This article has been
cited by other articles in ScienceCentral.
A 77-year-old woman, who had undergone coronary stent implantation at the proximal left anterior descending artery 30 months ago, presented with a large anterior left ventricle (LV) aneurysm. Chest X-ray revealed a soft tissue density measuring 7×5 cm, merging with the left heart border (
Figure 1). Computed tomography (CT) scan (
Figure 2) and echocardiography (
Figure 3) showed a very large aneurysmal dilatation of the anterior wall of the mid cavity of the LV without any thrombus. The patient underwent LV aneurysmectomy. A part of the huge aneurysm, approximately 3 cm in diameter, showed dense adhesion with the pericardium (
Figure 4A). The surrounding part of the adhesion was rather thin, almost translucent, as if there was no sign of endomyocardial layer (
Figure 4B). As the large pseudoaneurysmal change developed without well-defined edges, the myocardial layer surrounding the beginning of the aneurysmal sac was most likely pulled outward slightly along with the growing outpouching. The large anatomical defect was closed with Dacron patch (
Figure 4C). Postoperative CT scan showed the successful exclusion of the pseudoaneurysm and reconstruction of the LV (
Figure 5). She was discharged on postoperative day 11 with no neurological or cardiovascular sequelae.
A pseudoaneurysm of the LV develops after an acute myocardial infarction (AMI) that is complicated by incomplete rupture of the heart when organizing thrombus, hematoma, and pericardium seal a rupture of the LV.
1)2) LV pseudoaneurysm after AMI is life-threatening due to the high risk of acute rupture and therefore early surgical intervention is usually recommended.
1)2) However, about 10% of all cases are asymptomatic and some of them can develop into chronic pseudoaneurysm in which the anatomical defect is usually bigger and without well-defined edges (atypical form).
2)3) Some authors suggest that chronic LV pseudoaneurysms might be followed conservatively.
4) However, as for chronic LV pseudoaneurysm, we believe that surgery should be recommended in symptomatic patients or in those with a large (>3 cm) or gradually enlarging pseudoaneurysm.
5)
Figures and Tables
Figure 1
Preoperative chest X-ray shows a soft tissue density measuring 7×5 cm merging with the left heart border.
Figure 2
Preoperative CT scan shows a large saccular-appearing outpouching of the LV measuring 66×66×55 mm.
CT = computed tomography; LV = left ventricle.
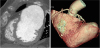
Figure 3
Echocardiography shows a large saccular-appearing outpouching of the LV.
LV = left ventricle.

Figure 4
Operative findings. (A) A part of the aneurysm showed dense adhesion with the pericardium; (B) a large aneurysm: a very thin and fibrotic wall through incised sac; and (C) the large anatomical defect was excluded with an oval Dacron patch.

Figure 5
Postoperative CT scan shows a successful reconstruction of the LV.
CT = computed tomography; LV = left ventricle.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download