Abstract
In 2011, a cluster of peripartum patients were admitted to the intensive care unit of a tertiary hospital in Seoul with signs and symptoms of severe respiratory distress of unknown etiology. Subsequent epidemiological and animal studies suggested that humidifier disinfectant (HD) might represent the source of this pathology. Epidemiological studies, animal studies, and dose-response analysis demonstrated a strong association between HD use and lung injuries. The diagnostic criteria for HD-associated lung injury (HDALI) was defined on the basis of the clinical, pathological, and radiological attributes of the patients. The clinical spectrum of HDALI appears to range from asymptomatic to full-blown acute respiratory failure, and some patients have required actual lung transplantation for survival. The overall mortality of the exposed population was not significant, although peripartum patients and children who were admitted to the intensive care unit did show high mortality rates. Persistent clinical findings such as diffuse ill-defined centrilobular nodules and restrictive lung dysfunction were observed in some of the survivors. The findings of this review emphasize the importance of assessment of the level of toxicity of chemical inhalants utilized in a home setting, as well as the need to identify and monitor afflicted individuals after inhalational injury.
Many people in Korea would use a humidifier during winters to relieve respiratory symptoms and dry skin. People started to dilute humidifier disinfectants (HDs) in the humidifier water tanks to prevent microbial growth. Disinfectants were then dispersed into the air by the humidifier's aerosolizer. Use of HDs became popular, which potentially exposed up to 30% of the entire Korean population between 2006 and 20111.
In the spring of 2011, a cluster of young pregnant women who were previously healthy were admitted to the intensive care unit (ICU) of a tertiary hospital in Seoul due to unexplained severe respiratory distress2. These unusual cases were reported to the Korea Center for Disease Control and Prevention (KCDC). Subsequent epidemiological studies34 and a disinfectant inhalation animal study5 revealed that exposure to nebulized HDs was the cause of respiratory failure in these patients. In November 2011, the KCDC officially announced a causal relationship between lung injury and use of HD6, following which the government ordered an immediate recall of all HD products from the market.
There have been many changes in the 6 years since the tragic outbreak event. In 2013, a nationwide study was conducted to ascertain and classify all potential cases of HD-associated lung injury (HDALI) prior to the government-mandated recall. All survivors were prospectively followed up at the Environmental Health Center for Hazardous Chemical Exposure, which is funded by the Ministry of Environment. Several studies have described the outbreak of lung injury and its causative association with HD278. However, there are limited data evaluating the course of the disease and its related prognostic factors. This review summarizes the clinical characteristics of HDALI, followed by a discussion on the disease course of HDALI, focusing on the short- and long-term prognosis.
To date, epidemiological studies that examined the causal association between HD exposure and severe lung injuries were case-control studies349. These studies were different in their subjects and controls: (1) 16 children with 47 acute lobar pneumonia, asthma, and healthy controls4; (2) 18 adults with 121 hospital-based controls3; and (3) 16 adults with 60 community-based controls9. Each study demonstrated a strong association between the use of HD and severe lung injuries (odds ratio, 2.73, 47.3, and 116.1 in each study, respectively) even when indoor fungus or other chemical usage were taken into consideration. Meanwhile, the exposure rates to HDs in controls were 23%, 26%, and 22% in each study, respectively, showing that exposure rate of HD in the general population was over 20%. The clinical conditions of toxic HDs may be more affected by the environment of families than by genetic causes, considering that about 20% of cases reported victims within a family and less than 10% of cases had underlying lung disease27.
Most of the HDs that were on the Korean market before the ban contained polyhexamethylene guanidine phosphate (PHMG), oligoethoxyethyl guanidine chloride (PGH), or chloromethylisothiazolinone/methylisothiazolinone10. HDALI is biologically plausible, as shown by a toxicological study on rats: the histopathological findings of rats that inhaled PHMG and PGH were identical to those of the patients with HDALI511.
In 2013, the KCDC conducted a nationwide study of HDALI to assess the dose-response relationship. Home visits and administration of a standardized questionnaire were arranged to assess exposure circumstances: (1) whether any HD remained in the home; (2) daily and seasonal patterns of humidifier and HD use; (3) the name, amount, and frequency of disinfectant added to the humidifier water tank; (4) room size and ventilation; and (5) the general condition of each home12. Dose-response analysis revealed that the exposure density, hours of exposure during a day, and days of exposure during a week were significant risk factors for death, whereas the yearly pattern (seasonal or perennial exposure) and cumulative exposure were not8. These findings suggest that a certain minimum intense acute exposure or recurrent intense exposure without adequate recovery time between exposures is required for development of HDALI.
The presenting symptoms for HDALI were nonspecific. Most of the patients complained of cough and dyspnea, whereas some patients progressed rapidly and developed symptoms akin to those of severe acute respiratory distress syndrome. The radiological findings revealed a rather unique chronological pattern (Figure 1). The initial stage was characterized by multifocal, patchy areas of consolidation at the lower lungs with relative subpleural sparing. In the latter stages, the lesions evolved into diffuse centrilobular ground-glass opacity that involved the entire lung with no zonal predominance. Spontaneous pneumothorax or pneumomediastinum was frequently observed. Pathological findings were also unique (Figure 2). A fibroinflammatory process, which predominantly involved the bronchioles and the centrilobular lung parenchyma with no notable granulomas, was observed. The bronchiolar lesions were characterized by epithelial sloughing and replacement with flattened regenerating cells; mild to severe subepithelial fibroblastic proliferation resulting in bronchiolar obliteration; and varying degrees of peribronchiolar fibrosis. The parenchymal lesions showed alveolar damage and the disease spectrum ranged from an early exudative phase to an extensive fibroproliferative phase. The subpleural and paraseptal spaces were relatively well-preserved. The diagnostic criteria for HDALI were defined based on the clinical, pathological, and radiological features of patients (Table 1)8.
In the first and second rounds of clinical assessment through a nationwide study, 294 adult cases were identified and classified as follows: 56 definite (19%), 32 probable (11%), 45 possible (15%), and 158 unlikely (54%), based on the prior agreed-upon diagnostic criteria (Table 1). Of the 88 cases with definite and probable disease, 84 consented to monitoring. Recently, we described these 84 patients13. The median (interquartile range) age was 35 years (range, 26–70 years), and most were women in the peripartal period. The incidence of lung disease was in March, almost at the end of winter, while the maximum incidence rate was at the end of April. The clinical course of this disease was subacute. The clinical spectrum of HDALI appears to range from asymptomatic to full-blown acute respiratory failure and death. Patients who experience mild hypoxemia responded to supportive care such as conventional oxygen therapy, antibiotic treatment, and use of steroids. However, those with refractory hypoxemia exhibited rapid progression despite the administration of antibiotics, antivirals, antifungals, steroids, and other immunosuppressants, as well as mechanical ventilation and extracorporeal membrane oxygenation. All patients who had undergone pulmonary function test showed a restrictive pattern and decreased diffusing capacity. The restrictive pattern may be due to both bronchiolar destruction and alveolar damage from the early stage. Examination of bronchoalveolar lavage fluid did not show any dominant cell type. In all patients, the sputum, bronchoalveolar lavage fluid, and blood samples were negative for bacteria, viruses, and fungi, which indicated that the injury was indeed due to a noninfectious cause. Nine patients who had undergone liver and renal function tests showed normal values.
A total of 46% of patients were admitted to the ICU. Of those who required mechanical ventilation, 74% died, and six patients required lung transplantation. The overall mortality rate was 36%. Compared to survivors, non-survivors were more likely women, young, and pregnant. A recent study found that many pregnant women in Korea used humidifiers114. Because these populations tend to remain inside the house, they may have been exposed longer to HD aerosol during winter than other populations. In addition, non-survivors had worse pulmonary function and more right heart failure than survivors at diagnosis of HDALI. Fifty-eight affected survivors were prospectively followed up by the Environmental Health Center for Hazardous Chemical Exposure. They were invited to undergo laboratory tests, chest computed tomography (CT) imaging, spirometry, and echocardiogram annually. In the following paragraphs, the follow-up results are presented.
Of the 46 patients who underwent laboratory follow-up, only one patient showed elevated level of liver enzymes (aspartate transaminase and/or alanine transaminase >40 IU/L). Three patients had high levels (>1.2 mg/dL) of serum creatinine. During the follow-up period, an echocardiogram was performed in 44 patients, of which six patients showed abnormal findings. However, these echocardiographic findings were considered unrelated to the lung injury.
To identify clinical and radiological findings that affect disease severity and short-term prognosis of HDALI in adults, a total of 132 CT scans of 59 patients were examined15. CT scans for all patients were categorized on the basis of the interval between the CT scan date and the initial symptom presentation: within 1 month, 2 months, 3 months, 6 months, 1 year, or annually, thereafter. Spontaneous pulmonary interstitial emphysema, pneumomediastinum, and pneumothorax were found to have developed within 1–3 months of the initial symptoms. The incidence of fibrosis and bronchiectasis gradually increased after 2–3 months and the lesions tended to persist. Young age, peripartum, low O2 saturation, and ground-glass opacity or consolidation (>30%) on the initial chest radiograph were associated with increased risk of ICU admission. CT findings of consolidation, pneumomediastinum, and pulmonary interstitial emphysema were risk factors for lung transplantation and mortality. Interestingly, although the diffuse extensive ill-defined centrilobular nodules gradually diminished in size, these tended to persist even after 5 years.
We recently assessed 40 adult survivors with HDALI who underwent annual spirometry to evaluate the long-term changes in lung function after HD exposure and sought to identify the factors associated with these changes16. During the first 3 years, forced vital capacity (FVC) increased significantly from 55% of the predicted at onset to 80% of the predicted at year 3, and forced expiratory volume in 1 second also rose markedly from 61% to 85% of the predicted. At year 4, these values stabilized at 80% and 84% of the predicted, respectively (Figure 3). The proportion of patients with abnormal FVC (<80% of the predicted) decreased from 88% (35/40) at onset to 48% (19/40) at year 4 (Figure 4A). In 19 out of the 35 patients (54%) who showed abnormal lung function at onset, FVCs did not recover to normal levels (Figure 4B). Persistently severe restrictive lung function (FVC <50% of the predicted) was seen in 13% (5/40) patients. Impaired recovery was associated with lung function at onset and the intensity of HD exposure, which reinforces the association of HD with lung injury.
Some serious patients even required lung transplantation for survival. To date, a total of ten patients received lung transplantation for HDALI. Eight patients remain active without any limitations, while two patients died of acute rejection and concomitant pneumonia post-transplantation. Thus, the overall survival rate is 80%. Most patients received lung transplantation during the affected period in the subacute stage of HDALI. We earlier reported a 33-year-old woman who underwent lung transplantation approximately 4 years after severe HDALI17. Her clinical, radiological, and pathological findings were similar to those who received lung transplantation during the affected period. The patient's clinical and radiological findings showed significant improvement and no postoperative complications were observed, which suggests that lung transplantation can be a therapeutic option for patients with chronic inhalational injury.
In 2011, investigators reviewed previously reported cases of infants with severe interstitial lung disease of unknown etiology that occurred in the early spring of every year since 1995. They found out that these cases showed similar clinical, radiological, and pathological patterns as those noted in adults, including pregnant and postpartum women18. Along with exposure conditions, age and pregnancy may also increase the risk of lung injury. In a retrospective cohort study on the association between HD use and lung injury using the first round of clinical assessment8, young mothers or pregnant women together with their infants occupied a large portion of the study population. Moreover, more females than males, and more infants younger than 4 years old, were included among the definite and probable cases. In this study, the overall mortality was about 8%. Mortality was highest for infants, especially those 2 years of age or younger, with 18%–27% mortality. Mortality was also higher for pregnant women, at about 12%. In multivariate analysis of survival time after exposure to PHMG, age at onset younger than 4 years was a significant risk factor for shortening survival.
We remain unaware of the entire spectrum of this illness induced by HDs. Therefore, we have only focused on HDALI. Improvement in clinical disease or lung function was observed in some of the patients. The exact causes of reversibility are not clear and this should be answered in future research. There is clear evidence of persistent clinical findings in those who stopped the use of the suspect HDs. The diffuse extensive ill-defined centrilobular nodules do not disappear in the chronic stage, even in patients followed up for 7 years. Long-term follow-up of survivors showed that half of the patients did not recover from the restrictive lung dysfunction, even after 4 years. These findings emphasize the importance of monitoring individuals after inhalational injury.
Figures and Tables
 | Figure 1The three stages of humidifier disinfectant-associated lung injury in a 33-year-old woman. (A) Initial computed tomography (CT) scan shows diffuse centrilobular ground-glass opacity nodules with patchy multifocal consolidations. (B) CT examination performed on the day of admission to our hospital shows resolution of the consolidations, but diffuse ground-glass opacity nodules have become more distinct. (C) Follow-up CT scan obtained 2 weeks after admission shows persistence of diffuse ground-glass opacity nodules and pneumomediastinum. |
 | Figure 2Pathology of the explanted lungs. (A) The main pathology was that of a fibroinflammatory process, which predominantly involved the bronchioles and centrilobular lung parenchyma in the absence of notable granuloma formation. Subpleural and paraseptal airspaces were relatively preserved (H&E stain, ×40). (B) Parenchymal lesions showed histological patterns, which ranged from the early exudative phase to the extensive fibrosing phase (H&E stain, ×40). |
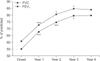 | Figure 3Mean changes in lung function over time after humidifier disinfectant-associated lung injury. FVC: forced vital capacity; FEV1: forced expiratory volume in 1 second. ***p<0.001, *p<0.05 compared with the previous year, as assessed with repeated measures analysis of variance. |
 | Figure 4Frequency over time of patients whose lung function was normal of abnormal (A) or whose lung function improved (B) compared with previous years. Five patients who had normal lung function at onset were excluded from this analysis. It was considered to have improved but not normalized if the forced vital capacity % predicted (FVC%pred) increased but did not achieve ≥80%. The total number of patients in each group is shown above the bar. |
Table 1
Diagnostic criteria for HD-associated lung injury

*Clinical evidence of disinfectant included: (1) acute or subacute development of cough, dyspnea, or breathlessness; (2) physical signs of spontaneous air leakage, including subcutaneous or mediastinal emphysema; and (3) chest radiographic features of terminal bronchiolar damage.
HD: humidifier disinfectant; CT: computed tomography.
Acknowledgments
This work was supported by the Environmental Health Center for Hazardous Chemical Exposure, which is funded by the Ministry of Environment, Republic of Korea (2015-0510). The funders had no role in preparation of the manuscript or decision to publish.
References
1. Jeon BH, Park YJ. Frequency of humidifier and humidifier disinfectant usage in Gyeonggi provine. Environ Health Toxicol. 2012; 27:e2012002.
2. Hong SB, Kim HJ, Huh JW, Do KH, Jang SJ, Song JS, et al. A cluster of lung injury associated with home humidifier use: clinical, radiological and pathological description of a new syndrome. Thorax. 2014; 69:694–702.
3. Kim HJ, Lee MS, Hong SB, Huh JW, Do KH, Jang SJ, et al. A cluster of lung injury cases associated with home humidifier use: an epidemiological investigation. Thorax. 2014; 69:703–708.
4. Yang HJ, Kim HJ, Yu J, Lee E, Jung YH, Kim HY, et al. Inhalation toxicity of humidifier disinfectants as a risk factor of children's interstitial lung disease in Korea: a case-control study. PLoS One. 2013; 8:e64430.
5. Kim HR, Lee K, Park CW, Song JA, Shin DY, Park YJ, et al. Polyhexamethylene guanidine phosphate aerosol particles induce pulmonary inflammatory and fibrotic responses. Arch Toxicol. 2016; 90:617–632.
6. Korea Center for Disease Control and Prevention. Interim report of epidemiological investigation on lung injury with unknown cause in Korea [Internet]. Cheongju: Korea Center for Disease Control and Prevention;2011. cited 2017 Feb 9. Available from: http://cdc.go.kr/CDC/cms/content/mobile/00/12700_view.html.
7. Kim KW, Ahn K, Yang HJ, Lee S, Park JD, Kim WK, et al. Humidifier disinfectant-associated children's interstitial lung disease. Am J Respir Crit Care Med. 2014; 189:48–56.
8. Paek D, Koh Y, Park DU, Cheong HK, Do KH, Lim CM, et al. Nationwide study of humidifier disinfectant lung injury in South Korea, 1994-2011: incidence and dose-response relationships. Ann Am Thorac Soc. 2015; 12:1813–1821.
9. Park JH, Kim HJ, Kwon GY, Gwack J, Park YJ, Youn SK, et al. Humidifier disinfectants are a cause of lung injury among adults in South Korea: a community-based case-control study. PLoS One. 2016; 11:e0151849.
10. Lee JH, Kim YH, Kwon JH. Fatal misuse of humidifier disinfectants in Korea: importance of screening risk assessment and implications for management of chemicals in consumer products. Environ Sci Technol. 2012; 46:2498–2500.
11. Park S, Lee K, Lee EJ, Lee SY, In KH, Kim HK, et al. Humidifier disinfectant-associated interstitial lung disease in an animal model induced by polyhexamethylene guanidine aerosol. Am J Respir Crit Care Med. 2014; 190:706–708.
12. Park DU, Friesen MC, Roh HS, Choi YY, Ahn JJ, Lim HK, et al. Estimating retrospective exposure of household humidifier disinfectants. Indoor Air. 2015; 25:631–640.
13. Huh JW, Hong SB, Do KH, Koo HJ, Jang SJ, Lee MS, et al. Inhalation lung injury associated with humidifier disinfectants in adults. J Korean Med Sci. 2016; 31:1857–1862.
14. Chang MH, Park H, Ha M, Kim Y, Hong YC, Ha EH. Characteristics of humidifier use in Korean pregnant women: the Mothers and Children’s Environmental Health (MOCEH) study. Environ Health Toxicol. 2012; 27:e2012003.
15. Koo HJ, Do KH, Chae EJ, Kim HJ, Song JS, Jang SJ, et al. Humidifier disinfectant-associated lung injury in adults: Prognostic factors in predicting short-term outcome. Eur Radiol. 2017; 27:203–211.
16. Kim WY, Park S, Kim HJ, Chae EJ, Do KH, Huh JW, et al. Lung function in patients with lung injury due to household chemical inhalation: post hoc analysis of a prospective nationwide cohort. Respirology. 2017; 22:345–351.
17. Kim WY, Kim SW, Jo KW, Choi SH, Kim HR, Kim YH, et al. Lung transplantation for chronic humidifier disinfectant-associated lung injury. Korean J Crit Care Med. 2016; 31:146–151.
18. Cheon CK, Jin HS, Kang EK, Kim HB, Kim BJ, Yu J, et al. Epidemic acute interstitial pneumonia in children occurred during the early 2006s. Korean J Pediatr. 2008; 51:383–390.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download