Abstract
Background
Eosinophilia is well recognized in specific conditions. The objective of the present study was to determine clinico-radiologic characteristics of eosinophilia and changes in prevalence over 10 years in recipients of private health screening program at a tertiary hospital in Korea.
Methods
Data of private health screening program recipients at the health promotion center of Chung-Ang University Hospital from 2004 to 2013 were collected. Health-related questionnaires and laboratory findings of private health screening program with possible relation with eosinophilia were reviewed. Results of enzyme-linked immunosorbent assay (ELISA) for parasite, chest computed tomography, and pulmonary function test were also reviewed.
Results
The cumulative prevalence of eosinophilia was 4.0% (1,963 of 48,928). Prevalence of eosinophilia showed a decreased trend from 2004 to 2013. Most cases (96.6%) had mild degree of eosinophilia. Eosinophilic subjects were older and male-predominant. They showed lower levels of forced expiratory volume in 1 second (FEV1%), forced vital capacity (FVC%), and FEV1/FVC than those without eosinophilia. Eosinophilic subjects showed higher positive rate for common parasite in ELISA than those without eosinophilia. On radiologic findings, consolidation and ground glass opacities were positively associated with the degree of eosinophilia. When eosinophil was classified based on severity, statistically significant correlation between the severity of eosinophil and radiologic abnormalities was found.
The typical percentage of blood eosinophils in healthy individuals is less than 5%1. Absolute eosinophil count can be determined by multiplying total white blood cell count by the percentage of eosinophils. Eosinophilia is considered when absolute eosinophil count exceeds 500/µL in peripheral blood. Eosinophilia can be categorized as mild (absolute eosinophil count ranges from 500/µL to 1,500/µL), moderate (absolute eosinophil count ranges from 1,500/µL to 5,000/µL), or severe (absolute eosinophil count >5,000/µL)2. Peripheral blood eosinophilia can be caused by parasitic infections, allergy, drug reactions, leukemia, and non-hematologic cancers1.
The urgency for the evaluation of eosinophilia depends on the presence and the degree of tissue and/or organ involvement. There are many reports of acutely ill patients with extremely high eosinophil count or outpatients with signs of organ involvement3456. However, eosinophilia might be discovered as an incidental finding based on complete blood count in an otherwise healthy individual. Because eosinophilia in such situation is rarely reported, collective features of incidental eosinophilia have not been clearly delineated.
Our health screening program is not a national health screening program. It is a private health screening program. It is performed for subjects who want to take a health check. Such private health screening program in our medical institutes almost always includes complete blood count. Our hospital health screening program also contains many other useful tests such as stool parasite exam, blood chemistry, urinalysis, ultrasound of upper abdomen, chest X-ray, and chest computed tomography (CT). It can provide information regarding the prevalence of eosinophilia in healthy population. It is also helpful in defining the cause of eosinophilia.
Changes in prevalence of eosinophilia over time in healthy population have rarely been reported. Therefore, the objective of the present study was to evaluate the prevalence of eosinophilia among recipients of private health screening program at the health promotion center of Chung-Ang University Hospital from 2004 to 2013. Clinical characteristics of those with eosinophilia were determined. Annual trend of prevalence and severity of eosinophilia were evaluated. Patterns of eosinophilia according to gender, age, and radiologic findings were also analyzed.
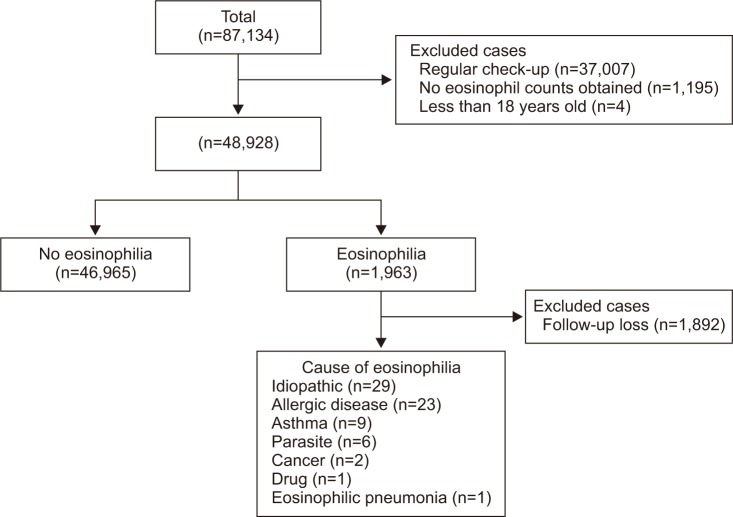
Ten years of data of health screening program recipients at the health promotion center of Chung-Ang University Hospital from 2004 to 2013 were reviewed. From 2004 to 2013, there were 87,134 health screening cases at the health promotion center of Chung-Ang University Hospital. A total of 37,077 cases were excluded because they were taken by the same recipients for regular annual check-up after the initial visit. In addition, 1,195 cases were excluded because eosinophil percentage was not reported. Four cases were excluded due to young age (<18 years). Therefore, a total of 48,928 subjects were included for analysis of this study (Figure 1).
Health-related questionnaires which contained demographic data were specifically reviewed. Laboratory findings of health screening program with possible relations with eosinophilia such as stool parasite exam, blood chemistry, and spirometry data were evaluated. Radiologic findings were retrospectively reviewed by one chest radiologist. One pulmonologist reviewed the final report of radiologist. Most CT scans were low dose chest CT, the most frequently used scan to screen lung cancer in private health screening program.
Eosinophilia was defined when absolute eosinophil count exceeded 500/µL in peripheral blood. This study protocol was approved by the Institutional Review Board of Chung-Ang University Hospital (approval No. C2014146 (1342)) and documentation of informed consent was waived.
All statistical analyses were performed using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA). Continuous variables were expressed as means and standard deviations of the means. Categorical variables were presented as numbers and percentages. Differences in values between those with eosinophilia and those without eosinophilia were evaluated using chi-square test and Student's t test. Statistical significant change in annual prevalence of eosinophilia during the observed period was evaluated by binary logistic regression after adjusting for age and sex. It was expressed as odds ratio (OR) with 95% confidence interval (CI). A p-value of less than 0.05 was considered statistically significant.
Among 46,928 cases, 1,963 (4.0%) had eosinophilia (absolute eosinophil count ≥500/µL). Mild eosinophilia (absolute eosinophil count of 500/µL to 1,500/µL) was found in most cases (n=1,893, 96.5%). Moderate eosinophilia (absolute eosinophil count of 1,500/µL to 5,000/µL) was found in 68 cases (3.5%) while severe eosinophilia (≥5,000/µL) was only found in 1 case (0.1%) in subjects with eosinophilia.
Clinical characteristics were assessed for all study subjects according to the presence or absence of eosinophilia (Table 1). Subjects with eosinophilia were older (p<0.001) than those without eosinophilia. They showed higher proportion of males (76.8% vs. 55.7%, p<0.001). Subjects with eosinophilia also had higher levels of body mass index, leukocyte count, aspartate aminotransferase, and alanine aminotransferase than those without eosinophilia after adjusting for age and sex (all p<0.01). Subjects with eosinophilia showed lower levels of forced expiratory volume at one second (FEV1), forced vital capacity (FVC), and FEV1/FVC percentage than those without eosinophilia after adjusting for age and sex (all p<0.01).
The prevalence of eosinophilia increased with advancing age (p for trend <0.001) (Figure 2A). After adjusting for sex, the OR of eosinophilia in 10-year-old was 1.098 (95% CI, 1.053–1.146; p<0.001). Regarding gender difference, male subjects showed significantly higher trend in the prevalence of eosinophilia with advancing age (p for trend <0.001; OR, 1.114; 95% CI, 1.060–1.170) (Figure 2B). However, such significance was not detected in females (p for trend=0.255).
Annual prevalence of eosinophilia decreased during the observed period (p for trend <0.001) (Figure 3A). After adjusting for age and sex, OR of eosinophilia in 1 year was 0.942 (95% CI, 0.926–0.958) (p<0.001). In both males and females, annual prevalence of eosinophilia decreased during the observed period (both p for trend <0.001) (Figure 3B). After adjusting for age, annual prevalence of eosinophilia decreased (in males: OR, 0.942; 95% CI, 0.924–0.960; p<0.001; in females: OR, 0.941; 95% CI, 0.909–0.974; p=0.001). In subjects with eosinophilia, the proportion of subjects with eosinophil count ≥2,000/µL decreased and that with eosinophil count ≥500 but <2,000/µL increased during the observed period (p for trend=0.009) (Figure 4).
Stool exam for parasite egg was performed for 30,109 non-eosinophilic subjects (test performance rate, 64.2%) and 1,285 eosinophilic subjects (test performance rate, 65.5%). Positive rate was 0.00% (9 of 30,109) in non-eosinophilic subjects and 0.1% (1 of 1,285) in eosinophilic subjects (p=0.342). In addition, enzyme-linked immunosorbent assay (ELISA) tests for four most common parasites (Clonorchis sinensis, Paragonimus westermani, Cysticercus, and Sparganum) were performed for 353 subjects (295 tests in 46,965 non-eosinophilic subjects and 58 tests in 1,963 eosinophilic subjects). Among total patients, only 32 patients (20 non-eosinophilic subjects and 12 eosinophilic subjects) were positive based on ELISA. Of these 32 ELISA positive patients, 24 (75.0%) were males. They had mild eosinophilia (mean eosinophil count, 659.93±972.67). Their mean age was 54.66±10.74 years. Of these 32 ELISA positive cases, nine (28.1%) were positive for C. sinensis, seven (21.9%) were positive for P. westermani, seven (21.9%) were positive for Cysticercus, and nine (28.1%) were positive for Sparganum. In the total population, the positivity rate of parasite based on ELISA gradually increased with advancing age: 0% in the 20s; 4% in the 30s; 4.5% in the 40s; 11.9% in the 50s; and 15.8% in the 60s (p=0.002). The rate of eosinophilia also gradually increased with advancing age: 0% in the 20s; 25% in the 30s; 14.3% in the 40s; 20.8% in the 50s; and 63.6% in the 60s (p=0.039).
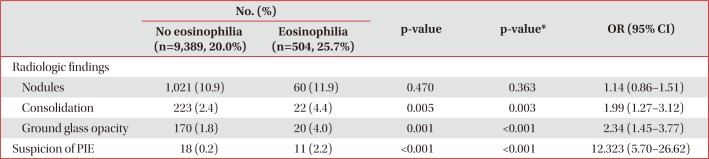
Of 46,928 subjects, a total of 9,893 subjects (20.2%) without eosinophilia and 504 subjects (1.0%) with eosinophilia underwent chest CT. Their radiologic findings were assessed regarding the presence of nodules, consolidation, and ground glass opacities on chest CT. Among them, consolidation (OR, 1.99; 95% CI, 1.27–3.12; p=0.003) and ground glass opacities (OR, 2.34; 95% CI, 1.45–3.77; p<0.001) were more frequently found in subjects with eosinophilia compared to those without eosinophilia. In addition, subjects with eosinophilia were more likely to have suspicion of pulmonary infiltrate with eosinophilia (OR, 12.32; 95% CI, 5.70–26.62; p<0.001) (Table 2). When eosinophil was classified based on severity, statistically significant correlation between the severity of eosinophilia and radiologic abnormalities was found (Figure 5).
In the present study, the prevalence of eosinophilia was evaluated using 10 years of data from a health promotion center of a tertiary hospital. The prevalence of eosinophilia was 4.0%. Eosinophilic subjects were older and male-predominant. Eosinophilia was mild in most cases. Subjects with eosinophilia had higher levels of body mass index, leukocyte count, and liver enzyme but lower lung function than those without eosinophilia. The prevalence of eosinophilia increased with advancing age. Interestingly, this relationship was valid only in male subjects in sub-analysis for gender difference. Of note, annual prevalence and severity of eosinophilia decreased from 2004 to 2013. As expected, eosinophilic subjects showed higher positive rates for common parasites based on ELISA, but not statistically significant. On radiologic findings, subjects with eosinophilia were more likely to have pulmonary abnormalities than those without eosinophilia.
Eosinophil is a multifunctional leukocyte that contributes to various inflammatory processes, including parasitic helminth, bacterial and viral infections, pathogenesis of tumor immunity, allergic disease, and drug-induced reaction78910. However, the prevalence and clinical implication of eosinophilia in healthy population have been rarely reported. Our results revealed that the prevalence of eosinophilia was 4% among health screening program recipients in a tertiary hospital of South Korea. Eosinophilic subjects showed male predominance. The reason for male predominance is currently unclear. It has been suggested that an overwhelming majority of males are affected by clonal eosinophilia11. Because eosinophilia is associated with smoking, higher smoking or alcohol rate of male than that of female might be one of the causes of eosinophilia1213. Eating habits can be one important factor. Usually, men have greater opportunities to consume herb medicines, raw fish, and beef tartare than women. Therefore, they are exposed to more risk factors for parasite infections. Most (96.6%) eosinophilia cases were mild. Severe eosinophilia exceeding 5,000/µL was extremely rare (0.1%).
It is well known that allergic diseases and helminthic infections are two major causes of eosinophilia. However, it is difficult to determine which one might have contributed more to the prevalence of eosinophilia in the present study. The prevalence of asthma has been increasing in Korean population as in many other industrialized countries1415. On the other hand, parasitic infections have continually decreased among Korean population16. In our study, no eosinophilic subject with ELISA positivity was found in those under 30s whereas 63.6% eosinophilic subjects in those over 60s were found to have ELISA positivity. Of course, the decrease of ELISA positivity cannot directly explain the all cause of decline in eosinophilia. Considering results from other studies, we can postulate with caution that the decreasing trend of parasitic infections might have outpaced the increasing trend of allergic diseases. However, further study is needed to support this hypothesis.
In our study, subjects with eosinophilia had lower levels of predicted FEV1, FVC, and FEV1/FVC. Their low pulmonary function indicates that eosinophilia might be related to airway obstruction and inflammation. Several community-based population studies have reported that peripheral eosinophilia is associated with lower FEV1%, providing evidence that eosinophilia is a disease involving the small airway1718. Another study has also demonstrated that blood eosinophil count is a useful biomarker to identify the severity of eosinophilic asthma19. In addition, eosinophila was associated with high body mass index in our study. Eosinophilia in this group might be due to the fact that eosinophil count is associated with metabolic and pulmonary traits20.
Ground glass opacities and consolidation on chest CT were more frequently found in eosinophilic patients than those in subjects without eosinophilia. The percentage of pulmonary infiltration in the eosinophilic group was also higher compared to that in non-eosinophilic subjects. It has been reported that the degree of eosinophilia is rarely helpful for identifying the cause except hematologic malignancy21. However, our results showed that the severity of eosinophilia was associated with radiologic abnormalities. Because lungs are the most frequently involved organ in eosinophilic subjects, the importance of pulmonary function test and CT should be highlighted, especially for subjects with high eosinophil count22.
Our study has some limitations. First, because a limited number of subjects were referred for clinical history, diagnostic evaluation for etiologies of eosinophilia were not specifically delineated for most cases of eosinophilia in the present study. Second, we evaluated the initial data of health screening program. Therefore, clinical course of eosinophilic subjects was not included in the analysis. Last, chest CT and ELISA test were not checked for all subjects. Since the parasite ELISA test was performed only on a part of the subjects, the difference in the parasite positivity between subjects with eosinophilia and those without eosinophilia may not be significant.
Nonetheless, the present study provided information regarding the prevalence of eosinophilia in a relatively large Korean population. Eosinophilia in healthy Korean population was not common. It was usually found with mild degree. The prevalence of eosinophilia tend to decrease from 2004 to 2013. In addition, eosinophilic patients showed higher ELISA positivity, lower pulmonary function, and more radiologic abnormalities than subjects without eosinophilia. Because eosinophilia is associated with various causes and abnormal findings, further diagnostic tests are needed for eosinophilic patients.
References
1. Tefferi A. Blood eosinophilia: a new paradigm in disease classification, diagnosis, and treatment. Mayo Clin Proc. 2005; 80:75–83. PMID: 15667033.

2. Helbig G. Advances in the diagnosis and treatment of eosinophilia. Curr Opin Hematol. 2014; 21:3–7. PMID: 24322486.

3. Crane MM, Chang CM, Kobayashi MG, Weller PF. Incidence of myeloproliferative hypereosinophilic syndrome in the United States and an estimate of all hypereosinophilic syndrome incidence. J Allergy Clin Immunol. 2010; 126:179–181. PMID: 20639012.

4. Mejia R, Nutman TB. Evaluation and differential diagnosis of marked, persistent eosinophilia. Semin Hematol. 2012; 49:149–159. PMID: 22449625.

5. Dulohery MM, Patel RR, Schneider F, Ryu JH. Lung involvement in hypereosinophilic syndromes. Respir Med. 2011; 105:114–121. PMID: 21036585.

6. Sluzevich JC, Sheth AP, Lucky AW. Persistent eosinophilia as a presenting sign of scabies in patients with disorders of keratinization. Arch Dermatol. 2007; 143:670–673.

7. Schleich FN, Chevremont A, Paulus V, Henket M, Manise M, Seidel L, et al. Importance of concomitant local and systemic eosinophilia in uncontrolled asthma. Eur Respir J. 2014; 44:97–108. PMID: 24525441.

8. Vu Thi N, Pozio E, Van De N, Praet N, Pezzotti P, Gabriel S, et al. Anti-Trichinella IgG in ethnic minorities living in Trichinella-endemic areas in northwest Vietnam: study of the predictive value of selected clinical signs and symptoms for the diagnosis of trichinellosis. Acta Trop. 2014; 139:93–98. PMID: 25076109.
9. Naldi L, Crotti S. Epidemiology of cutaneous drug-induced reactions. G Ital Dermatol Venereol. 2014; 149:207–218. PMID: 24819642.
10. Hogan SP, Rosenberg HF, Moqbel R, Phipps S, Foster PS, Lacy P, et al. Eosinophils: biological properties and role in health and disease. Clin Exp Allergy. 2008; 38:709–750. PMID: 18384431.

11. Gotlib J. World Health Organization-defined eosinophilic disorders: 2011 update on diagnosis, risk stratification, and management. Am J Hematol. 2011; 86:677–688. PMID: 21761433.

12. Kauffmann F, Neukirch F, Korobaeff M, Marne MJ, Claude JR, Lellouch J. Eosinophils, smoking, and lung function: an epidemiologic survey among 912 working men. Am Rev Respir Dis. 1986; 134:1172–1175. PMID: 3491554.
13. Kim HS, Jin Y, Choi MH, Kim JH, Lee YH, Yoon CH, et al. Significance of serum antibody test for toxocariasis in healthy healthcare examinees with eosinophilia in Seoul and Gyeongsangnam-do, Korea. J Korean Med Sci. 2014; 29:1618–1625. PMID: 25469060.

14. Hong SJ, Lee MS, Sohn MH, Shim JY, Han YS, Park KS, et al. Self-reported prevalence and risk factors of asthma among Korean adolescents: 5-year follow-up study, 1995-2000. Clin Exp Allergy. 2004; 34:1556–1562. PMID: 15479270.

15. Kim YY. Past, present, and future of allergy in Korea. Allergy Asthma Immunol Res. 2010; 2:155–164. PMID: 20592913.

16. Hong ST, Chai JY, Choi MH, Huh S, Rim HJ, Lee SH. A successful experience of soil-transmitted helminth control in the Republic of Korea. Korean J Parasitol. 2006; 44:177–185. PMID: 16969055.

17. Mensinga TT, Schouten JP, Weiss ST, Van der Lende R. Relationship of skin test reactivity and eosinophilia to level of pulmonary function in a community-based population study. Am Rev Respir Dis. 1992; 146:638–643. PMID: 1519840.

18. Ulrik CS. Eosinophils and pulmonary function: an epidemiologic study of adolescents and young adults. Ann Allergy Asthma Immunol. 1998; 80:487–493. PMID: 9647272.

19. Katz LE, Gleich GJ, Hartley BF, Yancey SW, Ortega HG. Blood eosinophil count is a useful biomarker to identify patients with severe eosinophilic asthma. Ann Am Thorac Soc. 2014; 11:531–536. PMID: 24606022.

20. LifeLines Cohort Study. Amini M, Bashirova D, Prins BP, Corpeleijn E, Bruinenberg M, et al. Eosinophil count is a common factor for complex metabolic and pulmonary traits and diseases: the LifeLines Cohort Study. PLoS One. 2016; 11:e0168480. PMID: 27978545.

21. Andersen CL, Siersma VD, Hasselbalch HC, Lindegaard H, Vestergaard H, Felding P, et al. Eosinophilia in routine blood samples and the subsequent risk of hematological malignancies and death. Am J Hematol. 2013; 88:843–847. PMID: 23765950.

22. Sade K, Mysels A, Levo Y, Kivity S. Eosinophilia: a study of 100 hospitalized patients. Eur J Intern Med. 2007; 18:196–201. PMID: 17449391.

Figure 2
The prevalence of eosinophilia according to age and sex. (A) The prevalence of eosinophilia according to age. The prevalence of eosinophilia increased with advancing age (p<0.001). (B) The increasing trend in the prevalence of eosinophilia was significant only in male subjects.
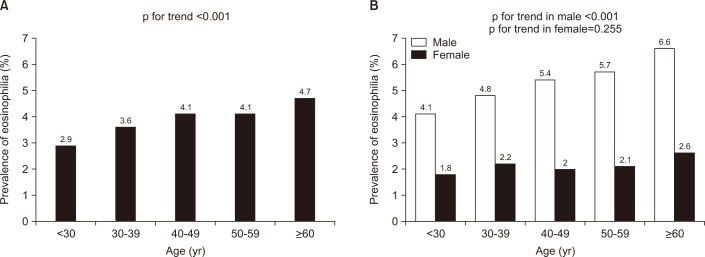
Figure 3
Annual prevalence of eosinophilia from 2004 to 2013. (A) In all subjects. (B) In males and females. p-value was adjusted for age and sex.
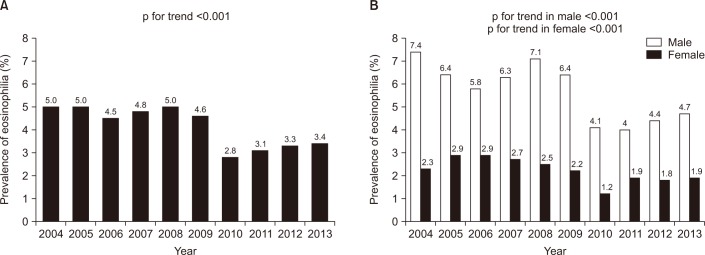
Figure 4
Changes in the distribution of severity of eosinophilia over time. The proportion of eosinophil count ≥2,000/µL decreased between 2004 and 2013.
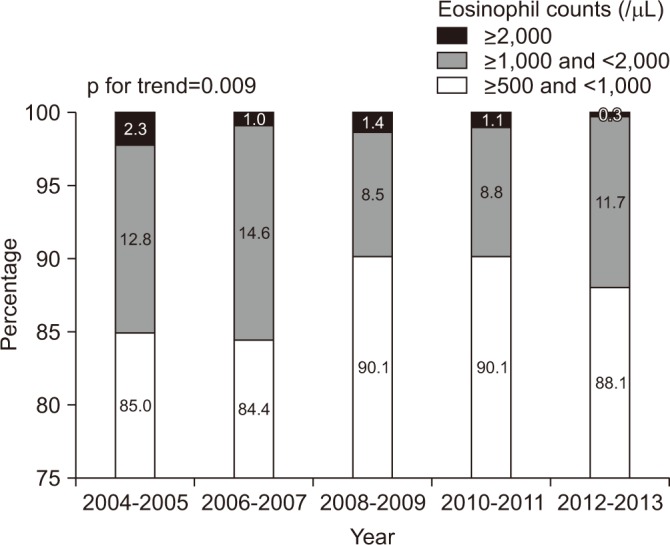
Figure 5
Correlation between the severity of eosinophil and radiologic abnormalities. Consolidation, ground glass opacities, and suspicion of pulmonary infiltrate with eosinophilia (PIE) were frequently detected in subjects with eosinophilia.
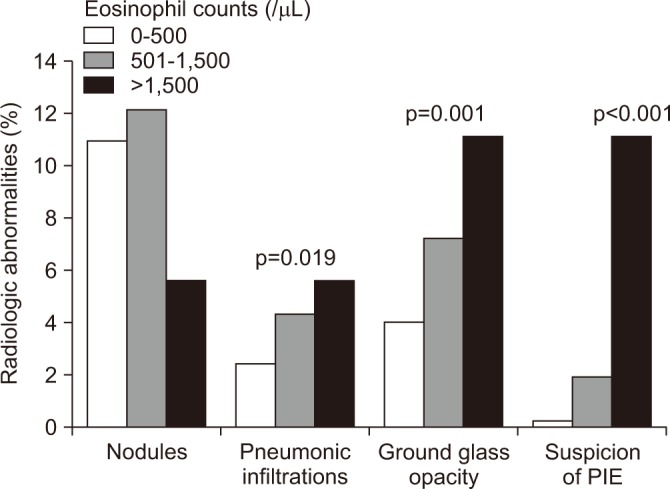
Table 1
Demographic and laboratory data of subjects with and without eosinophilia
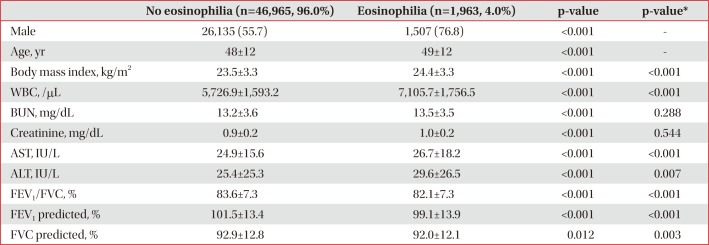
Table 2
Radiologic manifestation on low dose chest computed tomography according to presence or absence of eosinophilia




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download