Abstract
Purpose
The transoral endoscopic thyroid surgery vestibular approach (TOETVA) is one of the newest techniques which do not result in an anterior neck scar. We report herein our initial experience with TOETVA and its short-term outcomes in patients with papillary thyroid carcinoma (PTC).
Methods
This case series consisted of all consecutive patients who underwent TOETVA in our institution between August 2016 and June 2017. Indications for TOETVA were an fine needle aspiration-confirmed PTC or follicular neoplasm, an intrathyroidal tumor with a diameter of less than 2 cm, and no clinical evidence of central or lateral lymph node metastasis. A total of 20 patients underwent TOETVA and we retrospectively reviewed clinicopathologic data and short-term postoperative outcomes.
Results
Among the 20 TOETVA cases, 7 were total thyroidectomy, 12 were lobectomy and 1 was wide isthmusectomy. Mean age was 50.8 years and mean operation time was 152 ± 51.4 minutes. Tumor size ranged from 0.2–1.4 cm and the mean size of harvested central lymph nodes was 2.8 (range, 0–10). Neither mental nerve injury nor surgical site infection occurred. One patient had transient vocal cord palsy and 1 patient developed a neck seroma. Among 7 total thyroidectomy patients, 3 patients developed transient hypocalcemia.
Global incidence of thyroid cancer has gradually increased in recent decades [1]. Papillary thyroid carcinoma (PTC), which is the most common subtype of all thyroid cancers, is particularly prevalent in young women [2]. Such patients are particularly concerned about anterior neck scars after traditional thyroid surgery. As a result, surgeons have developed various thyroid surgery methods that either reduce or hide the wound. Two recently developed surgical approaches are the endoscopic/robotic bilateral axillo-breast approach and the transaxillary approach (BABA) [3456]. These methods involve remote skin incisions on the axillary fold and/or the breast.
A new concept in the field of surgery is natural orifice transluminal endoscopic surgery (NOTES), where surgery is performed through a natural mucosal orifice such as the mouth or rectum [7]. The mucosal wounds are perfectly hidden from view and heal without leaving scars. In 2008, Witzel et al. [8] reported the first results of NOTES for thyroid surgery. They reported that the transoral approach in living pigs was a safe and easy procedure. In the following 6 years, several studies in living pigs, human cadavers, and small numbers of patients were performed to optimize the transoral approach for thyroid surgery [910111213]. Then, in 2014, Wang et al. [14] performed a small randomized clinical trial with patients who underwent endoscopic thyroidectomy by either the areola approach or the vestibular approach. They reported that there were no differences in surgical time, blood loss, or postoperative hospital stay between the 2 groups and also that they experienced no superior laryngeal nerve injury, recurrent laryngeal nerve injury, hypocalcemia, postoperative fluid collection, or incomplete resection cases. In 2016, Anuwong [15] reported the first large case series (60 patients) of transoral endoscopic thyroidectomy using the vestibular approach (TOETVA). They reported that none of the patients had surgical site infections or mental nerve injuries, which alleviated concerns that others in the field had about transoral thyroid surgery.
After this large case series was published, many endocrine surgeons over the world started using TOETVA-like transoral thyroid surgery methods in their centers [1617181920]. However, most TOETVA studies were conducted with benign thyroid nodules or on a small number of thyroid cancer cases. We would like to report our initial experience with TOETVA performed by a single surgeon on consecutive PTC patients.
This case series consisted of 20 consecutive patients who underwent TOETVA in Seoul National University Hospital between August 2016 and June 2017. Indications for TOETVA were as follows: a lesion that was confirmed to be PTC or suspicious of PTC or follicular neoplasm by preoperative fine needle aspiration, a tumor diameter (as estimated by ultrasonography) of less than 2 cm, a tumor located in the thyroid, no clinical evidence of central and lateral neck node metastasis, and no history of neck or intraoral surgery.
All patients agreed to undergo TOETVA after being informed about the potential benefits and risks of the procedure. A single endocrine surgeon performed all TOETVAs. The medical records and pathology data of all the patients were reviewed in this case series and this study was approved as a waiver of agreement from the IRB of Seoul National University Hospital (approval number: 1715-020-851).
Patient was placed under general anesthesia with endotracheal intubation using a NIM 3.0 EMG tube (Medtronic, Minneapolis, MN, USA) and then positioned in the supine position with extension of the neck. The patient's head was firmly fixed to prevent neck rotation during the surgery. Oral cavity irrigation and vestibular area cleansing were conducted by using 0.05% Hibitane solution.
Three vestibular incisions were made (Fig. 1A). One was an 11-mm transverse incision above the frenulum for the camera port, and the other 2 were 5-mm vertical incisions that were made laterally from the incisors and were to receive the instrumental ports. After making the incisions, hydrodissection method with 1:200,000 epinephrine in normal saline solution was used to detach the strap muscles and platysma muscles. Trochars were placed as shown in Fig. 1B. We used a 10-mm 30° scope and 5- to 7-mmHg pressure with a high flow (15–20 L/min) setting for CO2 inflation.
Thyroidectomy procedures used for transoral endoscopic right lobectomy are shown in Fig. 2. Midline between both strap muscles was divided from the sternal notch to the thyroid cartilage (Fig. 2A). After strap muscle division, isthmus was cut from the inferior portion of cricoid cartilage (Fig. 2B). Thyroid was retracted to the opposite side and connective tissue between the thyroid and the strap muscle was dissected; moreover, the middle thyroid vein was ligated by using an ultrasonic device (Fig. 2C). In all the cases, superior thyroidal vessels and the tip of the thyroid upper pole were fully accessible in TOETVA. These structures were also safely divided by using the ultrasonic device (Fig. 2D). After division of the upper pole, the superior parathyroid gland was identified beneath the cut surface of the upper pole (Fig. 2E). The recurrent laryngeal nerve was identified, starting from the insertion of the nerve near the cricothyroid muscle and continuing to where it ran down along the tracheo-esophageal groove (Fig. 2F). After the recurrent laryngeal nerve was fully exposed, Berry's ligament dissection, inferior thyroid vessel ligation, and ipsilateral central node dissection could be performed in the same view (Fig. 2G). The signal of recurrent laryngeal nerve was checked by using a nerve stimulator connected with an endoscopic hook. In the case shown in Fig. 2H, both the upper and lower parathyroid glands shown in the thyroidectomy field and recurrent laryngeal nerve were intact after lobectomy. Fig. 3 shows the postoperative surgical field after right thyroid lobectomy. The resected thyroid and central nodes were extracted through the 11-mm port within a laparoscopic bag. A surgical drain was placed through a small skin puncture of the anterior neck. Oral wounds were closed by applying interrupted sutures with absorbable string.
Patients underwent oral examinations before surgery, history taking, and inspection by the surgeon in the outpatient department. All patients received intravenous prophylactic antibiotics (Oxacephem; a third-generation cephalosporin) 1 hour before surgery. Patients received oral antibiotics (amoxicillin/clavulanate, 625 mg, 3 times per day) after surgery during postoperative day 7. In the morning of postoperative days 1, 2, and 3, the patients were asked to score their pain by using a visual analogue scale (VAS). The test was administered and recorded by trained nurses. In cases where we simultaneously performed TOETVA with other organ surgery, the VAS scores that related to the different surgical sites were recorded separately.
All patients started an oral diet on postoperative day 1 with a soft fluid diet. On postoperative day 2, the patients started a soft blended diet or a normal regular diet depending on patient's preference. Patients could be discharged after postoperative day 3. Oral wound stitches were removed in outpatient clinic 1 week after surgery. Vocal cord function was evaluated by using traditional laryngoscopy or laryngeal ultrasonography [21]. Hypocalcemia was defined as a serum calcium level below the normal range (Ca < 8.8 mg/dL) or clinical symptoms that required calcium supplementation. Hypoparathyroidism was defined as a serum parathyroid hormone (PTH) level < 15 pg/mL in the postoperative period. Mental nerve injury was defined as sensory change, drooling, or numbness around the chin. All cases were assessed by JWY at first outpatient visit after 2 weeks.
The clinical characteristics of the 20 TOETVA patients are described in Table 1. Median follow-up period was 4 months. Mean age was 50.8 ± 11.3 years, 19 patients were female, and 1 was male. Preoperative fine needle aspiration cytology examinations revealed PTC or a follicular neoplasm. Lobectomies were performed in 12 cases (right in 9, left in 3) and total thyroidectomy was performed in 7 patients. Wide isthmectomy was performed in 1 patient. Ipsilateral or bilateral central node dissection was done in all cases according to tumor location. The mean operation time was 152 ± 51.4 minutes. The mean operation time of lobectomy and total thyroidectomy was 145.4 ± 55.7, 164.3 ± 43.5 respectively. The longest operation time was 250 minutes and was caused by severe adhesion of the thyroid, but there was no postoperative emphysema. Mean hospital stay after operation was 4.7 ± 3.8 days (range, 3–20 days). Mean hospital stay after lobectomy was 5.2 ± 4.5 days and after total thyroidectomy was 3.7 ± 1.5 days (Table 1). One patient developed wound seroma after right lobectomy and stayed in the hospital 20 days after surgery.
According to the pathologic report, tumor size ranged from 0.2–1.4 cm and the mean number of retrieved central lymph nodes was 2.8 ± 2.6. Two out of 7 thyroidectomy patients had lymph node metastasis (Table 1). Sixteen patients had classical PTC and 4 had follicular variant PTC. Twelve patients had an extrathyroidal extension. All surgical margins were negative for tumor.
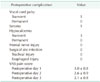
Intraoral wounds almost completely healed one or 2 weeks after surgery (Fig. 4). The postoperative outcomes are shown in Table 2. One patient had transient vocal cord palsy but recovered after 3 months. One patient developed neck seroma after postoperative day 2 and was treated by percutaneous drainage. None of the 20 patients had mental nerve injury or surgical site infection. One patient developed transient hypocalcemia that improved after 1 month. Postoperative days 1, 2, and 3 VAS scores were 3.0 ± 0.8, 2.6 ± 0.9, and 2.1 ± 0.8, respectively.
In the early 21st century, various surgical treatments started using the NOTES method, although initially the main focus was in gastrointestinal surgery [7]. In 2008, an Austrian group reported the first study on the feasibility and safety of NOTES in thyroid surgery: they used the transoral sublingual route to access the thyroid in 2 human cadavers and 10 living pigs [8]. Thereafter, endocrine surgeons conducted a variety of studies in cadaver or animal models with the aim of developing a safe and feasible transoral thyroidectomy method [91222]. In 2011, a German group reported the first study on transoral thyroid surgery with patients [13]. However, complication rate in the 8 patients was very high: 87.5% (n = 7) had mental nerve palsy and 12.5% (n = 1) had permanent recurrent laryngeal nerve injury. In 2013, a Japanese group reported another transoral approach in humans using a single 2.5-cm incision in the oral vestibule with the neck skin lift method [10]. Again, the complication rate was high: all 8 patients developed sensory disorders around the chin that persisted until at least 6 months after surgery. However, in 2014, a Chinese group reported the results of a randomized clinical trial comparing their transoral method with the areola method [14]. They used three vestibular incisions to avoid mental nerve injury. This was the first human clinical study to report no severe complications using the transoral approach.
A report published in 2016 reported the successful implementation of transoral thyroid surgery, termed TOETVA, in humans [15]. Sixty TOETVA surgeries using the tri-vestibular approach were performed; 1 middle 10-mm incision for the camera and 2 lateral 5-mm incisions for instruments. All surgeries proceeded uneventfully and there were no worrisome complications such as recurrent laryngeal or mental nerve injury or surgical site infections. Recently, this group also reported the results of TOETVA in 45 patients with Graves' disease. Serious complications were not observed and the patients had lower VAS pain scores than 49 patients who underwent open surgery for Graves' disease [23]. After the pioneering 2 reports in 2016, many hospitals worldwide have started to adopt transoral thyroid surgery [17181924]. In terms of thyroid surgery, the most important complications were recurrent laryngeal nerve injury and hypoparathyroidism. Additional complications associated with TOETVA were mental nerve injury and surgical site infection, reported in a previous study in 2011 [13]. In our study, transient vocal cord palsy and transient hypocalcemia occurred only in 1 patient. None of the patients developed mental nerve injury or surgical site infection. According to our initial results, TOETVA is acceptable with respect to short term surgical outcomes, as described in Table 2.
The greatest advantage of TOETVA is the absence of the need for a skin incision. Other remote access surgery methods, e.g., trasaxillary and BABA, still require skin incisions in the axillary fold or areolar. After TOETVA, wounds are invisible because they are hidden in the oral cavity. Moreover, oral mucosal wounds almost completely healed 1–2 weeks after surgery. Scars were not observed after oral stitches were taken out. The second advantage of TOETVA is that it causes less pain than traditional surgical approaches. In our case series, mean VAS scores for pain on postoperative days 1, 2, and 3 were 3.0, 2.6, and 2.1, respectively. In a previous study performed at our institution, mean VAS scores 1, 2, and 3 days after open thyroidectomy were 4.6, 3.50, 2.4, respectively. And mean VAS scores 1, 2, and 3 days after BABA thyroidectomy were 5.0, 4.0, 2.7, respectively [25]. The lower pain scores of our series probably reflects the fact that TOETVA does not make skin incisions and the flap dissection area is narrower than that in open or other remote access surgical methods. Another advantage of TOETVA is that it is cheaper than robot-assisted surgery because it only involves conventional endoscopic devices [15].
Despite these findings, additional research is needed before TOETVA can be accepted as an orthodox method for PTC. Oncological outcome is the most important issue in cancer surgery. Follow-up duration of TOETVA is shorter than that of other remote access endoscopic or robotic surgery methods. To assure the oncological safety of TOETVA, it will be necessary to build up a prospectively recruited large-scale cohort to check Thyroglobulin (TG) or thyroid stimulating hormone stimulated thyroglobulin (off-TG) levels after total thyroidectomy, as used in previous transaxillary and BABA methods [262728]. Another issue is surgical site infection. Although traditional thyroid surgery is considered as clean surgery, TOETVA is considered as clean-contaminated surgery due to the oral cavity access. To prevent possible surgical site infection in the thyroidectomy area, our institution prescribes oral antibiotics for 7 days after surgery. Other institutions use oral antibiotics for 3–7 days after surgery [151823]. Further studies are needed to determine the proper antibiotics dosage or duration after TOETVA. The technical limitations of TOETVA are related to the fact that it is a cephalo-caudal approach; thus, it has a limited view in the deep portion of the upper pole. If the upper pole is extended by a tumor mass or if the tumor located in the upper pole, complete removal of the thyroid cannot be achieved.
In summary, our institution has successfully implemented TOETVA for surgery on selected PTC patients. Cosmetic outcomes were excellent and surgical complications were acceptable. Large-scale long follow-up prospective studies are needed to prove the oncological safety of TOETVA.
Figures and Tables
 | Fig. 1Incision and trocar placement in the transoral endoscopic thyroidectomy vestibular approach. (A) Vestibular incisions (yellow lines). (B) Placement of the trocars. |
 | Fig. 2Thyroidectomy procedures in TOETVA. Representative images were taken from a single patient's transoral endoscopic right lobectomy procedure. (A) Strap muscle was divided on the midline and (B) isthmus was cut from the superior aspect. (C) After right lobe mobilization, the middle thyroid vein was ligated. (D) Dissection and division of the superior pole was performed using an ultrasonic device. After that, (E) the right upper parathyroid was identified and saved. (F) Right recurrent laryngeal nerve was identified and (G) Berrys ligament dissection with en bloc central node dissection was done. (H) The recurrent laryngeal nerve signal was checked using a nerve stimulator after thyroidectomy. T, trachea; I, isthmus; SN, sternal notch; RT, right thyroid; MTV, middle thyroid vein; SP, superior pole; CTM, cricothyroid muscle; UP, upper parathyroid; LP, lower parathyroid; RLN, recurrent laryngeal nerve; B, ligament of Berry; VI, level VI central node area; NS, nerve stimulator. |
 | Fig. 3Postoperative surgical field after right lobectomy. T, trachea; CTM, cricothyroid muscle; UP, upper parathyroid; LP, lower parathyroid; RLN, recurrent laryngeal nerve. |
 | Fig. 4Cosmetic outcomes at 2 weeks after surgery. (A) Anterior view of the patient's neck with neck extension. (B) The oral vestibule wounds healed without complications. |
References
1. Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R. Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J Cancer Epidemiol. 2013; 2013:965212.

2. Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. Trends in thyroid cancer incidence and mortality in the United States, 1974-2013. JAMA. 2017; 317:1338–1348.

3. Duncan TD, Rashid Q, Speights F, Ejeh I. Endoscopic transaxillary approach to the thyroid gland: our early experience. Surg Endosc. 2007; 21:2166–2171.

4. Kang SW, Jeong JJ, Yun JS, Sung TY, Lee SC, Lee YS, et al. Robot-assisted endoscopic surgery for thyroid cancer: experience with the first 100 patients. Surg Endosc. 2009; 23:2399–2406.

5. Lee KE, Koo do H, Kim SJ, Lee J, Park KS, Oh SK, et al. Outcomes of 109 patients with papillary thyroid carcinoma who underwent robotic total thyroidectomy with central node dissection via the bilateral axillo-breast approach. Surgery. 2010; 148:1207–1213.

6. Choe JH, Kim SW, Chung KW, Park KS, Han W, Noh DY, et al. Endoscopic thyroidectomy using a new bilateral axillo-breast approach. World J Surg. 2007; 31:601–606.

7. Rattner D, Kalloo A. ASGE/SAGES Working Group. ASGE/SAGES Working Group on Natural Orifice Translumenal Endoscopic Surgery. October 2005. Surg Endosc. 2006; 20:329–333.
8. Witzel K, von Rahden BH, Kaminski C, Stein HJ. Transoral access for endoscopic thyroid resection. Surg Endosc. 2008; 22:1871–1875.

9. Benhidjeb T, Wilhelm T, Harlaar J, Kleinrensink GJ, Schneider TA, Stark M. Natural orifice surgery on thyroid gland: totally transoral video-assisted thyroidectomy (TOVAT): report of first experimental results of a new surgical method. Surg Endosc. 2009; 23:1119–1120.

10. Nakajo A, Arima H, Hirata M, Mizoguchi T, Kijima Y, Mori S, et al. Trans-oral video-assisted neck surgery (TOVANS). A new transoral technique of endoscopic thyroidectomy with gasless premandible approach. Surg Endosc. 2013; 27:1105–1110.

11. Guo P, Tang Z, Ding Z, Chu G, Yao H, Pan T, et al. Transoral endoscopic thyroidectomy with central neck dissection: experimental studies on human cadavers. Chin Med J (Engl). 2014; 127:1067–1070.
12. Karakas E, Steinfeldt T, Gockel A, Schlosshauer T, Dietz C, Jager J, et al. Transoral thyroid and parathyroid surgery--development of a new transoral technique. Surgery. 2011; 150:108–115.

13. Wilhelm T, Metzig A. Endoscopic minimally invasive thyroidectomy (eMIT): a prospective proof-of-concept study in humans. World J Surg. 2011; 35:543–551.

14. Wang C, Zhai H, Liu W, Li J, Yang J, Hu Y, et al. Thyroidectomy: a novel endoscopic oral vestibular approach. Surgery. 2014; 155:33–38.

15. Anuwong A. Transoral endoscopic thyroidectomy vestibular approach: a series of the first 60 human cases. World J Surg. 2016; 40:491–497.

16. Dionigi G, Bacuzzi A, Lavazza M, Inversini D, Pappalardo V, Boni L, et al. Transoral endoscopic thyroidectomy via vestibular approach: operative steps and video. Gland Surg. 2016; 5:625–627.

17. Park JO, Kim MR, Kim DH, Lee DK. Transoral endoscopic thyroidectomy via the trivestibular route. Ann Surg Treat Res. 2016; 91:269–272.

18. Wang Y, Yu X, Wang P, Miao C, Xie Q, Yan H, et al. Implementation of intraoperative neuromonitoring for transoral endoscopic thyroid surgery: a preliminary report. J Laparoendosc Adv Surg Tech A. 2016; 26:965–971.

19. Dionigi G, Bacuzzi A, Lavazza M, Inversini D, Boni L, Rausei S, et al. Transoral endoscopic thyroidectomy: preliminary experience in Italy. Updates Surg. 2017; 69:225–234.

20. Dionigi G, Lavazza M, Bacuzzi A, Inversini D, Pappalardo V, Tufano RP, et al. Transoral endoscopic thyroidectomy vestibular approach (TOETVA): from A to Z. Surg Technol Int. 2017; 30:103–112.
21. Woo JW, Suh H, Song RY, Lee JH, Yu HW, Kim SJ, et al. A novel lateral-approach laryngeal ultrasonography for vocal cord evaluation. Surgery. 2016; 159:52–56.

22. Miccoli P, Materazzi G, Berti P. Natural orifice surgery on the thyroid gland using totally transoral video-assisted thyroidectomy: report of the first experimental results for a new surgical method: are we going in the right direction? Surg Endosc. 2010; 24:957–958.

23. Jitpratoom P, Ketwong K, Sasanakietkul T, Anuwong A. Transoral endoscopic thyroidectomy vestibular approach (TOETVA) for Graves’ disease: a comparison of surgical results with open thyroidectomy. Gland Surg. 2016; 5:546–552.

24. Udelsman R, Anuwong A, Oprea AD, Rhodes A, Prasad M, Sansone M, et al. Transoral vestibular endocrine surgery: a new technique in the United States. Ann Surg. 2016; 264:e13–e16.
25. Chai YJ, Song J, Kang J, Woo JW, Song RY, Kwon H, et al. A comparative study of postoperative pain for open thyroidectomy versus bilateral axillo-breast approach robotic thyroidectomy using a self-reporting application for iPad. Ann Surg Treat Res. 2016; 90:239–245.

26. Son SK, Kim JH, Bae JS, Lee SH. Surgical safety and oncologic effectiveness in robotic versus conventional open thyroidectomy in thyroid cancer: a systematic review and meta-analysis. Ann Surg Oncol. 2015; 22:3022–3032.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download