Abstract
Background
Proper education regarding inhaler usage and optimal management of chronic obstructive pulmonary disease (COPD) is essential for effectively treating patients with COPD. This study was conducted to evaluate the effects of a comprehensive education program including inhaler training and COPD management.
Methods
We enlisted 127 patients with COPD on an outpatient basis at 43 private clinics in Korea. The patients were educated on inhaler usage and disease management for three visits across 2 weeks. Physicians and patients were administered a COPD assessment test (CAT) and questionnaires about the correct usage of inhalers and management of COPD before commencement of this program and after their third visit.
Results
The outcomes of 127 COPD patients were analyzed. CAT scores (19.6±12.5 vs. 15.1±12.3) improved significantly after this program (p<0.05). Patients with improved CAT scores of 4 points or more had a better understanding of COPD management and the correct technique for using inhalers than those who did not have improved CAT scores (p<0.05).
Morbidity and mortality by chronic obstructive pulmonary disease (COPD) is increasing worldwide and Korean survey in 2008 detected 13.4% of COPD among subjects older than 40 years12. Comprehensive care including inhalation therapy and disease education for self management is a cornerstone in the management of COPD134. However, previous studies showed that COPD patients were not using inhalers as prescribed or correctly567. Correct usage of inhalers is reported to be related to patients' knowledge about disease process, educational status, age, gender, formal training, etc.5689. It has been reported that inadequate inhalation technique and poor adherence to inhaled medication in COPD are associated with poor clinical outcomes such as increased hospitalization and high mortality1011. Even self-management interventions in patients with COPD are associated with improved health-related quality of life, a reduction in hospital admissions, and improvement in dyspnea4.
Recently, comprehensive educational program of COPD management including smoking cessation, nutritional support, exercise, vaccination, co-morbidity evaluation, acute exacerbation, and inhaler training was developed by Korean Academy of Tuberculosis and Respiratory Disease12. We implemented this program for COPD patients in a primary care setting and evaluated the efficacy of this comprehensive education program comparing clinical markers before and after this program.
From August 2014 to April 2016, we enlisted 285 patients with asthma or COPD on an outpatient basis who volunteered to be enrolled, and primary physicians of 43 private clinics from seven provinces (Seoul, Chungcheongbuk-do, Chungcheongnam-do, Gyeonggi-do, Gangwon-do, Jeollabuk-do, Jeollanam-do, Jeju-do) throughout Korea participated in this study. We selected four to five primary clinics from each province to make our data representative of general asthma or COPD population of Korea. Among the total group, 127 patients with COPD were selected for the analysis.
Patients were diagnosed as COPD based on the primary physician's clinical judgment according to the following criteria: (1) 40 years or older, (2) forced expiratory volume in 1 second (FEV1) to forced expiratory volume in 6 seconds (FEV6) <0.73, (3) no evidence of malignant cancer, severe kidney or heart disease, transplanted organ for any lesion, bronchiectasis, sequelae of tuberculosis, or pregnancy1314.
The comprehensive educational program developed by Korean Academy of Tuberculosis and Respiratory Disease consisted of inhaler training, an action plan for emergency situation focusing on acute exacerbation of COPD, and management of COPD concerning smoking cessation, nutritional support, exercise, vaccination, and comorbidities12.
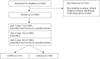
This prospective study was performed to evaluate a 1-month comprehensive educational program. This study enrolled subjects who had been visiting each primary clinic over 1 year or more onto the education program. Considering the reality of primary care setting, we designed this study consisting of three consecutive educational visits with every 2-week follow-up and analyzed the outcomes of a 1-month education program (Figure 1). This comprehensive educational program was performed with educating patients with pamphlet by physicians and educational video by nurses.
At first visit, we obtained the informed consent from each patient and conducted a knowledge assessment about their chronic airway disease, and tested the inhaler technique before the patients received the educational program. At the second and third visits, this education program were repeated. Questionnaires were completed by patients and physicians at the first visit and third visit to evaluate the following items; the knowledge about COPD, COPD assessment test (CAT), inhaler use technique, and measurement items of each topic were composed of six (knowledge), eight (CAT), seven (inhaler use), three (satisfaction of the patients), and five items (satisfaction of the physicians). Each item had 4 grade scales such as “strongly disagree, somewhat disagree, somewhat agree, strongly agree.” Minimum Clinically Important Difference (MCID) for objective evaluation of quality of life improvement was defined as the improvement of 4 points or more in CAT score15.
The study protocol was reviewed and approved by the Inje University Institutional Review Board (IIT-2014-283). Written informed consent, describing the purpose of the study was obtained from all the participating patients.
All data were expressed as mean±SD or percentage. We determined the 95% confidence interval of each variable from the mean and standard deviation. Paired t test was used for the comparison of continuous variables before and after education. We used chi-square test was used for categorical variables. The chi-square test was used for categorical data before and after education. A p-value of <0.05 was deemed statistically significant. All data were analyzed with SPSS version 21.0 (IBM Corp., Armonk, NY, USA).
Out of 147 COPD patients initially enrolled, 127 patients patients (male, 89%; mean age, 67.8±14.2 years) with COPD completed this study. The baseline characteristics are shown in Table 1. Hypertension was the most frequent comorbidity (n=61, 48.0%). For 1 year prior to this study, previous education about COPD was not performed in 60.3% and inhaler training was not done in 44.4% (Table 1).
Inhaler use technique was assessed stage by stage from opening the lid to rinsing the mouth after inhalation. Before this program, positive answer for enough breathing out before inhalation and holding their breath for 5 seconds after inhalation was only 32.3% and 40.2%, respectively. However, after the completion of this education program, every item regarding inhaler usage was improved significantly as assessed by physicians (p<0.05) (Table 2).
Total CAT score and all items in the CAT score except ‘have lots of energy’ were significantly improved after this comprehensive program (p<0.05) (Figure 2). All items concerning patients' knowledge about COPD per se and management of problems arising from COPD showed significant positive changes as well (p<0.01) (Figure 3).
In 44.9% of enrolled patients, the improvement of MCID or more in CAT were achieved through this program.
After the inhaler usage education, the following four of all seven items regarding inhaler usage achieved the improvement of MCID or more (p<0.05): (1) open the lid correctly; (2) hold the inhaler correctly; (3) hold the breath for 5 seconds after inhalation; and (4) rinse their mouth after inhaler use (Table 3).
After the education of the understanding on COPD, the following four items were associated with the improvement of MCID or more (p<0.05): (1) COPD is a disease that should be consistently treated; (2) the most important medicine in the treatment of COPD is inhaler; (3) I know about the method of inhaler usage, well; and (4) I use inhalers on a regular basis according to the physician's advice (Table 4).
Our study demonstrated that a comprehensive education program including inhaler training and COPD management performed at primary care setting resulted in positive outcomes including correct inhaler usage, improvement of CAT score, and patients' better understanding of COPD management.
Therefore, authors are of the opinion that education program about the clinical course of COPD should be combined with inhaler training to overcome poor adherence and improve the outcomes of COPD.
Our study has some noteworthy findings.
First, inhaler training and organized education program on COPD management with pamphlet and educational video (specially designed by The Korean Academy of Tuberculosis and Respiratory Diseases) made significant improvements on many outcomes including inhaler usage, CAT score, and knowledge about COPD, in COPD patients treated by primary care physicians. Few studies have addressed the clinical outcomes of COPD assessed by clinicians and patients through comprehensive program with a visual education by video and pamphlet, including the education of patients on the management of COPD and inhaler training.
In inhaler items of our study, positive answers for enough breathing out before inhalation, holding their breath for 5 seconds after inhalation, and understanding the manner of inhalation were only 32.3%, 40.2%, and 44.9% respectively, before inhaler training. However, positive answers for all the items regarding inhaler usage increased after inhaler training.
Previous studies showed that correct usage of inhalers was 58.9% for dry powder inhaler (DPI) and 31.1% for pressurized metered dose inhaler (pMDI), and that proper training led to an improvement in correct usage of inhalers to 92.6% for DPI and to 45.2% for pMDI5.
Misuse of inhaler devices due to inadequate training can lead to poor disease control and an increase in health care cost in COPD and asthma16.
Analysis of Torch study over 3-year period showed that increased adherence independent of study treatment was associated with improved mortality and reduction in hospital admission in COPD, although direct comparison between Torch study and our findings is not possible because of different study design10.
Another randomized controlled trial in COPD over 3-month period demonstrated that the intervention focusing on inhalation technique and adherence to maintenance therapy could reduce hospitalization rate17.
Second, all the items of our study concerning the knowledge on COPD care showed a remarkable improvement after comprehensive disease education program. The effect of comprehensive disease education was further proven in findings that most items regarding the understanding of COPD being associated with improvement of MCID or more.
One limitation is that our study cannot prove whether the comprehensive education per se may have been a placebo effect due to the single arm design. Another limitation is that this study did not demonstrate how long the effect of comprehensive education will last and how often the education should be performed on a long-term basis. Further studies are required to instruct such points.
The improvement of MCID or more were achieved in 44.9% of enrolled patients, through this program. We defined MCID as 4 points or more of CAT score, in keeping with previous report using this cohort, although our definition is a conservative approach, compared to other studies15.
Comprehensive management including smoking cessation, nutrition, exercise, vaccination, and co-morbidities is necessary in the care of COPD along with proper inhalation therapy, since COPD is deemed a syndrome with a high prevalence of comorbidities18.
Despite advancement in medical treatment, poor adherence remains a major challenge in the management of COPD101119. Patients' perception about disease process and recommended treatment is critical in improving medication adherence in COPD patients919.
Before disease education program, only 36.8% of total patients gave positive answers on coping with acute exacerbation of COPD, but remarkable positive change with positive answer rate of 82.4% occurred after this education program.
Acute exacerbation of COPD can lead to more severe lung function decline and worse quality of life in the clinical course of COPD patients202122. Previous studies reported a high incidence of unreported exacerbations which can have an impact on health status2324.
This study has several limitations.
First, this study did not include a control group because lack of inhaler training and no education on the management of COPD could be hazardous for control group. Accordingly, we investigated the effect of educational intervention in a design comparing clinical markers before and after comprehensive educational program.
Second, observation period was not long enough to assess the major outcomes of COPD such as acute exacerbation, hospitalization, and mortality.
Third, COPD was not diagnosed with traditional post-bronchodilator ratio of FEV1 to forced vital capacity <0.7. However, the FEV1/FEV6 can substitute FEV1/forced vital capacity as a valid alternative in diagnosing airflow obstruction, in primary care setting for screening COPD1314.
Fourth, the severity of COPD was not assessed because spirometry was not performed in primary care setting.
Fifth, other outcome measures such as exercise test and smoking cessation rate were not performed.
In conclusion, our study showed that in the primary care setting, a comprehensive education program including inhaler training and COPD management resulted in correct inhaler usage and improvement of CAT score, suggesting that such programs should be extended further in the primary care of COPD.
Figures and Tables
Figure 2
Chronic obstructive pulmonary disease assessment test (CAT) score before and after comprehensive education program (n=125).
(A) Total CAT score (20.1±9.6 vs. 15.7±9.0, p<0.001). (B) 1: I never cough (2.67±1.48 vs. 1.91±1.43, p<0.001); 2: sputum (2.84±1.43 vs. 2.30±1.36, p<0.001); 3: chest tightness (2.34±1.69 vs. 1.75±1.46, p<0.001); 4: dyspnea (3.36±1.42 vs. 2.69±1.54, p<0.001); 5: limitation on home activity (2.08±1.67 vs. 1.39±1.37, p<0.001); 6: confidently leaving my home (2.05±1.60 vs. 1.66±1.48, p=0.008); 7: sleep soundly (2.15±1.68 vs. 1.66±1.53, p=0.001); 8: have lots of energy (2.57±1.47 vs. 2.28±2.30, p=0.189). Values are presented as mean±SD. *p<0.05.
Figure 3
Change of knowledge about chronic obstructive pulmonary disease (COPD) before and after comprehensive education program. A: I understand COPD well (45.2% vs. 88.9%, p<0.001); B: COPD is a disease that should be consistently treated (73.8% vs. 98.4%, p<0.001); C: I know about how to cope with sudden aggravation of respiratory symptoms (37.3% vs. 82.5%, p<0.001); D: The most important medicine in the treatment of COPD is inhaler (60.3% vs. 95.2%, p<0.001); E: I know about the method of inhaler use well (69.6% vs. 97.6%, p<0.001); F: I use inhalers regularly according to the physician's advice (69.0% vs. 96.0%, p<0.001). Values of positive answers are presented as percentage. *p<0.05.

Table 1
Baseline characteristics of enrolled COPD patients

Table 2
Inhaler usage assessed by physicians before and after inhaler training

Table 3
Evaluation of CAT change by MCID after the education of inhaler usage

Table 4
Evaluation of CAT change by MCID after education of the understanding on COPD

Acknowledgments
Dr. Tae-Eun Kim was supported by a training program grant from the Korea Healthcare Technology R&D Project, Ministry for Health & Welfare, Republic of Korea (HI14C2339).
The registration number of this clinical trial is NCT02827929.
References
1. Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007; 176:532–555.
2. Yoo KH, Kim YS, Sheen SS, Park JH, Hwang YI, Kim SH, et al. Prevalence of chronic obstructive pulmonary disease in Korea: the fourth Korean National Health and Nutrition Examination Survey, 2008. Respirology. 2011; 16:659–665.
3. Kim SA, Lee JH, Kim EK, Kim TH, Kim WJ, Lee JH, et al. Outcome of inhaler withdrawal in patients receiving triple therapy for COPD. Tuberc Respir Dis. 2016; 79:22–30.
4. Zwerink M, Brusse-Keizer M, van der Valk PD, Zielhuis GA, Monninkhof EM, van der Palen J, et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014; (3):CD002990.
5. Aydemir Y. Assessment of the factors affecting the failure to use inhaler devices before and after training. Respir Med. 2015; 109:451–458.
6. Jarvis S, Ind PW, Shiner RJ. Inhaled therapy in elderly COPD patients; time for re-evaluation? Age Ageing. 2007; 36:213–218.
7. VanderSchaaf K, Olson KL, Billups S, Hartsfield CL, Rice M. Self-reported inhaler use in patients with chronic obstructive pulmonary disease. Respir Med. 2010; 104:99–106.
8. Pothirat C, Chaiwong W, Phetsuk N, Pisalthanapuna S, Chetsadaphan N, Choomuang W. Evaluating inhaler use technique in COPD patients. Int J Chron Obstruct Pulmon Dis. 2015; 10:1291–1298.
9. George J, Kong DC, Thoman R, Stewart K. Factors associated with medication nonadherence in patients with COPD. Chest. 2005; 128:3198–3204.
10. Vestbo J, Anderson JA, Calverley PM, Celli B, Ferguson GT, Jenkins C, et al. Adherence to inhaled therapy, mortality and hospital admission in COPD. Thorax. 2009; 64:939–943.
11. Bryant J, McDonald VM, Boyes A, Sanson-Fisher R, Paul C, Melville J. Improving medication adherence in chronic obstructive pulmonary disease: a systematic review. Respir Res. 2013; 14:109.
12. Lee JY, Yoo KH, Kim DK, Kim SH, Kim TE, Kim TH, et al. Effects of educational interventions for chronic airway disease on primary care. J Korean Med Sci. 2016; 31:1069–1074.
13. Bhatt SP, Kim YI, Wells JM, Bailey WC, Ramsdell JW, Foreman MG, et al. FEV1/FEV6 to diagnose airflow obstruction. Comparisons with computed tomography and morbidity indices. Ann Am Thorac Soc. 2014; 11:335–341.
14. Vandevoorde J, Verbanck S, Schuermans D, Kartounian J, Vincken W. FEV1/FEV6 and FEV6 as an alternative for FEV1/FVC and FVC in the spirometric detection of airway obstruction and restriction. Chest. 2005; 127:1560–1564.
15. Gupta N, Pinto LM, Morogan A, Bourbeau J. The COPD assessment test: a systematic review. Eur Respir J. 2014; 44:873–884.
16. Roggeri A, Micheletto C, Roggeri DP. Inhalation errors due to device switch in patients with chronic obstructive pulmonary disease and asthma: critical health and economic issues. Int J Chron Obstruct Pulmon Dis. 2016; 11:597–602.
17. Tommelein E, Mehuys E, Van Hees T, Adriaens E, Van Bortel L, Christiaens T, et al. Effectiveness of pharmaceutical care for patients with chronic obstructive pulmonary disease (PHARMACOP): a randomized controlled trial. Br J Clin Pharmacol. 2014; 77:756–766.
18. Vanfleteren LE, Spruit MA, Groenen M, Gaffron S, van Empel VP, Bruijnzeel PL, et al. Clusters of comorbidities based on validated objective measurements and systemic inflammation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013; 187:728–735.
19. George J, Kong DC, Stewart K. Adherence to disease management programs in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2007; 2:253–262.
20. Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007; 370:786–796.
21. Bourbeau J, Ford G, Zackon H, Pinsky N, Lee J, Ruberto G. Impact on patients' health status following early identification of a COPD exacerbation. Eur Respir J. 2007; 30:907–913.
22. Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002; 57:847–852.
23. Langsetmo L, Platt RW, Ernst P, Bourbeau J. Underreporting exacerbation of chronic obstructive pulmonary disease in a longitudinal cohort. Am J Respir Crit Care Med. 2008; 177:396–401.
24. Seemungal TA, Donaldson GC, Bhowmik A, Jeffries DJ, Wedzicha JA. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000; 161:1608–1613.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download