMID:
26952970.
17. Saki J, Shafieenia S, Foroutan-Rad M. Seroprevalence of toxoplasmosis in diabetic pregnant women in southwestern of Iran. J Parasit Dis. 2016; 40:1586–1589. PMID:
27876989.

18. Fallahi S, Rostami A, Nourollahpour Shiadeh M, Behniafar H, Paktinat S. An updated literature review on maternal-fetal and reproductive disorders of Toxoplasma gondii infection. J Gynecol Obstet Hum Reprod. 2018; 47:133–140. PMID:
29229361.

19. Torgerson PR, Mastroiacovo P. The global burden of congenital toxoplasmosis: a systematic review. Bull World Health Organ. 2013; 91:501–508. PMID:
23825877.

20. Sullivan WJ Jr, Jeffers V. Mechanisms of Toxoplasma gondii persistence and latency. FEMS Microbiol Rev. 2012; 36:717–733. PMID:
22091606.
21. Antczak M, Dzitko K, Dlugonska H. Human toxoplasmosis-searching for novel chemotherapeutics. Biomed Pharmacother. 2016; 82:677–684. PMID:
27470411.

22. Weiss LM, Dubey JP. Toxoplasmosis: a history of clinical observations. Int J Parasitol. 2009; 39:895–901. PMID:
19217908.

23. Rostami A, Karanis P, Fallahi S. Advances in serological, imaging techniques and molecular diagnosis of Toxoplasma gondii infection. Infection. 2018; 46:303–315. PMID:
29330674.

24. Zhang NZ, Wang M, Xu Y, Petersen E, Zhu XQ. Recent advances in developing vaccines against Toxoplasma gondii: an update. Expert Rev Vaccines. 2015; 14:1609–1621. PMID:
26467840.
25. Lim SS, Othman RY. Recent advances in Toxoplasma gondii immunotherapeutics. Korean J Parasitol. 2014; 52:581–593. PMID:
25548409.

26. Hiszczynska-Sawicka E, Gatkowska JM, Grzybowski MM, Dlugonska H. Veterinary vaccines against toxoplasmosis. Parasitology. 2014; 141:1365–1378. PMID:
24805159.

27. Foroutan M, Ghaffarifar F. Calcium-dependent protein kinases are potential targets for Toxoplasma gondii vaccine. Clin Exp Vaccine Res. 2018; 7:24–36. PMID:
29399577.
28. Foroutan M, Ghaffarifar F, Sharifi Z, Dalimi A, Pirestani M. Bioinformatics analysis of ROP8 protein to improve vaccine design against Toxoplasma gondii. Infect Genet Evol. 2018; 62:193–204. PMID:
29705360.

29. Kur J, Holec-Gasior L, Hiszczynska-Sawicka E. Current status of toxoplasmosis vaccine development. Expert Rev Vaccines. 2009; 8:791–808. PMID:
19485758.

30. Vazini H, Ghafarifar F, Sharifi Z, Dalimi A. Evaluation of immune responses induced by GRA7 and ROP2 genes by DNA vaccine cocktails against acute toxoplasmosis in BALB/c mice. Avicenna J Med Biotechnol. 2018; 10:2–8. PMID:
29296260.
31. Naserifar R, Ghaffarifar F, Dalimi A, Sharifi Z, Solhjoo K, Hosseinian Khosroshahi K. Evaluation of immunogenicity of cocktail DNA vaccine containing plasmids encoding complete GRA5, SAG1, and ROP2 antigens of Toxoplasma gondii in BALB/C mice. Iran J Parasitol. 2015; 10:590–598. PMID:
26811726.
32. Ghaffarifar F, Naserifar R, Jafari Madrak M. Eukaryotic plasmids with Toxoplasma gondii dense granule antigen (GRA5) and microneme 3 (MIC3) genes as a cocktail DNA vaccine and evaluation of immune responses in BALB/C mice. J Clin Med Genomics. 2014; 3:121.

33. Khosroshahi KH, Ghaffarifar F, Sharifi Z, et al. Comparing the effect of IL-12 genetic adjuvant and alum non-genetic adjuvant on the efficiency of the cocktail DNA vaccine containing plasmids encoding SAG-1 and ROP-2 of Toxoplasma gondii. Parasitol Res. 2012; 111:403–411. PMID:
22350714.

34. Eslamirad Z, Dalimi A, Ghaffarifar F, Sharifi Z, Hosseini AZ. Induction of protective immunity against toxoplasmosis in mice by immunization with a plasmid encoding Toxoplama gondii ROP1 gene. Afr J Biotechnol. 2012; 11:8735–8741.

35. Hoseinian Khosroshahi K, Ghaffarifar F, D'Souza S, Sharifi Z, Dalimi A. Evaluation of the immune response induced by DNA vaccine cocktail expressing complete SAG1 and ROP2 genes against toxoplasmosis. Vaccine. 2011; 29:778–783. PMID:
21095254.

36. Solhjoo K, Ghaffari Far F, Dalimi-Asl A, Sharifi Z. Enhancement of antibody immune response to a Toxoplasma gondii SAGl-encoded DNA vaccine by formulation with aluminum phosphate. J Med Sci. 2007; 7:361–367.
37. Chen J, Li ZY, Petersen E, Huang SY, Zhou DH, Zhu XQ. DNA vaccination with genes encoding Toxoplasma gondii antigens ROP5 and GRA15 induces protective immunity against toxoplasmosis in Kunming mice. Expert Rev Vaccines. 2015; 14:617–624. PMID:
25749394.
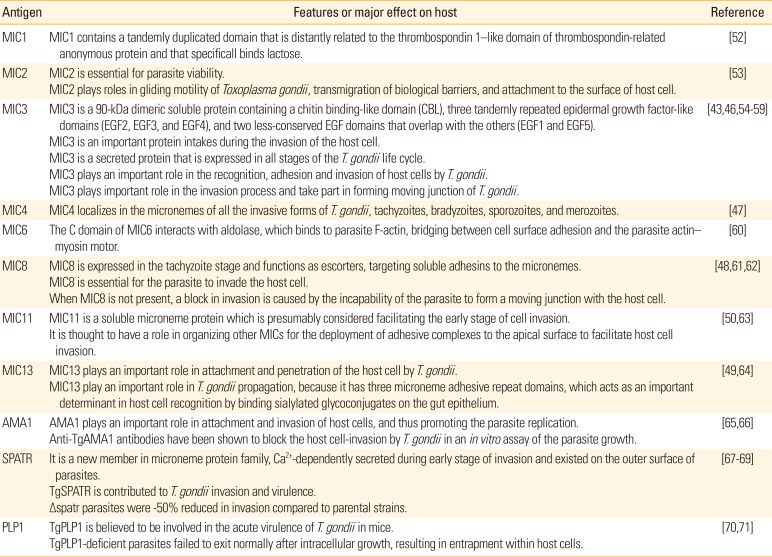
38. Liu Q, Li FC, Zhou CX, Zhu XQ. Research advances in interactions related to Toxoplasma gondii microneme proteins. Exp Parasitol. 2017; 176:89–98. PMID:
28286325.

39. Liu WG, Xu XP, Chen J, Xu QM, Luo SL, Zhu XQ. MIC16 gene represents a potential novel genetic marker for population genetic studies of Toxoplasma gondii. BMC Microbiol. 2016; 16:101. PMID:
27277196.

40. Pinzan CF, Sardinha-Silva A, Almeida F, et al. Vaccination with recombinant microneme proteins confers protection against experimental toxoplasmosis in mice. PLoS One. 2015; 10:e0143087. PMID:
26575028.

41. Kim K. Role of proteases in host cell invasion by Toxoplasma gondii and other Apicomplexa. Acta Trop. 2004; 91:69–81. PMID:
15158690.

42. Carruthers VB, Tomley FM. Microneme proteins in apicomplexans. Subcell Biochem. 2008; 47:33–45. PMID:
18512339.

43. Wang Y, Yin H. Research advances in microneme protein 3 of Toxoplasma gondii. Parasit Vectors. 2015; 8:384. PMID:
26194005.

44. Dowse T, Soldati D. Host cell invasion by the apicomplexans: the significance of microneme protein proteolysis. Curr Opin Microbiol. 2004; 7:388–396. PMID:
15358257.

45. Dautu G, Munyaka B, Carmen G, et al. Toxoplasma gondii: DNA vaccination with genes encoding antigens MIC2, M2AP, AMA1 and BAG1 and evaluation of their immunogenic potential. Exp Parasitol. 2007; 116:273–282. PMID:
17379212.

46. Ismael AB, Sekkai D, Collin C, Bout D, Mevelec MN. The MIC3 gene of Toxoplasma gondii is a novel potent vaccine candidate against toxoplasmosis. Infect Immun. 2003; 71:6222–6228. PMID:
14573640.
47. Wang H, He S, Yao Y, et al. Toxoplasma gondii: protective effect of an intranasal SAG1 and MIC4 DNA vaccine in mice. Exp Parasitol. 2009; 122:226–232. PMID:
19366622.

48. Liu MM, Yuan ZG, Peng GH, et al. Toxoplasma gondii microneme protein 8 (MIC8) is a potential vaccine candidate against toxoplasmosis. Parasitol Res. 2010; 106:1079–1084. PMID:
20177910.

49. Yuan ZG, Ren D, Zhou DH, et al. Evaluation of protective effect of pVAX-TgMIC13 plasmid against acute and chronic Toxoplasma gondii infection in a murine model. Vaccine. 2013; 31:3135–3139. PMID:
23707448.

50. Tao Q, Fang R, Zhang W, et al. Protective immunity induced by a DNA vaccine-encoding Toxoplasma gondii microneme protein 11 against acute toxoplasmosis in BALB/c mice. Parasitol Res. 2013; 112:2871–2877. PMID:
23749087.

51. Li ZY, Chen J, Petersen E, et al. Synergy of mIL-21 and mIL-15 in enhancing DNA vaccine efficacy against acute and chronic Toxoplasma gondii infection in mice. Vaccine. 2014; 32:3058–3065. PMID:
24690150.

52. Lourenco EV, Pereira SR, Faca VM, et al. Toxoplasma gondii micronemal protein MIC1 is a lactose-binding lectin. Glycobiology. 2001; 11:541–547. PMID:
11447133.

53. Brossier F, David Sibley L. Toxoplasma gondii: microneme protein MIC2. Int J Biochem Cell Biol. 2005; 37:2266–2272. PMID:
16084754.

54. Qu D, Han J, Du A. Evaluation of protective effect of multiantigenic DNA vaccine encoding MIC3 and ROP18 antigen segments of Toxoplasma gondii in mice. Parasitol Res. 2013; 112:2593–2599. PMID:
23591483.

55. Fang R, Nie H, Wang Z, et al. Protective immune response in BALB/c mice induced by a suicidal DNA vaccine of the MIC3 gene of Toxoplasma gondii. Vet Parasitol. 2009; 164:134–140. PMID:
19592172.

56. Garcia-Reguet N, Lebrun M, Fourmaux MN, et al. The microneme protein MIC3 of Toxoplasma gondii is a secretory adhesin that binds to both the surface of the host cells and the surface of the parasite. Cell Microbiol. 2000; 2:353–364. PMID:
11207591.

57. Shen B, Sibley LD. The moving junction, a key portal to host cell invasion by apicomplexan parasites. Curr Opin Microbiol. 2012; 15:449–455. PMID:
22445360.

58. Gong P, Cao L, Guo Y, et al. Toxoplasma gondii: Protective immunity induced by a DNA vaccine expressing GRA1 and MIC3 against toxoplasmosis in BALB/c mice. Exp Parasitol. 2016; 166:131–136. PMID:
27059254.

59. Yang D, Liu J, Hao P, et al. MIC3, a novel cross-protective antigen expressed in Toxoplasma gondii and Neospora caninum. Parasitol Res. 2015; 114:3791–3799. PMID:
26141436.

60. Zheng B, He A, Gan M, Li Z, He H, Zhan X. MIC6 associates with aldolase in host cell invasion by Toxoplasma gondii. Parasitol Res. 2009; 105:441–445. PMID:
19308454.

61. Kessler H, Herm-Gotz A, Hegge S, et al. Microneme protein 8: a new essential invasion factor in Toxoplasma gondii. J Cell Sci. 2008; 121(Pt 7):947–956. PMID:
18319299.
62. Meissner M, Reiss M, Viebig N, et al. A family of transmembrane microneme proteins of Toxoplasma gondii contain EGF-like domains and function as escorters. J Cell Sci. 2002; 115:563–574. PMID:
11861763.
63. Harper JM, Zhou XW, Pszenny V, Kafsack BF, Carruthers VB. The novel coccidian micronemal protein MIC11 undergoes proteolytic maturation by sequential cleavage to remove an internal propeptide. Int J Parasitol. 2004; 34:1047–1058. PMID:
15313131.

64. Friedrich N, Santos JM, Liu Y, et al. Members of a novel protein family containing microneme adhesive repeat domains act as sialic acid-binding lectins during host cell invasion by apicomplexan parasites. J Biol Chem. 2010; 285:2064–2076. PMID:
19901027.

65. Hehl AB, Lekutis C, Grigg ME, et al. Toxoplasma gondii homologue of plasmodium apical membrane antigen 1 is involved in invasion of host cells. Infect Immun. 2000; 68:7078–7086. PMID:
11083833.
66. Santos JM, Ferguson DJ, Blackman MJ, Soldati-Favre D. Intramembrane cleavage of AMA1 triggers Toxoplasma to switch from an invasive to a replicative mode. Science. 2011; 331:473–477. PMID:
21205639.
67. Kawase O, Nishikawa Y, Bannai H, Igarashi M, Matsuo T, Xuan X. Characterization of a novel thrombospondin-related protein in Toxoplasma gondii. Parasitol Int. 2010; 59:211–216. PMID:
20144733.

68. Zheng B, Ding J, Chen X, et al. Immuno-efficacy of a T. gondii secreted protein with an altered thrombospondin repeat (TgSPATR) as a novel DNA vaccine candidate against acute toxoplasmosis in BALB/c mice. Front Microbiol. 2017; 8:216. PMID:
28261175.

69. Huynh MH, Boulanger MJ, Carruthers VB. A conserved apicomplexan microneme protein contributes to Toxoplasma gondii invasion and virulence. Infect Immun. 2014; 82:4358–4368. PMID:
25092910.

70. Kafsack BF, Pena JD, Coppens I, Ravindran S, Boothroyd JC, Carruthers VB. Rapid membrane disruption by a perforin-like protein facilitates parasite exit from host cells. Science. 2009; 323:530–533. PMID:
19095897.

71. Yan HK, Yuan ZG, Petersen E, et al. Toxoplasma gondii: protective immunity against experimental toxoplasmosis induced by a DNA vaccine encoding the perforin-like protein 1. Exp Parasitol. 2011; 128:38–43. PMID:
21310148.

72. Li L, Petrovsky N. Molecular mechanisms for enhanced DNA vaccine immunogenicity. Expert Rev Vaccines. 2016; 15:313–329. PMID:
26707950.

73. Doria-Rose NA, Haigwood NL. DNA vaccine strategies: candidates for immune modulation and immunization regimens. Methods. 2003; 31:207–216. PMID:
14511953.

74. Sayles PC, Gibson GW, Johnson LL. B cells are essential for vaccination-induced resistance to virulent Toxoplasma gondii. Infect Immun. 2000; 68:1026–1033. PMID:
10678903.
75. Denkers EY, Butcher BA, Del Rio L, Bennouna S. Neutrophils, dendritic cells and Toxoplasma. Int J Parasitol. 2004; 34:411–421. PMID:
15003500.

76. Denkers EY, Gazzinelli RT. Regulation and function of T-cell-mediated immunity during Toxoplasma gondii infection. Clin Microbiol Rev. 1998; 11:569–588. PMID:
9767056.
77. Suzuki Y, Orellana MA, Schreiber RD, Remington JS. Interferon-gamma: the major mediator of resistance against Toxoplasma gondii. Science. 1988; 240:516–518. PMID:
3128869.
78. Mosmann TR, Moore KW. The role of IL-10 in crossregulation of TH1 and TH2 responses. Immunol Today. 1991; 12:A49–A53. PMID:
1648926.

79. Ghaffarifar F. Strategies of DNA vaccines against toxoplasmosis. Rev Med Microbiol. 2015; 26:88–90.

80. Xue M, He S, Zhang J, Cui Y, Yao Y, Wang H. Comparison of cholera toxin A2/B and murine interleukin-12 as adjuvants of Toxoplasma multi-antigenic SAG1-ROP2 DNA vaccine. Exp Parasitol. 2008; 119:352–357. PMID:
18442818.

81. Liu Q, Wang F, Wang G, et al. Toxoplasma gondii: immune response and protective efficacy induced by ROP16/GRA7 multicomponent DNA vaccine with a genetic adjuvant B7-2. Hum Vaccin Immunother. 2014; 10:184–191. PMID:
24096573.
82. Turin L, Riva F. Toll-like receptor family in domestic animal species. Crit Rev Immunol. 2008; 28:513–538. PMID:
19265507.

83. Greenland JR, Letvin NL. Chemical adjuvants for plasmid DNA vaccines. Vaccine. 2007; 25:3731–3741. PMID:
17350735.

84. Xiang W, Qiong Z, Li-peng L, Kui T, Jian-wu G, Heng-ping S. The location of invasion-related protein MIC3 of Toxoplasma gondii and protective effect of its DNA vaccine in mice. Vet Parasitol. 2009; 166:1–7. PMID:
19800170.

85. Fang R, Feng H, Hu M, et al. Evaluation of immune responses induced by SAG1 and MIC3 vaccine cocktails against Toxoplasma gondii. Vet Parasitol. 2012; 187:140–146. PMID:
22336771.

86. Peng GH, Yuan ZG, Zhou DH, et al. Sequence variation in Toxoplasma gondii MIC4 gene and protective effect of an MIC4 DNA vaccine in a murine model against toxoplasmosis. J Anim Vet Adv. 2010; 9:1463–1468.

87. Peng GH, Yuan ZG, Zhou DH, et al. Toxoplasma gondii microneme protein 6 (MIC6) is a potential vaccine candidate against toxoplasmosis in mice. Vaccine. 2009; 27:6570–6574. PMID:
19720368.

88. Yan HK, Yuan ZG, Song HQ, et al. Vaccination with a DNA vaccine coding for perforin-like protein 1 and MIC6 induces significant protective immunity against Toxoplasma gondii. Clin Vaccine Immunol. 2012; 19:684–689. PMID:
22379063.

89. Beghetto E, Nielsen HV, Del Porto P, et al. A combination of antigenic regions of Toxoplasma gondii microneme proteins induces protective immunity against oral infection with parasite cysts. J Infect Dis. 2005; 191:637–645. PMID:
15655789.
90. Ismael AB, Hedhli D, Cerede O, Lebrun M, Dimier-Poisson I, Mevelec MN. Further analysis of protection induced by the MIC3 DNA vaccine against T. gondii: CD4 and CD8 T cells are the major effectors of the MIC3 DNA vaccine-induced protection, both Lectin-like and EGF-like domains of MIC3 conferred protection. Vaccine. 2009; 27:2959–2966. PMID:
19428907.

91. Peixoto L, Chen F, Harb OS, et al. Integrative genomic approaches highlight a family of parasite-specific kinases that regulate host responses. Cell Host Microbe. 2010; 8:208–218. PMID:
20709297.

92. Boothroyd JC, Dubremetz JF. Kiss and spit: the dual roles of Toxoplasma rhoptries. Nat Rev Microbiol. 2008; 6:79–88. PMID:
18059289.

93. Bradley PJ, Ward C, Cheng SJ, et al. Proteomic analysis of rhoptry organelles reveals many novel constituents for host-parasite interactions in Toxoplasma gondii. J Biol Chem. 2005; 280:34245–34258. PMID:
16002398.

94. Lourenco EV, Bernardes ES, Silva NM, Mineo JR, Panunto-Castelo A, Roque-Barreira MC. Immunization with MIC1 and MIC4 induces protective immunity against Toxoplasma gondii. Microbes Infect. 2006; 8:1244–1251. PMID:
16616574.
95. Qu D, Yu H, Wang S, Cai W, Du A. Induction of protective immunity by multiantigenic DNA vaccine delivered in attenuated Salmonella typhimurium against Toxoplasma gondii infection in mice. Vet Parasitol. 2009; 166:220–227. PMID:
19740610.

96. Wang T, Yin H, Li Y, Zhao L, Sun X, Cong H. Vaccination with recombinant adenovirus expressing multi-stage antigens of Toxoplasma gondii by the mucosal route induces higher systemic cellular and local mucosal immune responses than with other vaccination routes. Parasite. 2017; 24:12. PMID:
28367800.
97. Nie H, Fang R, Xiong BQ, et al. Immunogenicity and protective efficacy of two recombinant pseudorabies viruses expressing Toxoplasma gondii SAG1 and MIC3 proteins. Vet Parasitol. 2011; 181:215–221. PMID:
21632181.

98. Lee SH, Kim AR, Lee DH, Rubino I, Choi HJ, Quan FS. Protection induced by virus-like particles containing Toxoplasma gondii microneme protein 8 against highly virulent RH strain of Toxoplasma gondii infection. PLoS One. 2017; 12:e0175644. PMID:
28406951.

99. Yin H, Zhao L, Wang T, Zhou H, He S, Cong H. A Toxoplasma gondii vaccine encoding multistage antigens in conjunction with ubiquitin confers protective immunity to BALB/c mice against parasite infection. Parasit Vectors. 2015; 8:498. PMID:
26420606.

100. Quan FS, Kim Y, Lee S, et al. Viruslike particle vaccine induces protection against respiratory syncytial virus infection in mice. J Infect Dis. 2011; 204:987–995. PMID:
21881112.

101. Crisci E, Barcena J, Montoya M. Virus-like particles: the new frontier of vaccines for animal viral infections. Vet Immunol Immunopathol. 2012; 148:211–225. PMID:
22705417.

102. Lee DH, Lee SH, Kim AR, Quan FS. Virus-like nanoparticle vaccine confers protection against Toxoplasma gondii. PLoS One. 2016; 11:e0161231. PMID:
27548677.

103. Abdian N, Gholami E, Zahedifard F, Safaee N, Rafati S. Evaluation of DNA/DNA and prime-boost vaccination using LPG3 against Leishmania major infection in susceptible BALB/c mice and its antigenic properties in human leishmaniasis. Exp Parasitol. 2011; 127:627–636. PMID:
21187087.

104. Yu L, Yamagishi J, Zhang S, et al. Protective effect of a prime-boost strategy with plasmid DNA followed by recombinant adenovirus expressing TgAMA1 as vaccines against Toxoplasma gondii infection in mice. Parasitol Int. 2012; 61:481–486. PMID:
22537971.

105. Kardani K, Bolhassani A, Shahbazi S. Prime-boost vaccine strategy against viral infections: mechanisms and benefits. Vaccine. 2016; 34:413–423. PMID:
26691569.

106. Ledgerwood JE, Zephir K, Hu Z, et al. Prime-boost interval matters: a randomized phase 1 study to identify the minimum interval necessary to observe the H5 DNA influenza vaccine priming effect. J Infect Dis. 2013; 208:418–422. PMID:
23633407.

107. Lu S. Heterologous prime-boost vaccination. Curr Opin Immunol. 2009; 21:346–351. PMID:
19500964.

108. Hansson M, Nygren PA, Stahl S. Design and production of recombinant subunit vaccines. Biotechnol Appl Biochem. 2000; 32(Pt 2):95–107. PMID:
11001870.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download