This article has been
cited by other articles in ScienceCentral.
Abstract
Background
The “Tuberculosis Relief Belt Supporting Project (Tuberculosis Patient Management Project for Poverty Groups)” is a national program for socioeconomically vulnerable tuberculosis (TB) patients. We sought to evaluate the clinical and socioeconomic characteristics of poverty-stricken TB patients, and determined the need for relief.
Methods
We examined in-patients with TB, who were supported by this project at the National Medical Center from 2014 to 2015. We retrospectively investigated the patients' socioeconomic status, clinical characteristics, and project expenditures.
Results
Fifty-eight patients were enrolled. Among 55 patients with known income status, 24 (43.6%) had no income. Most patients (80%) lived alone. A total of 48 patients (82.8%) had more than one underlying disease. More than half of the enrolled patients (30 patients, 51.7%) had smear-positive TB. Cavitary disease was found in 38 patients (65.5%). Among the 38 patients with known resistance status, 19 (50%) had drug-resistant TB. In terms of disease severity, 96.6% of the cases had moderate-to-severe disease. A total of 14 patients (26.4%) died during treatment. Nursing expenses were supported for 12 patients (20.7%), with patient transportation costs reimbursed for 35 patients (60%). In terms of treatment expenses for 31 people (53.4%), 93.5% of them were supported by uninsured benefits.
Conclusion
Underlying disease, infectivity, drug resistance, severity, and death occurred frequently in socioeconomically vulnerable patients with TB. Many uninsured treatment costs were not supported by the current government TB programs, and the “Tuberculosis Relief Belt Supporting Project” compensated for these limitations.
Keywords: Poverty, Tuberculosis
Introduction
Tuberculosis (TB) is contagious chronic wasting disease and the leading cause of infection-related deaths worldwide
12. In South Korea, poverty, cramped living spaces, and the limited anti-TB treatment that occurred during and after the Korean War created ideal conditions for the spread of TB
345.
In Korea, notified TB cases have not decreased during the last decade (2001–2010). The number of notified new cases was the highest in 2011 (78.9 cases per 100,000 persons)
6. Since then, new TB notification rates have decreased steadily, with the rate being 63.2 per 100,000 persons in 2015—compared to the rate in 2014, this indicates an 8.1% decrease
6. This positive trend is the result of many national programs. However, despite national TB control efforts, South Korea still ranks the highest in three major indicators—TB incidence, prevalence, and mortality—among the Organization for Economic Co-operation and Development countries, according to a 2015 World Health Organization report
67.
The “Tuberculosis Relief Belt Supporting Project” was devised to compensate for shortcomings of the national TB control projects among poverty-stricken groups. This system connecting four regional public hospitals started in March 2014, with the aim of assisting treatment of socioeconomically vulnerable TB patients. The National Medical Center (NMC) treats patients with severe TB who require surgery or have severe complications. Three regional public hospitals (Seoul Metropolitan Seobuk Hospital, Masan National Tuberculosis Hospital, and Mokpo National Tuberculosis Hospital) mainly treat patients who chronically excrete Mycobacterium bacilli, patients who were admitted for treatment noncompliance, and patients with infectious multi-drug-resistant (MDR) TB. These four hospitals are connected and transfer patients between them, as needed, based on the patient's suitability for each hospital.
Here, we have reviewed the data for NMC inpatients with TB who were part of the Tuberculosis Relief Belt Supporting Project from 2014 to 2015. The first goal of this study was to determine the socioeconomic and clinical characteristics of poor TB patients who needed this project. Secondly, we sought to determine which aspects could not be covered by the government's previous TB programs. Thus, we set out to evaluate whether this project remains required for economically vulnerable TB patients in Korea in the years to come.
Materials and Methods
Sixty-one inpatients who received treatment expenses, nursing expenses, or patient transportation costs from the Tuberculosis Relief Belt Supporting Project at NMC between March 2014 and December 2015 were involved in this study. Of these, two patients were excluded because they were not confirmed to be TB patients. One outpatient was also excluded because of a lack of socioeconomic data. Thus, a total of 58 patients were enrolled in the study. Because there were some missing data for patients, which differed across the variables, the total numbers differ for some variables, and we indicate the relevant total numbers in parentheses in the tables.
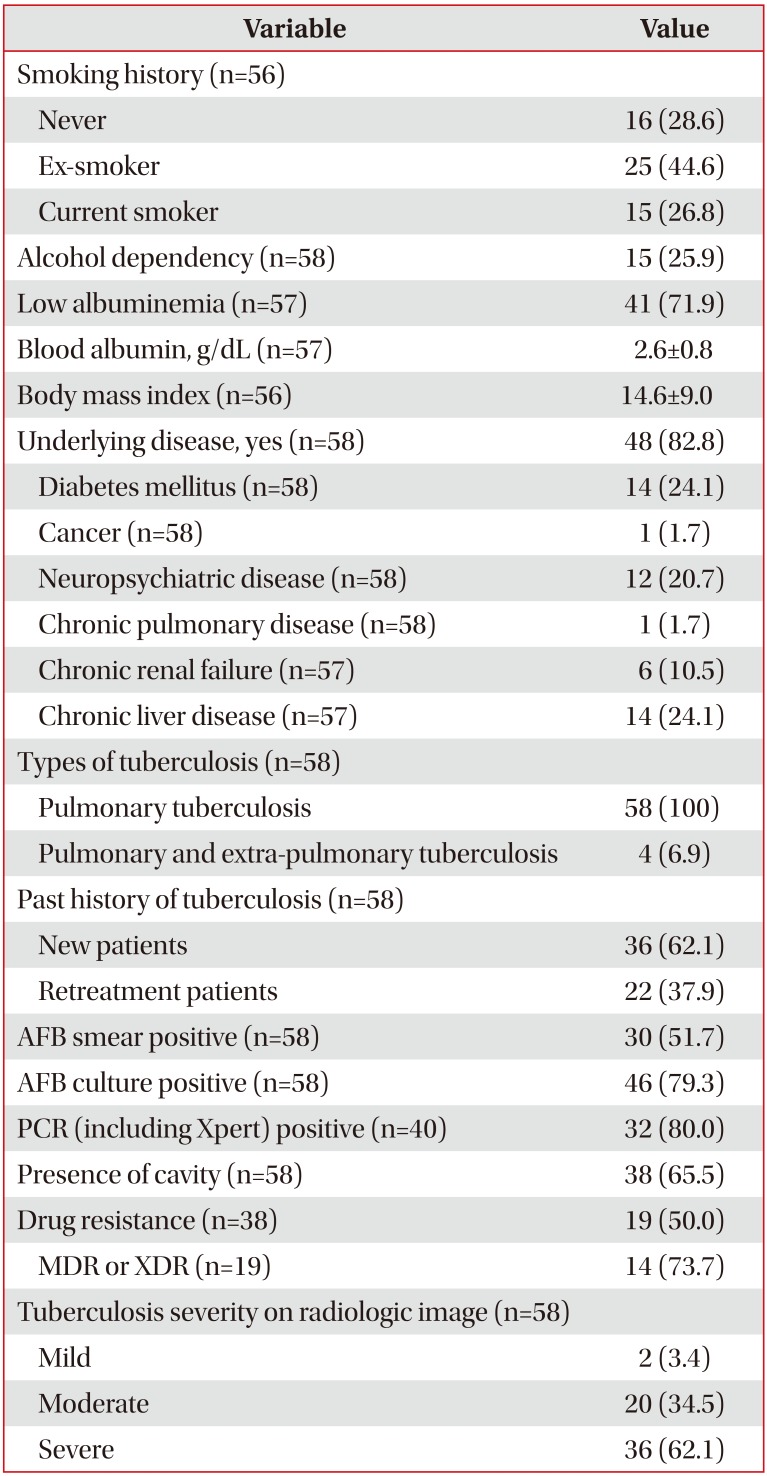
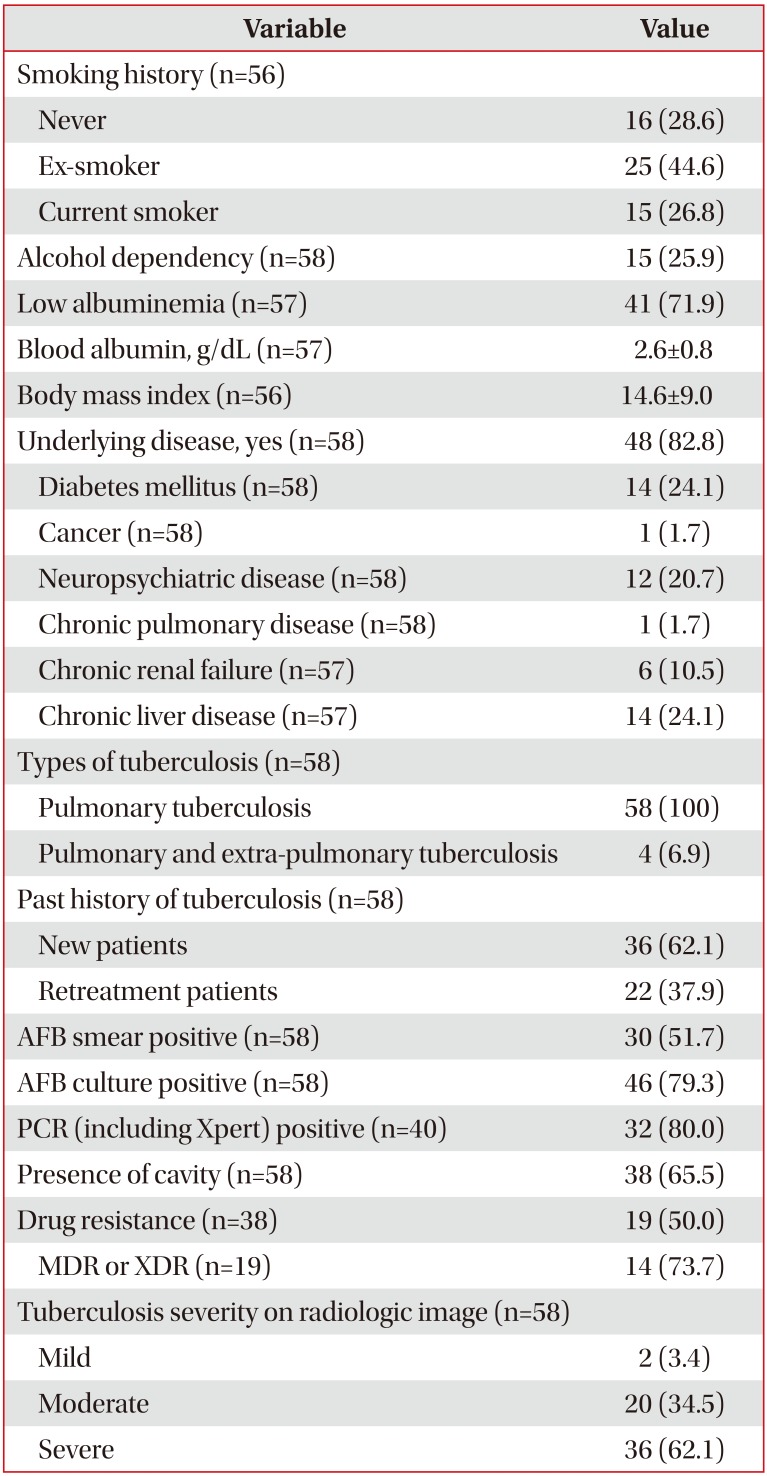
We investigated patients' socioeconomic status, clinical characteristics, and TB treatment outcomes, as well as the details of project expenditures in this study. According to the World Health Organization definitions
1, a new case of TB was a patient who had never been treated for TB or had taken anti-TB drugs for less than 1 month; all others were considered as retreatment cases (
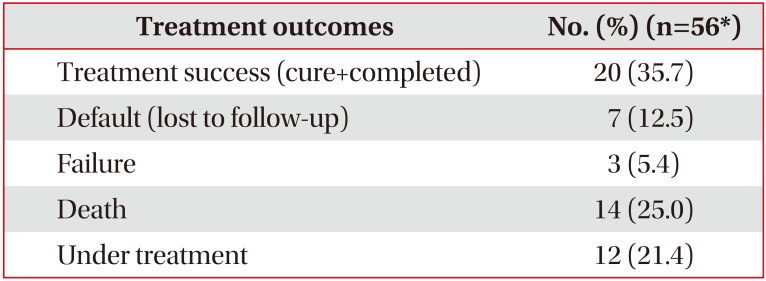
Table 1). Treatment outcomes were defined as follows (
Table 2). A successfully treated individual was defined as a patient who was cured or had completed treatment. “Cured” referred to a patient who was smear- or culture-negative in the last month of treatment and on at least one previous occasion, and “completed” referred to a patient who had completed treatment without evidence of failure, but with no record showing sputum smear or culture results. Lost to follow-up referred to patients who did not start treatment or whose treatment was interrupted for 2 or more consecutive months. “Failed” referred to patients whose sputum smear or culture was positive at month 5 or later during treatment, and “died” referred to patients who died from any cause during treatment.
We collected patient data retrospectively from NMC medical records and project reports from the “Tuberculosis Relief Belt Supporting Project.” We obtained additional data about transferred patients from the Private Public Mixed (PPM) nurses in each hospital.
SPSS version 18 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis, mainly for determining frequencies.
This study was approved by the institutional review board (IRB) of National Medical Center (H-1706-079-001). Informed consent was wavived by the IRB.
Results
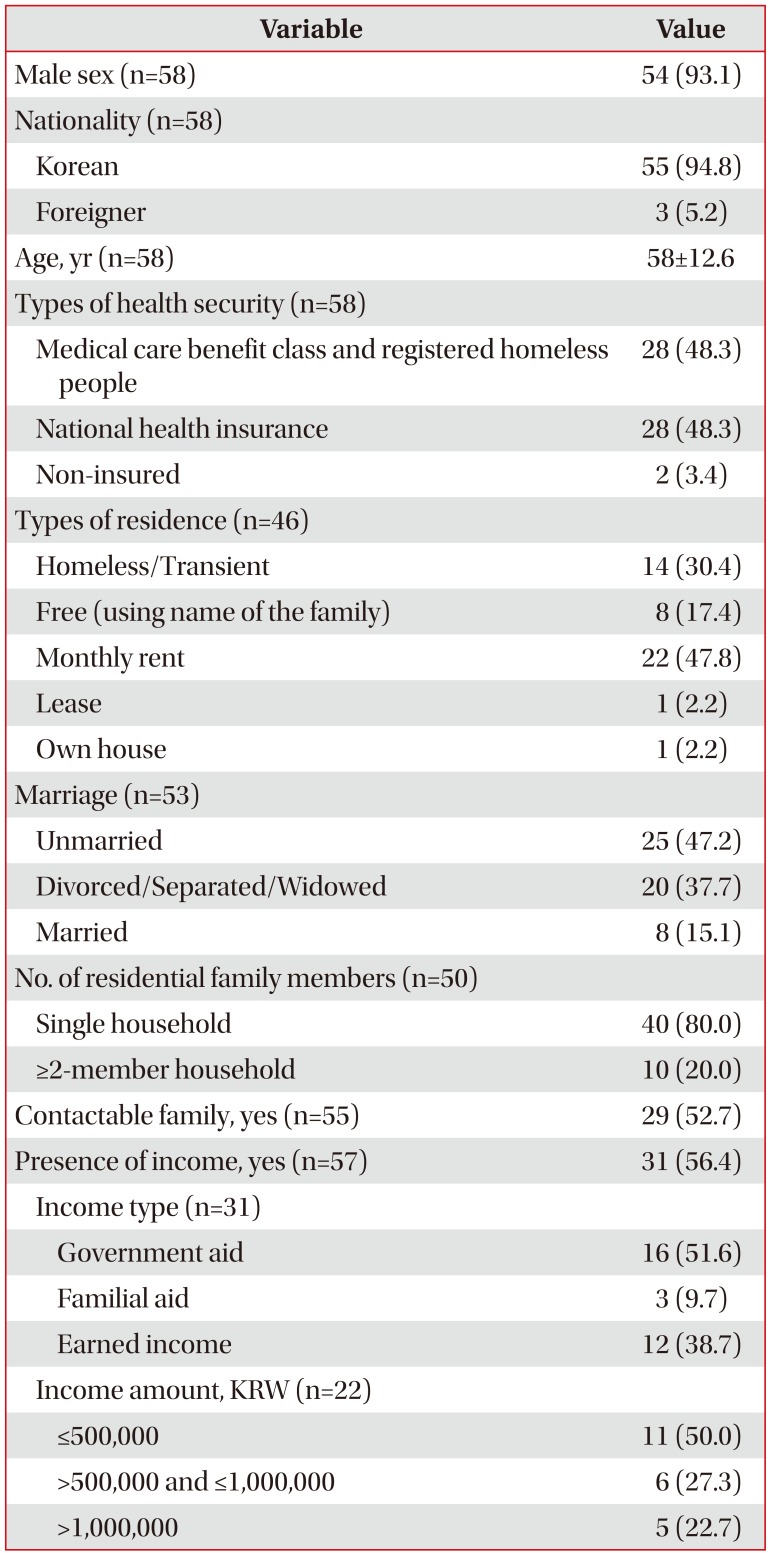
1. Socioeconomic status
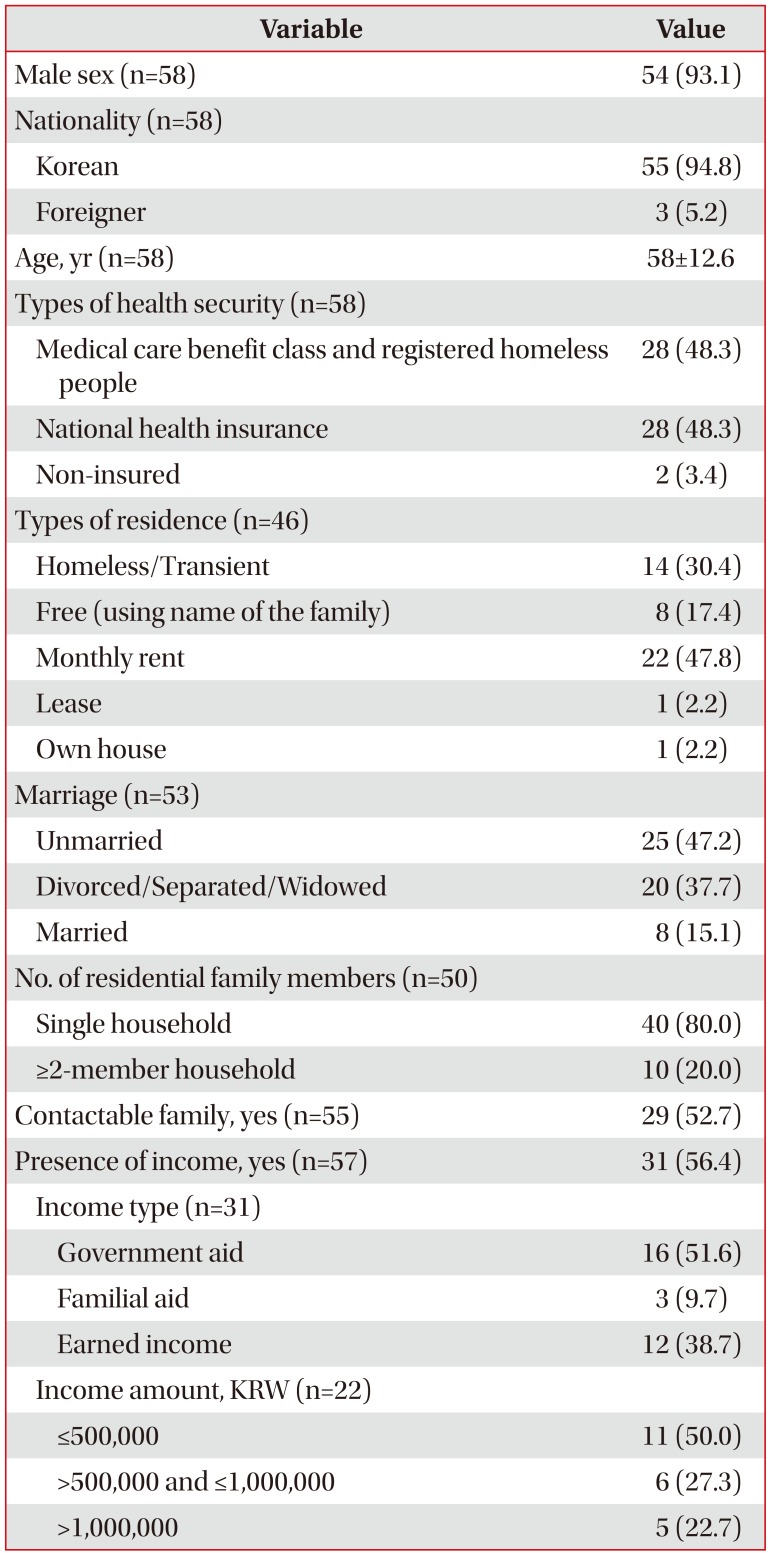
The socioeconomic status of the enrolled patients is reported in
Table 3. A total of 58 patients were enrolled in the study: 54 male patients (93.1%) and four female patients (6.9%). Of these, 55 (94.8%) were Koreans and three (5.2%) were foreigners. The mean age was 58 years (standard deviation [SD], 12.6 years). Most patients (n=33, 56.9%) were in their 40s and 50s. In this study, 28 individuals (48.3%) received medical care benefits and were registered as homeless (people registered as homeless are supported in terms of medical costs by the cities' budget), whereas another 28 individuals (48.3%) had national health insurance (NHI). Twenty-four people (43.6%) had no income. Of the 31 people with an income, 16 (51.6%) received government subsidies as their total income. Only 22 of the 31 people with an income provided accurate information about the amount of their monthly income: 500,000 Korean won or less (11 patients, 50%), greater than 500,000 Korean won, but equal to or less than 1,000,000 Korean won (6 patients, 27.3%), and greater than 1,000,000 Korean won (5 patients, 22.7%). Regarding the income levels of the NHI patients (total number of NHI patients is 28), half (50.0%) of these had no income. Twenty-two people (47.8%) were renting their residences on a monthly basis, whereas 14 people (30.4%) were homeless/transient. Most patients (80%) lived alone, and 29 patients (47.3%) had contactable family members. Most patients were single (unmarried, divorced, separated, or widowed); only eight patients (15.1%) were married (
Table 3).
2. Clinical characteristics
1) Medical history
The medical history and current status of TB patients are shown in
Table 1. Forty patients (71.4%) were smokers (currently or formerly); all of them had smoking histories of more than 10 pack-years. The average albumin level was 2.6 g/dL (SD, 0.86) and the average body mass index (BMI) was 14.6 (SD, 9.04). Forty-eight patients (82.8%) had one or more underlying diseases, with diabetes mellitus (24.1%), chronic liver disease (24.1%), and neuropsychiatric disease (20.7%) being the most common.
2) TB-related characteristics
All patients had pulmonary TB (100%), and four patients (6.9%) had pulmonary TB with extrapulmonary TB. We did not include TB pleurisy concomitant with pulmonary and extrapulmonary TB; instead, these patients were included among the pulmonary TB cases, as many cases of pulmonary TB had varying amounts of pleural effusion, but effusion was not evaluated in most of them. Of the four patients with extrapulmonary TB, three had TB enteritis and one had TB peritonitis.
Thirty-six individuals (62.1%) were newly diagnosed with TB, whereas 22 patients (37.9%) were being retreated because of relapse, treatment failure, or because they had stopped treatment.
More than half of the enrolled patients had smear-positive TB (n=30, 51.7%) or cavitary disease (n=38, 65.5%). Drug-sensitivity tests were performed in 38 patients with positive acid-fast bacilli cultures. Drug-resistant TB was found in 19 individuals (50%); 14 of these cases (73.7%) were multi-drug resistant.
The severity of pulmonary TB was based on chest imaging (chest radiography and chest computerized tomography) according to the National Tuberculosis Association classification
8: 36 (62.1%) were severe cases, 20 (34.5%) were moderate cases, and two (3.4%) were mild cases.
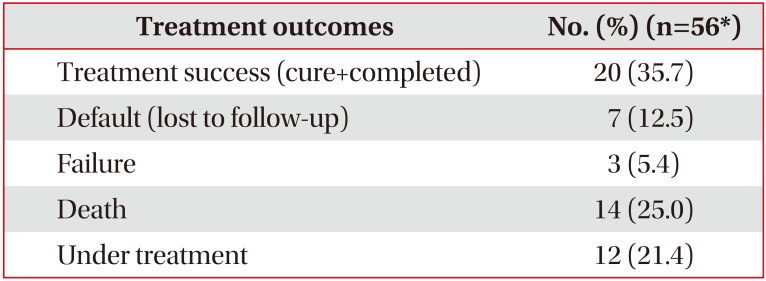
3. TB treatment outcomes
The treatment outcomes were analyzed for 56 patients, including transfer-out patients. Information on the outcomes of two patients was not evaluated due to loss of data. Twenty patients (35.7%) were successfully treated, seven patients (12.5%) stopped treatment (lost to follow-up), three patients (5.4%) showed failed treatment, 14 patients (25.0%) died, and 12 patients (21.4%) were undergoing treatment at the time of the study (
Table 2).
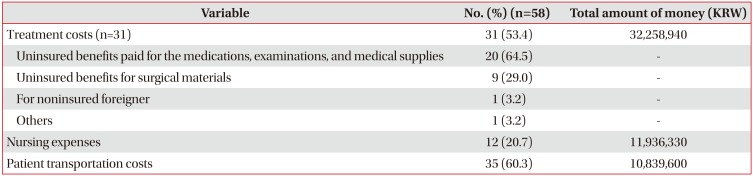
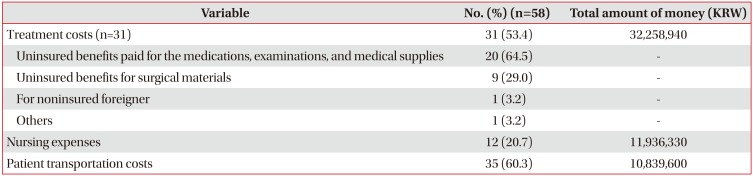
4. Project costs
We were provided with information on the treatment costs for 31 of the 58 patients (53.4%) in this project. Patients paid for 5% of their TB treatment within insured costs during the project period of 2014–2015. This reduction in treatment costs is a result of the national TB treatment support system, and thus their share of treatment cost was fairly low. However, this support applied only to insured benefits; hence, the real needs of poor patients' treatment were related to the uninsured benefits.
We analyzed which uninsured benefits were paid for, as shown in
Table 4. Uninsured benefits paid for the medications, examinations, and medical supplies of 20 patients (64.5%). We classified uninsured benefits for surgical materials as another category, in nine patients (29.0%). A total of 29 individuals (93.5%) were supported by uninsured benefits. One person (3.2%) was a noninsured foreigner who did not qualify for either NHI or medical care benefits; hence, the total costs of his treatments were supported only by this project. Nursing expenses and patient transportation costs were not insured, and thus, 100% of these payments were covered by the patients. The project provided nursing expenses for 12 of 58 patients (20.7%) with severe disease or disability, who had no caretaker. The project also provided patient transportation costs for transfers within the four national hospitals' system for 35 patients (60%) (
Table 4).
Discussion
This study retrospectively analyzed inpatients with TB in the NMCs who were supported by the “Tuberculosis Relief Belt Supporting Project” from 2014 to 2015.
The low average albumin and BMI levels indicate a poor nutritional status. A total of 82.8% of patients had one or more underlying diseases, which influence the incidence and treatment success rate of TB. Smear-positive and cavitary disease rates were greater than 50%. Smear-positive rates were higher in our project than that reported nationally in South Korea for the same period (2014, 37.4%; 2015, 36.4%)
5. In another study about homeless patients in the United States, smear-positive rates were also higher among homeless patients than in the normal population
9. Smear-positive findings and cavitary disease are related to high infectivity; therefore, active treatment and management of these patients are urgently needed. Although MDR TB cases have been decreasing since 2013 as a result of the intensive national TB management programs
6, 50% of the patients in this study had drug-resistant TB and 73.7% of resistant cases were multi-drug resistant. Therefore, special and long-term treatments are needed for TB patients with low socioeconomic status. Chest imaging (chest radiography and chest computerized tomography) of pulmonary TB indicated that 3.4% of cases were mild and 96.6% of cases were moderate or severe. The TB severity of patients was high, and death rate of patients was 25.0%.
Since the establishment of a national tuberculosis program in the 1960s, the prevalence of TB in South Korea has been declining
10. However, the decrease in the rate of TB prevalence has been reducing and the number of MDR TB patients has been increasing since 2000. For these reasons, new national programs were devised in the 2000s. The PPM program started in 2009. The PPM program assists TB patients with treatment education, consultations, and monitoring drug compliance and adverse drug reaction by specially trained nurses in private health centers. The results of this program were successful; patients included in the PPM program showed better treatment success rate for TB than controls (91.6% vs. 71.8%)
511. “Admission orders” (compulsory hospitalization) for noncompliant TB patients and infectious MDR TB patients started in 2011. While some national TB projects, including PPM and “admission orders”, were applicable for noncompliant TB patients, other programs are also required for economically vulnerable TB patients. In many previous studies, TB was more prevalent in low socioeconomic groups
121314. Low socioeconomic status is associated with poor knowledge of TB, high risk of infection and dissemination, and inadequate and/or delayed availability of health care. Poverty also results in poor nutrition and low body weight, which make the immune system more vulnerable to TB
13. Overcrowded residences also increase the risk of disease transmission. Low socioeconomic status is also an important risk factor for nonadherence to TB treatment; therefore, treatment outcomes are poor in these groups
1315. For these reasons, the government has covered much of the medical expenses for TB patients from 2011, and total exemption of the medical expenses being provided by the insured benefits for all TB patients was started in July 2016.
However, despite these national efforts, there are some challenges. First, controlling noncompliant TB patients is difficult. Although intensive efforts have been made to address the issue of noncompliant patients, the success rate for controlling noncompliant TB patients is still not high. It was 56.4% in 2014, 50.0% in 2015, and in the first 3 quarters of 2016, it was 56.6%
16. In addition, the “admission order system” is difficult to implement because of human rights issues. Secondly, there are some limitations in the control of TB in low socioeconomic groups. It is difficult for socioeconomically vulnerable TB patients to receive treatment in the private health sector, because of their unaffordability and the hospitals' refusal to treat such patients.
In Korea, there are two major types of health insurance. The first type is the NHI; this is compulsory insurance for the whole nation and insurance fees differ across income grades. The second type is a medical care benefit; this is medical assistance for the economically vulnerable group, for which most of the medical costs are supported by a government budget. These two types of insurance are only applied to insured costs. Moreover, although there are additional national programs that cover the expense of TB treatments, the national support systems are also limited to insured benefit costs. However considerable costs are incurred for uninsured benefits, including nursing and patient transportation costs, as shown in this study. Therefore, the “Tuberculosis Relief Belt Supporting Project” could cover the costs and medical support that are not addressed by the existing national programs. Individuals with low socioeconomic status are at a higher risk of TB
121314, and treatment is more difficult in these individuals, due to many concomitant underlying diseases, a high rate of infectivity, drug resistance, and disease severity, as also shown in this study (
Table 2). Therefore, national support systems should focus more on economically vulnerable patients to eliminate TB. Moreover, cooperation among the four national hospitals could be helpful for patients who were admitted for treatment noncompliance, by rotating these patients based on the patient's suitability for each hospital. Such a system is important, given the increasing rate of MDR TB
16.
There are limitations in generalizing the characteristics of the socioeconomically vulnerable TB patients in this study. The NMC's role in this project was to treat low-income patients with severe TB who required surgery or had severe complications.
We analyzed only the subjects in this study; there were no controls. We expect to draw more meaningful conclusions from comparative studies between TB patients in a low socioeconomic group and the general population in a future study.
In conclusion, underlying diseases, infectivity, drug resistance, disease severity, and death occurred frequently in socioeconomically vulnerable TB patients who were part of the Tuberculosis Relief Belt Supporting Project in NMC. A large amount of uninsured costs that could not be covered by previous national projects was required in the treatment of these patients. Thus, the Tuberculosis Relief Belt Supporting Project would be needed for economically vulnerable TB patients in Korea for years to come, in order to eliminate TB.
Table 1
Clinical characteristics
|
Variable |
Value |
|
Smoking history (n=56) |
|
|
Never |
16 (28.6) |
|
Ex-smoker |
25 (44.6) |
|
Current smoker |
15 (26.8) |
|
Alcohol dependency (n=58) |
15 (25.9) |
|
Low albuminemia (n=57) |
41 (71.9) |
|
Blood albumin, g/dL (n=57) |
2.6±0.8 |
|
Body mass index (n=56) |
14.6±9.0 |
|
Underlying disease, yes (n=58) |
48 (82.8) |
|
Diabetes mellitus (n=58) |
14 (24.1) |
|
Cancer (n=58) |
1 (1.7) |
|
Neuropsychiatric disease (n=58) |
12 (20.7) |
|
Chronic pulmonary disease (n=58) |
1 (1.7) |
|
Chronic renal failure (n=57) |
6 (10.5) |
|
Chronic liver disease (n=57) |
14 (24.1) |
|
Types of tuberculosis (n=58) |
|
|
Pulmonary tuberculosis |
58 (100) |
|
Pulmonary and extra-pulmonary tuberculosis |
4 (6.9) |
|
Past history of tuberculosis (n=58) |
|
|
New patients |
36 (62.1) |
|
Retreatment patients |
22 (37.9) |
|
AFB smear positive (n=58) |
30 (51.7) |
|
AFB culture positive (n=58) |
46 (79.3) |
|
PCR (including Xpert) positive (n=40) |
32 (80.0) |
|
Presence of cavity (n=58) |
38 (65.5) |
|
Drug resistance (n=38) |
19 (50.0) |
|
MDR or XDR (n=19) |
14 (73.7) |
|
Tuberculosis severity on radiologic image (n=58) |
|
|
Mild |
2 (3.4) |
|
Moderate |
20 (34.5) |
|
Severe |
36 (62.1) |
Table 2
Treatment outcomes
|
Treatment outcomes |
No. (%) (n=56*) |
|
Treatment success (cure+completed) |
20 (35.7) |
|
Default (lost to follow-up) |
7 (12.5) |
|
Failure |
3 (5.4) |
|
Death |
14 (25.0) |
|
Under treatment |
12 (21.4) |
Table 3
Socioeconomic characteristics
|
Variable |
Value |
|
Male sex (n=58) |
54 (93.1) |
|
Nationality (n=58) |
|
|
Korean |
55 (94.8) |
|
Foreigner |
3 (5.2) |
|
Age, yr (n=58) |
58±12.6 |
|
Types of health security (n=58) |
|
|
Medical care benefit class and registered homeless people |
28 (48.3) |
|
National health insurance |
28 (48.3) |
|
Non-insured |
2 (3.4) |
|
Types of residence (n=46) |
|
|
Homeless/Transient |
14 (30.4) |
|
Free (using name of the family) |
8 (17.4) |
|
Monthly rent |
22 (47.8) |
|
Lease |
1 (2.2) |
|
Own house |
1 (2.2) |
|
Marriage (n=53) |
|
|
Unmarried |
25 (47.2) |
|
Divorced/Separated/Widowed |
20 (37.7) |
|
Married |
8 (15.1) |
|
No. of residential family members (n=50) |
|
|
Single household |
40 (80.0) |
|
≥2-member household |
10 (20.0) |
|
Contactable family, yes (n=55) |
29 (52.7) |
|
Presence of income, yes (n=57) |
31 (56.4) |
|
Income type (n=31) |
|
|
Government aid |
16 (51.6) |
|
Familial aid |
3 (9.7) |
|
Earned income |
12 (38.7) |
|
Income amount, KRW (n=22) |
|
|
≤500,000 |
11 (50.0) |
|
>500,000 and ≤1,000,000 |
6 (27.3) |
|
>1,000,000 |
5 (22.7) |
Table 4
Details of project costs
|
Variable |
No. (%) (n=58) |
Total amount of money (KRW) |
|
Treatment costs (n=31) |
31 (53.4) |
32,258,940 |
|
Uninsured benefits paid for the medications, examinations, and medical supplies |
20 (64.5) |
- |
|
Uninsured benefits for surgical materials |
9 (29.0) |
- |
|
For noninsured foreigner |
1 (3.2) |
- |
|
Others |
1 (3.2) |
- |
|
Nursing expenses |
12 (20.7) |
11,936,330 |
|
Patient transportation costs |
35 (60.3) |
10,839,600 |




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download