RESULTS
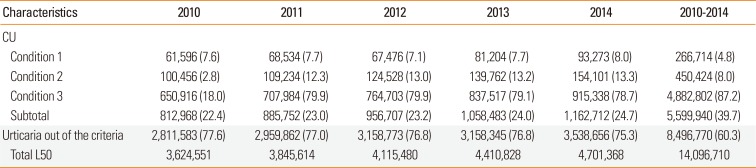
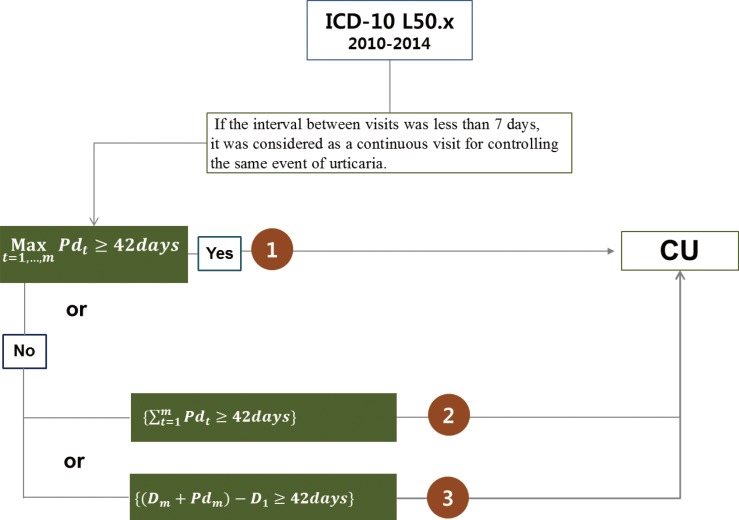
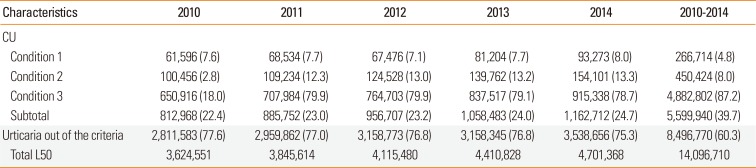
There were 14,096,710 cases under the diagnostic codes of urticaria (ICD-10 code of L50) from 2010 to 2014 recorded in the HIRA database. In accordance with the stated criteria for determining CU (
Fig. 1), 39.7% (5,599,940) of all cases were classified as having CU over the 5-year period (
Table 1). Of all CU cases, 4.8% were obtained by the first criterion, 8.0% by the second criterion, and 87.2% by the third criterion (266,714 vs 450,424 vs 4,882,802 cases, respectively). The annual CU ratio of total patients having urticaria was on average 23.5% over the 5-year study period.
Table 1
Prevalence of chronic urticaria according to the algorithm
|
Characteristics |
2010 |
2011 |
2012 |
2013 |
2014 |
2010-2014 |
|
CU |
|
|
|
|
|
|
|
Condition 1 |
61,596 (7.6) |
68,534 (7.7) |
67,476 (7.1) |
81,204 (7.7) |
93,273 (8.0) |
266,714 (4.8) |
|
Condition 2 |
100,456 (2.8) |
109,234 (12.3) |
124,528 (13.0) |
139,762 (13.2) |
154,101 (13.3) |
450,424 (8.0) |
|
Condition 3 |
650,916 (18.0) |
707,984 (79.9) |
764,703 (79.9) |
837,517 (79.1) |
915,338 (78.7) |
4,882,802 (87.2) |
|
Subtotal |
812,968 (22.4) |
885,752 (23.0) |
956,707 (23.2) |
1,058,483 (24.0) |
1,162,712 (24.7) |
5,599,940 (39.7) |
|
Urticaria out of the criteria |
2,811,583 (77.6) |
2,959,862 (77.0) |
3,158,773 (76.8) |
3,158,345 (76.8) |
3,538,656 (75.3) |
8,496,770 (60.3) |
|
Total L50 |
3,624,551 |
3,845,614 |
4,115,480 |
4,410,828 |
4,701,368 |
14,096,710 |

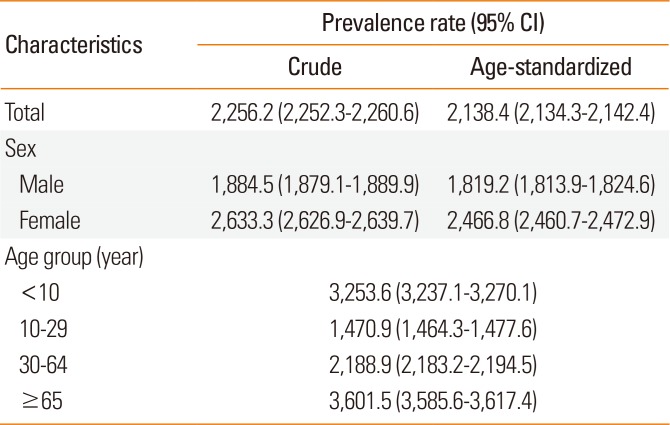
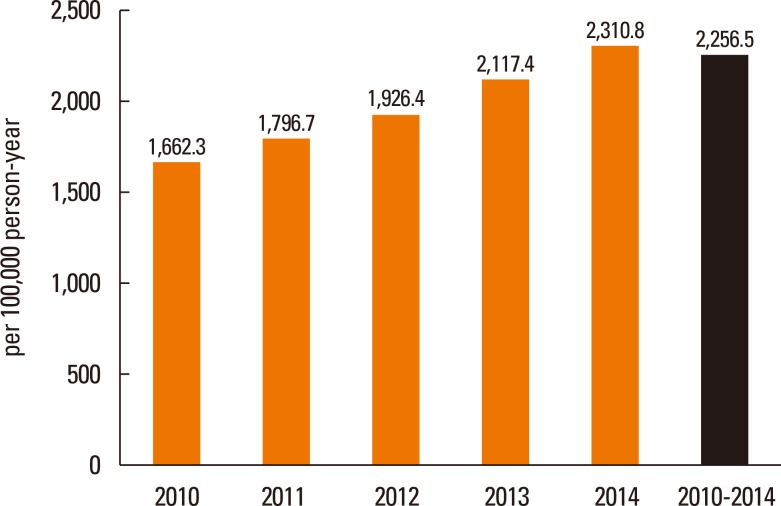
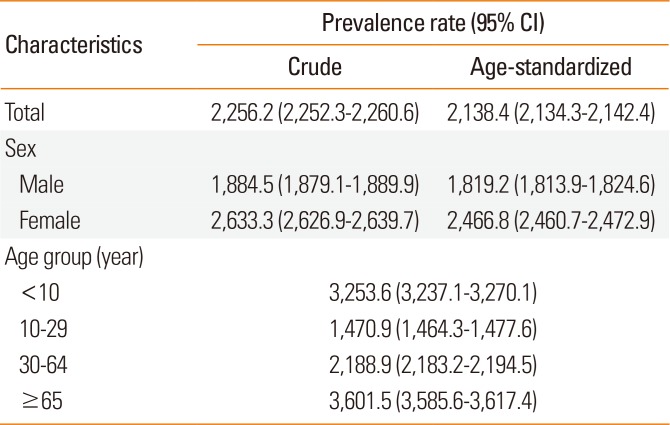
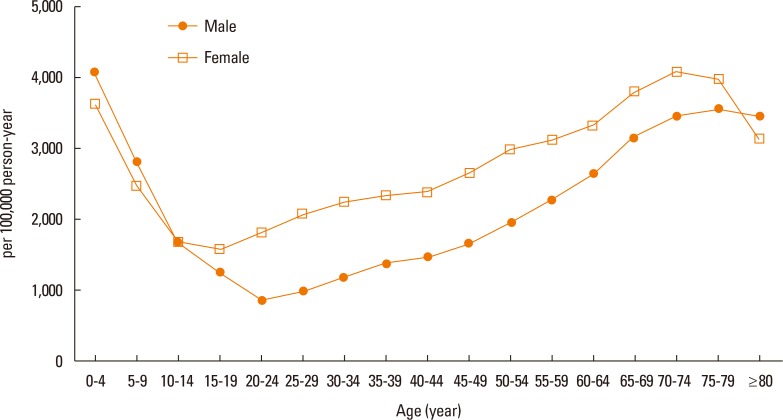
The crude prevalence of CU was 2,256.5 (95% CI, 2,252.3–2,260.6) per 100,000 person-years (
Fig. 2). The annual prevalence of CU consistently increased from 1,662.3 per 100,000 persons in 2010 to 2,310.8 per 100,000 persons in 2014 (
Fig. 2). For 2010–2014, the age-adjusted prevalences of CU were 2,138.4 (2,134.3–2,142.4) per 100,000 person-years overall, 1,819.2 (1,813.9–1,824.6) per 100,000 person-years among men, and 2,466.8 (2,460.7–2,472.9) per 100,000 person-years among women (
P<0.001,
Table 2). The age-specific prevalence of CU was highest in older adults over the age of 65 years and lowest in ages 10–29 years. The age-specific prevalence of urticaria that did meet our set of criteria for CU was highest in children younger than 10 years. Chi-square tests for analyzing trends revealed significantly different prevalence rates of CU among age groups (
Table 2,
P<0.001).
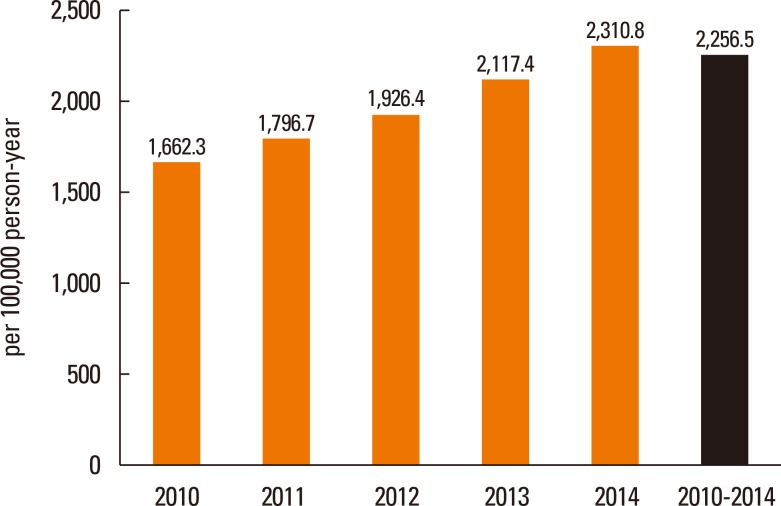 | Fig. 2Crude prevalence of CU (per 100,000 person-years) over a 5-year period. There was a significant linear trend in the crude prevalence of CU over the 5-year period (P<0.001). CU, chronic urticaria. 
|
Table 2
Prevalence of chronic urticaria (per 100,000 person-years) by age and sex
|
Characteristics |
Prevalence rate (95% CI) |
|
Crude |
Age-standardized |
|
Total |
2,256.2 (2,252.3–2,260.6) |
2,138.4 (2,134.3–2,142.4) |
|
Sex |
|
|
|
Male |
1,884.5 (1,879.1–1,889.9) |
1,819.2 (1,813.9–1,824.6) |
|
Female |
2,633.3 (2,626.9–2,639.7) |
2,466.8 (2,460.7–2,472.9) |
|
Age group (year) |
|
|
|
<10 |
3,253.6 (3,237.1–3,270.1) |
|
10–29 |
1,470.9 (1,464.3–1,477.6) |
|
30–64 |
2,188.9 (2,183.2–2,194.5) |
|
≥65 |
3,601.5 (3,585.6–3,617.4) |

The prevalence of CU according to sex also differed according to age (
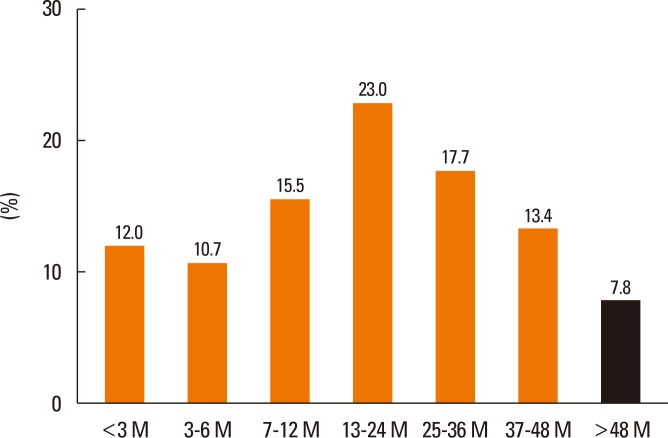
Fig. 3), that is, the prevalence of CU was higher in boys than in girls among children under the age of 10 years, although it was significantly higher in females than in males among adolescent and adults older than 15 years. The median duration of urticaria was estimated as 591 days, with an interquartile range of 256–1,054 in CU patients. Among CU patients, the durations of prescription medications were shorter than 3 months in 12.0%, from 3 to 12 months in 26.2%, from 12 to 24 months in 23.0%, from 24 to 36 months in 17.7%, from 36 to 48 months in 13.4%, and longer than 48 months in 7.8% (
Fig. 4).
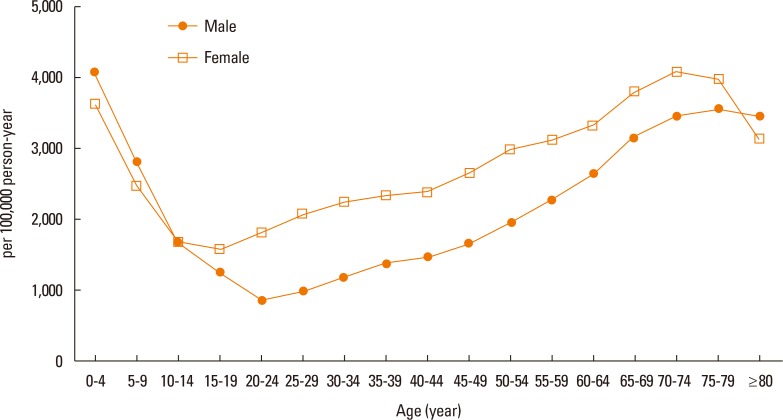 | Fig. 3The prevalence of CU (per 100,000 person-years) specific to age and sex. CU, chronic urticaria. 
|
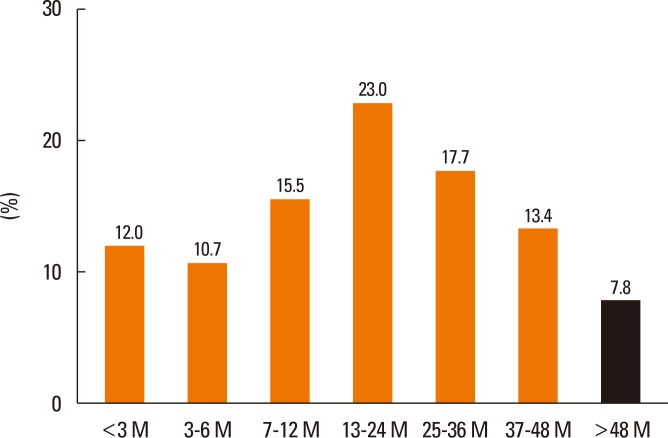 | Fig. 4Distribution of CU patients according to urticaria duration. M, month; CU, chronic urticaria. 
|
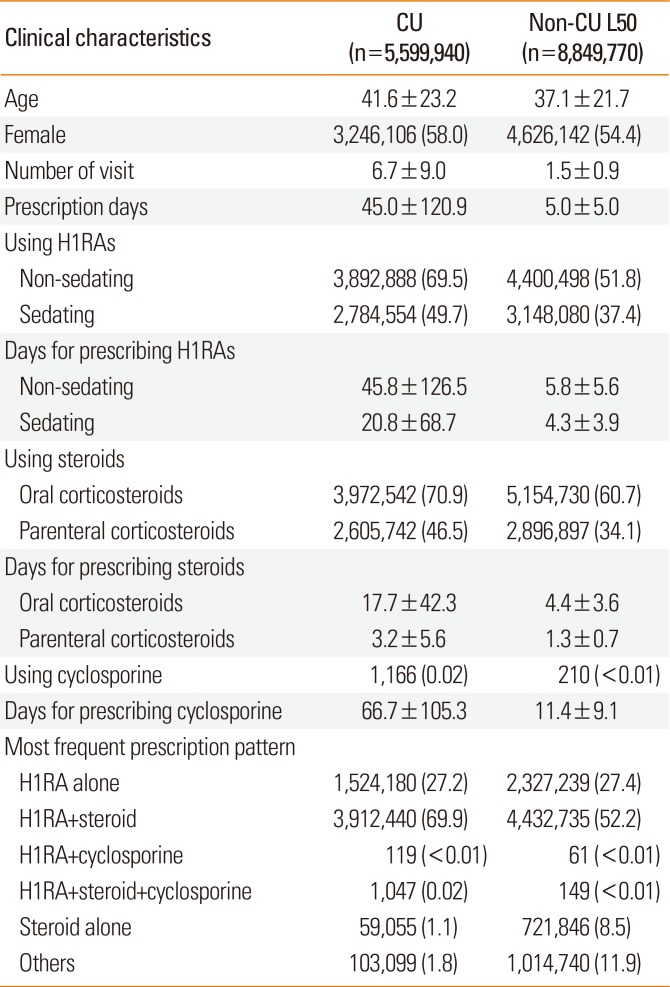
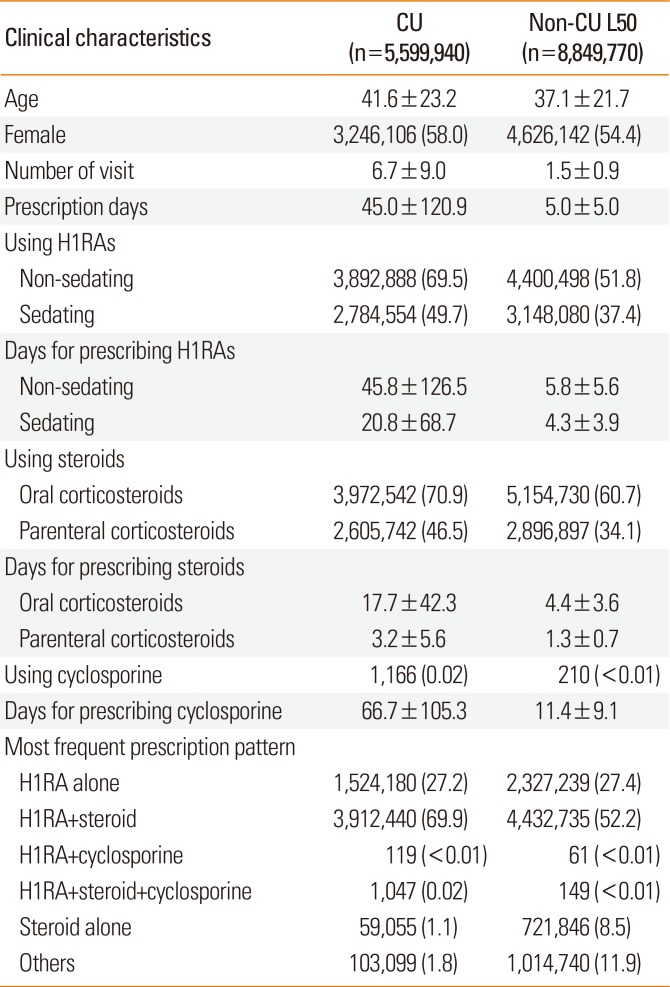
Table 3 depicts the clinical characteristics of and medication prescription days and patterns in patients with CU. The mean age of the CU patients was 41.6±23.2 years. CU patients visited medical clinics on an average of 6.7 times and took medicines for a mean of 45.0 days. Of all CU patients, 27.2% were prescribed antihistamines alone, and 69.9% received combined medicines with antihistamines and systemic corticosteroids. Among patients receiving antihistamines, 49.7% were given sedating antihistamines, and 69.7% were prescribed non-sedating antihistamines. Mean days for prescribing antihistamines were significantly higher with non-sedating antihistamines, compared to sedating antihistamines (45.8±126.5 vs 20.8±68.7 days,
P<0.001). Mean days for supply of systemic corticosteroids differed from 3.2±5.6 days for parenteral corticosteroids to 17.7±42.3 days for oral corticosteroids (
P<0.001). In contrast, cyclosporine was prescribed only for 0.02% of CU patients. Mean prescription days for cyclosporine reached 66.7±105.3 days over the 5-year study period.
Table 3
Clinical characteristics and medication prescription patterns in patients with chronic urticaria in comparison to patients with urticaria that not fulfill CU criteria
|
Clinical characteristics |
CU (n=5,599,940) |
Non-CU L50 (n=8,849,770) |
|
Age |
41.6±23.2 |
37.1±21.7 |
|
Female |
3,246,106 (58.0) |
4,626,142 (54.4) |
|
Number of visit |
6.7±9.0 |
1.5±0.9 |
|
Prescription days |
45.0±120.9 |
5.0±5.0 |
|
Using H1RAs |
|
|
|
Non-sedating |
3,892,888 (69.5) |
4,400,498 (51.8) |
|
Sedating |
2,784,554 (49.7) |
3,148,080 (37.4) |
|
Days for prescribing H1RAs |
|
|
|
Non-sedating |
45.8±126.5 |
5.8±5.6 |
|
Sedating |
20.8±68.7 |
4.3±3.9 |
|
Using steroids |
|
|
|
Oral corticosteroids |
3,972,542 (70.9) |
5,154,730 (60.7) |
|
Parenteral corticosteroids |
2,605,742 (46.5) |
2,896,897 (34.1) |
|
Days for prescribing steroids |
|
|
|
Oral corticosteroids |
17.7±42.3 |
4.4±3.6 |
|
Parenteral corticosteroids |
3.2±5.6 |
1.3±0.7 |
|
Using cyclosporine |
1,166 (0.02) |
210 (<0.01) |
|
Days for prescribing cyclosporine |
66.7±105.3 |
11.4±9.1 |
|
Most frequent prescription pattern |
|
|
|
H1RA alone |
1,524,180 (27.2) |
2,327,239 (27.4) |
|
H1RA+steroid |
3,912,440 (69.9) |
4,432,735 (52.2) |
|
H1RA+cyclosporine |
119 (<0.01) |
61 (<0.01) |
|
H1RA+steroid+cyclosporine |
1,047 (0.02) |
149 (<0.01) |
|
Steroid alone |
59,055 (1.1) |
721,846 (8.5) |
|
Others |
103,099 (1.8) |
1,014,740 (11.9) |

To determine the accuracy of our algorithms for identifying CU patients, we investigated mean number of visits, mean duration of prescription medications, and number of cyclosporine users among patients who did not fulfill the criteria for CU. They had visited clinics under a primary diagnosis of urticaria 1.5 times as a mean, with 5.0 days of prescription medication use (
Table 3). Only 210 (<0.01%) of 8,496,770 patients in the non-CU group had been prescribed cyclosporine. These findings indicated that most of the patients that did not fulfill the criteria for CU in the present study might be patients with acute urticaria.
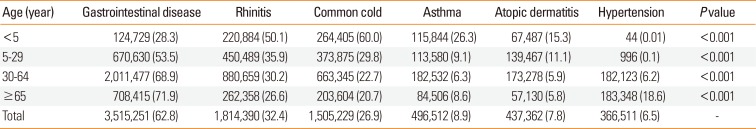
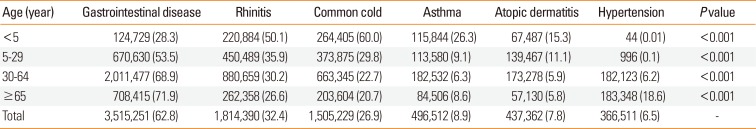
The most common comorbidities in CU patients were gastrointestinal disease, allergic rhinitis, and common cold (62.8% vs 32.4% vs 26.9%, respectively,
Table 4). In adults, especially those older than 30 years, gastrointestinal disease was the most common comorbid disorder (age of 30–64, 68.9%; ≥65, 71.9%). Meanwhile, however, allergic rhinitis (50.1%) and common cold (60.0%) were the most prevalent diseases in children, especially in those younger than 5 years.
Table 4
Age-specific comorbidities of patients with chronic urticaria
|
Age (year) |
Gastrointestinal disease |
Rhinitis |
Common cold |
Asthma |
Atopic dermatitis |
Hypertension |
P value |
|
<5 |
124,729 (28.3) |
220,884 (50.1) |
264,405 (60.0) |
115,844 (26.3) |
67,487 (15.3) |
44 (0.01) |
<0.001 |
|
5–29 |
670,630 (53.5) |
450,489 (35.9) |
373,875 (29.8) |
113,580 (9.1) |
139,467 (11.1) |
996 (0.1) |
<0.001 |
|
30–64 |
2,011,477 (68.9) |
880,659 (30.2) |
663,345 (22.7) |
182,532 (6.3) |
173,278 (5.9) |
182,123 (6.2) |
<0.001 |
|
≥65 |
708,415 (71.9) |
262,358 (26.6) |
203,604 (20.7) |
84,506 (8.6) |
57,130 (5.8) |
183,348 (18.6) |
<0.001 |
|
Total |
3,515,251 (62.8) |
1,814,390 (32.4) |
1,505,229 (26.9) |
496,512 (8.9) |
437,362 (7.8) |
366,511 (6.5) |
- |

Go to :

DISCUSSION
The present study represents the first nationwide epidemiological study on CU in Korea. Between 2010 and 2014, an estimated age-adjusted prevalence of 2,138.4 (95% CI, 2,134.3–2,142.4) per 100,000 person-years in CU was obtained using a nationwide database in Korea. The annual prevalence of CU has been increasing year by year, and the overall ratio of CU among all urticaria patients was on average 23.5% over the 5-year study period. Age-specific prevalence showed 2 peaks in children younger than 10 years old and older adults aged 65 years and older. Female predilection of CU was also noted in patients older than 15 years in the present study, whereas in those younger than 10 years, a significantly higher prevalence of CU was found in boys than in girls.
Although study populations and methods vary among studies, estimates in previous reports on the prevalence of CU have ranged from 0.05% to 3.0%.
7 A prior questionnaire survey conducted among the general population of Germany revealed a lifetime prevalence for CU of 1.8% and a period prevalence of 0.8% for active CU within the past 12 months.
7 The authors of another study in Spain utilized a similar questionnaire survey to estimate the real prevalence of CU in the adult general population. While they found a 0.6% prevalence of active CU, 2.9% of the nationwide sample of adults was recognized as having had urticaria for more than 6 weeks.
8 As these questionnaires-based population studies are dependent on the patients' participation and memories, there might be recall bias and limitations of fewer respondents among children and older adults. Therefore, the CU prevalence covering 5 years in Korea would be comparable to the lifetime prevalence of 1.8% and 2.9% for German
7 and Italian
8 populations.
Similar to the present study, recent studies have also used insurance claims databases to investigate the prevalence of chronic spontaneous urticaria (CSU).
910 Zazzali et al.
9 adopted algorithms for defining CSU as the presence of at least one outpatient International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) code of 708.1, 708.8, or 708.9 and a second diagnosis of the same codes later than 6 weeks from 2010 to 2013, the presence of angioedema (ICD-9-CM code of 995.1) for at least 6 weeks from the urticaria diagnosis, or 90-day use of prescription medications for treating CSU, such as antihistamine and montelukast, cyclosporine, methotrexate, or oral corticosteroids. They identified an estimated 1-year period prevalence of 0.08% for CSU.
9 The proportions of CU patients were dependent on the 3 different conditions target by our algorithms. Of all patients with CU, 87.2% were selected by condition 3, followed by conditions 2 (8.0%) and 1 (4.8%). These are consistent with prior results by Zazzali et al.
9 in that a second urticaria claim at 6 weeks or later was the most common reason for inclusion (82.2%) as a patient with CU, followed by days of prescription medications used to treat CSU (16.7%). Lapi et al.
10 used similar algorithms as those in the aforementioned study for patients aged ≥15 years between 2002 and 2013 in Italy. Therein, the annual prevalence of CSU ranged from 0.02% in 2002 to 0.38% in 2013.
10 According to the literature, of patients having non-acute urticaria, 66%–93% have been found to have CSU.
3 Since we selected all patients with urticaria, regardless of their etiologies and ages, the age-adjusted prevalence rate of CU of 2,138.4 per 100,000 person-years over a 5-year of study period was a little higher than rates in previous reports limited to CSU.
910 Moreover, differences in ethnicity, geographic distributions, and criteria for identifying CU may have also contributed to the variations in the prevalence of CU among different studies. Because the criteria for selecting CU in our study did not consider the presence of angioedema and focused on the use of antihistamines, it would be difficult to extrapolate the prevalence of CSU for the Korean population based on the present results. Further studies using previous validated algorithms
9 for CSU are needed to confirm whether the real prevalences of CSU, as well as CU, are higher in Korea than in other countries.
Consistent with other studies, we confirmed that the age-adjusted prevalence of CU was higher in females than in males among adults older than 15 years: 66.7% in the US,
9 63% in Israel,
11 69.8% in Turkey,
12 70.3% in Germany,
7 and 79% in Thailand.
13 Considering that autoimmune mechanisms are involved in about half of all CU cases, a female predilection in the prevalence of CU is acceptable, as it is a common feature in various autoimmune disorders.
14 However, we found that in children younger than 10 years, the prevalence of CU was significantly higher in boys than in girls. A recent questionnarire-based study on Korean children also reported a higher prevalence of CU in boys, although no statistical significance was noted.
15 Furthermore, differences in other allergic diseases between boys and girls have been shown by other studies,
1617 in which, compared with girls, boys show higher incidences of asthma, allergic rhinitis, and anaphylaxis during childhood.
In general, the peak incidence of CU is observed between 20 and 40 years of age.
31318 The mean age of CU patients was 41.6 years in Korea from 2010 to 2014 in the present study. In a previous claims-based research on CU epidemiology in the US, the mean age of the patients was 41.0 years, the same as that in the present study. A recent cross-sectional study using questionnaires reported that the prevalence of CU in children aged from 4 to 13 years was 1.8% in Korea.
15 This is in line with the present results that approximately 3.2% (3,253.6 per 100,000 person-years) in children aged less than 10 years and around 1.5% (1,470.9 per 100,000 person-years) in 10–29 years were estimated as CU patients. Meanwhile, previous retrospective observational studies or phone surveys have found the age group of 45 to 64 years to show the highest prevalence of CU.
7819 However, we found that the prevalence of CU was higher in patients over the age of 65 years and younger than 10 years, compared to other age groups. In agreement with our results, a recent population-based study using claims data in Italy indicated that, based on the prevalence of CU in individuals younger than 20 years, the adjusted hazard ratio of CU increased significantly in patients aged 60–79 years, while it was significantly decreased in patients of ages 20–29 and 30–39 years.
10 However, our results are limited in that information on over-the-counter medications was not available for analysis in the present study, nor in the previous Italian studies. Considering that younger individuals, particularly those of ages from 20 to 40 years are more prone to take over-the-counter antihistamines, we could not simply conclude that the prevalence of CU is higher in older adults than in middle-aged adults. In order to clarify epidemiological results on CU, further studies with data on the use of over-the-counter medications and validation of our algorithms based on clinical chart reviews are needed.
The median duration of CU in the present study population was 1.6 years, which is similar to previous reports.
1920 Over a 5-year period, only 12% of CU patients stopped visiting clinics within 3 months in our study; the highest proportion of patients was treated for 12-24 months, accounting for 23% of all patients with CU. In our findings, 38.2% of CU patients had stopped visiting clinics under the diagnosis of urticaria within 1 year, whereas another 38.9% had remained in the claims database for at least 3 years. A previous retrospective study on 450 patients with CU in Thailand revealed a consistent result with the present study in that 34.5% of CU patients had symptom remission within 1 year.
13 Toubi et al.
11 reported that, in more than 70% of 139 patients with CU, urticaria lasted for more than 1 year, whereas we found that 61.9% of patients in our study were treated for CU for more than 1 year.
In regards to medication use, 27.2% of CU patients used antihistamines alone, while only 1.1% used systemic corticosteroids without antihistamines. Among antihistamine users, 69.5% took non-sedating ones, and 49.7% had prescriptions for sedating antihistamines. In a previous retrospective study of distributions of medications used for CU patients, the authors observed that 72% and 46% of patients were taking non-sedating and sedating antihistamines, respectively.
21 In contrast, 69.9% of patients received combined medicines, antihistamines, and systemic corticosteroids in the present study. A recent claims-based study in the US also revealed that the most common prescription pattern for CU population was a combination of non-sedating antihistamines with at least one course of oral corticosteroids;
9 however, this was recorded for only 31.0% of their study patients, which is almost half that noted in our study. Moreover, oral corticosteroids (70.9%) were the most common medication, comparable to the frequency of prescription non-sedating antihistamines (69.5%) in the present study, whereas 53.7% of patients in the study by Zazzali et al.
9 used oral corticosteroids. Taken together, while the patterns of prescription urticaria medication use in Korea were similar to those in US,
9 relatively more frequent use of systemic corticosteroids was observed in the present study. Notwithstanding, insurance claims do not link prescriptions with diagnoses in the HIRA database, and sometimes, oral corticosteroids can be used for treating other combined diseases.
In our study population, gastrointestinal disease was most commonly associated with CU, followed by allergic rhinitis, common cold, asthma, atopic dermatitis, and hypertension, in that order. The rank ordering of frequently combined diseases was dependent on the ages of the CU patients. The most common comorbidity among patients of ages over 5 years was gastrointestinal disease, rates of which increased with age. Interestingly, a recent meta-analysis demonstrated a significant association between
Helicobacter pylori infection and CU.
22 A higher prevalence of
H. pylori infection in Korea could plausibly explain the high frequency of gastrointestinal diseases as a comorbidity of CU in the present study.
23 However, as HIRA data are collected for the purposes of reimbursing healthcare services, the code of K29 could be added to diagnoses when prescribing H2 receptor antagonists for controlling urticarial symptoms and not for treating gastrointestinal diseases in CU patients. In contrast, common cold and allergic rhinitis were the most common comorbidities in children younger than 5 years. In agreement with our findings, allergic rhinitis and asthma were noted as the most frequent comorbidities in another claims-based study.
9 In Italy, different findings were observed for a 12-year period longitudinal database.
10 Although they enrolled patients older than 15 years, they noted a higher risk of developing CSU in patients with malignancies and anxiety, as well as in obese individuals, whereas allergy had no impact on the risk for CU.
10 Meanwhile, we investigated patients of all ages registered in the HIRA database, and a higher prevalence of CU in younger subjects was noted. For these reasons, our analyses may not have identified anxiety, diabetes, and malignancies, which are more prevalent in older populations, as common comorbidities among CU patients in the present study.
There were some limitations to the use of HIRA data in this study, even though the database provides a wealth of information on demographics and treatment patterns of CU in Korea. Since no specific disease code for CU is available and since both over-the-counter drugs and herbal medicines were not registered in the present study, a confirmatory medical record analysis of CU patients is needed to obtain accurate estimates of the prevalence and disease burden of CU in Korea. In addition, a possible discordance between drug claims and active urticaria symptoms might distort real medication patterns of CU in the HIRA database.
In conclusion, we have outlined the epidemiology of CU in Korea using a nationwide database. The prevalence of CU in this study was similar to that in the literature for other countries. However, we were able to shed light on more frequent use of systemic corticosteroids, a relatively shorter duration of prescription antihistamines, and a higher frequency of gastrointestinal comorbidity, compared with other countries. Thus, to support physicians in the management of urticaria, development of appropriate treatment guidelines may be needed.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download