Abstract
Purpose
Although nonerosive and erosive gastroesophageal reflux disease (GERD) have similar symptom severity, nonerosive reflux disease (NERD) is considered a milder type of GERD and gastroenterologists have hesitated to refer these patients for antireflux surgery. The aim of this study was to compare surgical outcomes of antireflux surgery between patients with NERD and erosive reflux disease (ERD).
Methods
Seventy patients met the inclusion criteria of this study among a total of 117 patients who underwent antireflux surgery from November 2012 to October 2017. According to preoperative endoscopy, patients were classified into NERD group (minimal changes or no esophagitis) and ERD group. Clinical characteristics and surgical outcomes were compared between NERD and ERD.
Results
There were 26 patients in NERD group and 44 patients in ERD group. The male:female ratio was higher in the ERD group than in the NERD group (P = 0.044). Preoperative symptoms, response to acid suppressive medication, acid exposure on pH monitoring study, and esophageal manometry results were similar in the 2 groups. Reflux on barium esophagography was more frequently observed in ERD (77.3%) than in NERD (50.0%, P = 0.019). At 6 months after surgery, complete resolution and partial improvement of GERD symptoms were similar in the 2 groups (80.8% and 15.4%, respectively, in NERD vs. 88.6% and 2.3%, respectively, in ERD; P = 0.363).
Gastroesophageal reflux disease (GERD) is considered as the most common benign diseases of the upper gastrointestinal tract. Laparoscopic fundoplication is now the standard surgical treatment for GERD in Western countries, while the mainstay of GERD treatment in Korea is still medical therapy with acid suppressive drug. As the prevalence of GERD in East Asian countries has increased recently due to changes in diet, interest in surgical treatment of GERD has also emerged in Korea [1]. Most patients with GERD can be classified into 2 subtypes:
nonerosive reflux disease (NERD) and erosive reflux disease (ERD). NERD has been defined as the presence of classic GERD symptoms in the absence of esophageal mucosal injury on upper endoscopy [2]. Several studies reported that almost 70% of patients with GERD have no endoscopic evidence of esophagitis [34]. Although NERD and ERD have similar symptom severity, NERD is considered a milder type of GERD by patients and physicians. Thus, many gastroenterologists have hesitated to refer patients with typical G ERD for antireflux surgery without evidence of severe esophagitis on endoscopy.
The aim of the present study was to compare surgical outcomes of antireflux surgery in patients with NERD and ERD.
We identified 117 consecutive patients who underwent antireflux surgery from November 2012 to October 2017 at Chung-Ang University Hospital, Korea. Patients were included in the present study if the antireflux surgery was primarily conducted for the treatment of GERD, rather than as prophylaxis after another surgical procedure involving the gastroesophageal junction or revisional antireflux surgery for failed primary fundoplication. We excluded the patients when preoperative endoscopy, pH monitoring, esophageal manometry, and barium esophagography had not been performed for objective evidence of gastroesophageal reflux, and treatment outcomes were not evaluated at 6 months after antireflux surgery (Fig. 1).
A laparoscopic Nissen fundoplication was performed in all included patients. Laparoscopic Nissen fundoplication procedure sequentially consist of division of the short gastric vessels, full circumferential mobilization of the esophagus, posterior cruroplasty, and 360° total fundoplication as previously described [5].
For preoperative symptomatic evaluation, GERD symptoms were reported based on our questionnaire. Heartburn and acid regurgitation were typical symptoms while other extraesophageal symptoms such as globus sense, throat pain, hoarseness, and chronic coughing were atypical symptoms. Information on the length of time with symptoms and use of acid suppressive medication was also collected.
For preoperative evaluation of GERD, endoscopy, esophageal manometry, barium esophagography, and ambulatory pH monitoring had been performed in all enrolled patients.
Upper gastrointestinal endoscopy was performed preoperatively to determine the presence of esophagitis or hiatal hernia. Erosive esophagitis was graded according to the Los Angeles (LA) classification [6]. Patients with LA class A to D esophagitis were in the ERD group, whereas those without esophagitis and with minimal changes were in the NERD group.
Esophageal manometric measurements were performed after patients stopped taking any medication that could affect esophageal motility. A water-perfused system with a multiple-lumen catheter and an incorporated sleeve sensor (Dentsleeve, Adelaide, Australia) was used.
Ambulatory pH monitoring was performed 7 days after discontinuation of any acid suppressive medication that could affect results. We used BRAVO pH capsules (Given Imaging, Yokneam, Israel) in this study. Determination of the presence or absence of pathologic acid reflux was based on the DeMeester score calculated using the test results. Pathologic acid reflux was defined as a DeMeester score >14.7.
Barium swallow esophagography was performed with double-contrast and single-contrast technique. Structural defects such as hiatal hernia and stricture were evaluated. In patients with a wide-open lower esophageal sphincter (LES), actual reflux of contrast media could be detected.
Clinical characteristics such as demographic parameters and results of symptomatic and objective evaluations were compared in patients with NERD and ERD.
At 6 months after surgery, GERD symptoms and side effects of fundoplication were reported. Complete resolution was defined when all typical and atypical GERD symptoms were controlled, and partial improvement was defined when the primary GERD symptom was improved, but other GERD symptoms remained. Surgical outcomes of laparoscopic Nissen fundoplication on the basis of symptomatic evaluation were compared in 26 patients with NERD and 44 patients with ERD.
The chi-square test was used to compare categorical variables between 2 groups. Independent t-tests were used to compare noncategorical variables. A P-value < 0.05 was defined as statistically significant. Statistical analyses were conducted using the IBM SPSS Statistics ver. 19.0 (IBM Co., Armonk, NY, USA).
This study was approved by the Institutional Review Board (IRB) of Chung-Ang University Hospital (approval number: C2016113(1856)). Written informed consent was waived from the IRB.
Of 117 patients undergoing antireflux surgery, 70 underwent primary Nissen fundoplication for treatment of GERD after complete preoperative evaluation, and had full symptomatic evaluation at 6 months after fundoplication. A group of 26 patients was NERD group and the other group of 44 patients was ERD group (Fig. 1).
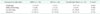
Table 1 shows the enrolled patients' characteristics. Females comprised 53.8% of the NERD group and 29.5% of the ERD group. The male:female ratio was higher in the ERD group than in the NERD group (P = 0.044). Mean age, body mass index, and duration of symptoms were similar in patients with NERD and ERD. Atypical extraesophageal symptoms tended to be more common in NERD than in ERD (69.2% vs. 56.8%), although it was not statistically significant (P = 0.303). Response to acid suppressive medication tended to be lower in NERD than in ERD (34.6% vs. 52.3%), but this tendency was not significant (P = 0.152).
The presence of hiatal hernia on endoscopy, pathologic acid reflux on pH monitoring, the mean DeMeester score, and mean pressure of LES were also similar in both groups. On the other hand, reflux on barium esophagography study was more frequently observed in ERD (77.3%) than in NERD (50.0%, P = 0.019).
At 6 months after surgery, complete resolution or partial improvement of GERD symptoms was observed in 80.8% and 15.4%, respectively, of the NERD group, versus 88.6% and 2.3% of the ERD group. Symptom resolution rates were not different between the groups (P = 0.363) (Fig. 2).
The side effects of fundoplication were evaluated postoperatively. Eight patients (11.4%) complained about occasional dysphagia at 6 months after fundoplication. Two patients (2.9%) had difficulty in belching. Gas bloating and flatulence were in 21 patients (30.0%) and 22 patients (31.4%), respectively. Most symptoms of the side effect were mild and surgical or medical treatments were not necessary for these patients. The side effects of fundoplication were not different between NERD and ERD groups (Table 2).
This study compared symptomatic outcomes of antireflux surgery for NERD and ERD. The short-term outcome after antireflux surgery for patients with NERD was comparable to the outcome for patients with ERD.
NERD and ERD are the 2 main types of GERD. According to several previous reports, only one fourths of symptomatic GERD patients have erosive esophagitis [347]. Particularly in Asia, NERD comprises 78%–93% of all reflux disease, although there has been an increase in ERD [8]. NERD is the commonest type of GERD. Many physicians and patients consider NERD to be a mild form of GERD that could progress to more severe erosive disease.
The pathophysiological relationship between NERD and ERD remains unclear. Some studies reported progression of NERD to ERD [910]. However, the assumption that NERD and ERD are components of a disease continuum has been challenged by recent studies demonstrating differences in epidemiologic, pathophysiologic, and clinical characteristics, and response to medical and surgical therapy [1112]. Bardhan et al. [13] compiled the longest and largest natural history database of GERD patients. The authors found that only 4.4% of NERD patients progressed to erosive esophagitis over a period of 24 years. Currently available data suggest that lack of progression is more common than progression to erosive esophagitis in patients with NERD [31415].
Characteristics of NERD and ERD have been reported to be different. Patients with erosive esophagitis were characterized by a higher prevalence of hiatal hernia, greater esophageal acid exposure, and greater esophageal dysmotility [3]. Literatures have shown that about 30%–50% of NERD patients demonstrate the physiological range of esophageal acid exposure [16]. In the present study, only 7 patients (26.9%) in the NERD group showed pathologic acid reflux on pH monitoring. However, acid reflux on pH monitoring in the ERD group was comparable to that in the NERD group in this study, because all enrolled patients underwent surgical treatment, and refractory GERD was more common in these study patients than in the general GERD population. Furthermore, symptom improvement after antireflux surgery was not different according to the esophageal acid exposure detected in pH monitoring study.
On the other hand, radiologic detection of actual reflux was more common in ERD than NERD in this study, and might represent another difference between ERD and NERD, especially in patients who underwent antireflux surgery. Gastroesophageal reflux can be easily demonstrated when patients have a wide-open LES. In general, the mean resting LES pressure is significantly lower in patients with erosive esophagitis than in those with NERD [17], although there was no difference in the LES pressure between NERD and ERD in this study. This is the reason why radiologic detection of reflux was more common in ERD than in NERD. According to previous literature, barium swallow esophagography should not be used for diagnosis of GERD, and the presence of gastroesophageal reflux during the test does not correlate with pH monitoring study results [18]. Although pH monitoring is considered the most objective test for GERD [15], barium swallow esophagography had a role in confirming the diagnosis, by detecting actual gastroesophageal reflux during the test in this study.
Several studies that compared the effectiveness of acid suppressive drugs for NERD and ERD have demonstrated that patients with NERD are more prone to be refractory. Previous literature reported that 30%–40% of patients with NERD do not have a symptomatic response to a proton pump inhibitor (PPI) [19]. In general, the proportion of NERD patients responsive to a standard dose of PPI is approximately 20%–30% lower than in patients with erosive esophagitis [19]. In this study, preoperative effectiveness of acid suppressive medication was not statistically different between NERD and ERD groups. This may reflect the fact that all patients in this study underwent antireflux surgery, and a common indication for surgery was ineffectiveness of medical treatment, even in cases of erosive esophagitis.
Physicians usually do not recommend surgical treatment for NERD because they consider NERD to be a mild form of reflux disease. However, the severity of mucosal damage examined by endoscopy is not correlated with the symptomatic severity [20]. A lower response to PPI treatment for NERD would support a greater role for surgery in the treatment of patients with NERD. Patients with NERD are more likely to become candidates for antireflux surgery.
The effectiveness of fundoplication was comparable for NERD and ERD in this study. However, because a poor response to medical therapy has been considered predictive of a poor surgical outcome and NERD has been known to be less responsive to PPI treatment, antireflux surgery is potentially less effective for NERD than for ERD. The previously reported outcome of antireflux surgery for NERD is contradictory. Some report similar outcomes [2122], whereas others report worse outcomes for NERD than for ERD [23]. Broeders et al. [4] compared subjective and objective outcomes of Nissen fundoplication between 96 patients with NERD and 117 with ERD for 5 years after surgery. Relief of reflux symptoms, reduction of PPI use, improvement of quality of life scores, reduction of total acid exposure time, and increase in LES pressure were all similar between NERD and ERD.
In studies reporting a worse surgical outcome of fundoplication for NERD, patients who underwent antireflux surgery had a good response to acid suppressive drugs [23]. On the other hand, in studies reporting similar outcomes including our study, the indication for surgery was mainly PPI-refractory GERD. Thus, the outcome of fundoplication for NERD compared to that for ERD might depend on the response to PPI medication. In a previous study in our institution, response to acid suppressive medical therapy with PPI was the most significant predictive factor for outcome of fundoplication [5]. Nonresponse to PPI is a poor predictor of antireflux surgery outcome, but is still an indication for antireflux surgery. Similarly, antireflux surgery for NERD may be less effective than for ERD, but NERD is still a candidate for antireflux surgery.
There were some limitations in the present study. First, symptoms at 6 months after surgery may not represent the longterm outcome of fundoplication. Second, we did not evaluate patients using an objective diagnostic modality such as pH monitoring and esophageal manometry. Therefore, there was a lack of objective evidence for a change in gastroesophageal reflux after Nissen fundoplication. However, antireflux surgery is functional surgery, and changes in patient symptoms after surgery would have greater value in determining the benefit of fundoplication. Third, this study was designed as a retrospective study and had insufficient number of patients. Thus, prospectively designed study with a sufficient number of cases is necessary. In addition, long-term outcomes and objective evaluation of reflux disease status require further study.
Even with the above-mentioned limitations, we can conclude that laparoscopic Nissen fundoplication is equally beneficial to patients with NERD and ERD. The absence of erosive esophagitis on endoscopy in patients with GERD symptoms should be no longer a reason to avoid antireflux surgery.
Figures and Tables
 | Fig. 2Change in reflux symptoms 6 months after surgery compared with preoperative status in 26 patients with NERD and 44 patients with ERD. Complete resolution of GERD symptoms was observed in 80.8% of the NERD group versus 88.6% of the ERD group (P = 0.363). NERD, nonerosive reflux disease; ERD, erosive reflux disease; GERD, gastroesophageal reflux disease. |
References
1. Jung HK. Epidemiology of gastroesophageal reflux disease in Asia: a systematic review. J Neurogastroenterol Motil. 2011; 17:14–27.

2. Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006; 101:1900–1920.

3. Hershcovici T, Fass R. Nonerosive reflux disease (NERD) - an update. J Neurogastroenterol Motil. 2010; 16:8–21.

4. Broeders JA, Draaisma WA, Bredenoord AJ, Smout AJ, Broeders IA, Gooszen HG. Long-term outcome of Nissen fundoplication in non-erosive and erosive gastrooesophageal reflux disease. Br J Surg. 2010; 97:845–852.

5. Park JM, Kim BJ, Kim JG, Chi KC. Factors predicting outcomes of laparoscopic Nissen fundoplication for gastroesophageal reflux disease: experience at a single institution in Korea. Ann Surg Treat Res. 2017; 92:184–190.

6. Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999; 45:172–180.

7. Ronkainen J, Aro P, Storskrubb T, Johansson SE, Lind T, Bolling-Sternevald E, et al. High prevalence of gastroesophageal reflux symptoms and esophagitis with or without symptoms in the general adult Swedish population: a Kalixanda study report. Scand J Gastroenterol. 2005; 40:275–285.

8. Goh KL. Gastroesophageal reflux disease in Asia: a historical perspective and present challenges. J Gastroenterol Hepatol. 2011; 26:Suppl 1. 2–10.

9. Pace F, Bollani S, Molteni P, Bianchi Porro G. Natural history of gastro-oesophageal reflux disease without oesophagitis (NERD)--a reappraisal 10 years on. Dig Liver Dis. 2004; 36:111–115.
10. Pace F, Bianchi Porro G. Gastroesophageal reflux disease: a typical spectrum disease (a new conceptual framework is not needed). Am J Gastroenterol. 2004; 99:946–949.

11. Fass R. Non-erosive reflux disease (NERD) and erosive esophagitis: a spectrum of disease or special entities? Z Gastroenterol. 2007; 45:1156–1163.
12. Fass R. Erosive esophagitis and nonerosive reflux disease (NERD): comparison of epidemiologic, physiologic, and therapeutic characteristics. J Clin Gastroenterol. 2007; 41:131–137.
13. Bardhan KD, Royston C, Nayyar AK. Reflux rising! An essay on witnessing a disease in evolution. Dig Liver Dis. 2006; 38:163–168.

14. Sontag SJ, Sonnenberg A, Schnell TG, Leya J, Metz A. The long-term natural history of gastroesophageal reflux disease. J Clin Gastroenterol. 2006; 40:398–404.

15. Isolauri J, Luostarinen M, Isolauri E, Reinikainen P, Viljakka M, Keyrilainen O. Natural course of gastroesophageal reflux disease: 17-22 year follow-up of 60 patients. Am J Gastroenterol. 1997; 92:37–41.
16. Martinez SD, Malagon IB, Garewal HS, Cui H, Fass R. Non-erosive reflux disease (NERD)--acid reflux and symptom patterns. Aliment Pharmacol Ther. 2003; 17:537–545.
17. Ho KY, Kang JY. Ref lux esophagitis patients in Singapore have motor and acid exposure abnormalities similar to patients in the Western hemisphere. Am J Gastroenterol. 1999; 94:1186–1191.
18. Bello B, Zoccali M, Gullo R, Allaix ME, Herbella FA, Gasparaitis A, et al. Gastroesophageal reflux disease and antireflux surgery-what is the proper preoperative work-up? J Gastrointest Surg. 2013; 17:14–20.

19. Dean BB, Gano AD Jr, Knight K, Ofman JJ, Fass R. Effectiveness of proton pump inhibitors in nonerosive reflux disease. Clin Gastroenterol Hepatol. 2004; 2:656–664.

20. Okamoto K, Iwakiri R, Mori M, Hara M, Oda K, Danjo A, et al. Clinical symptoms in endoscopic reflux esophagitis: evaluation in 8031 adult subjects. Dig Dis Sci. 2003; 48:2237–2241.

21. Desai KM, Frisella MM, Soper NJ. Clinical outcomes after laparoscopic antireflux surgery in patients with and without preoperative endoscopic esophagitis. J Gastrointest Surg. 2003; 7:44–52.

22. Kamolz T, Granderath FA, Schweiger UM, Pointner R. Laparoscopic Nissen fundoplication in patients with nonerosive reflux disease. Long-term quality-of-life assessment and surgical outcome. Surg Endosc. 2005; 19:494–500.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download