Abstract
Purpose
To characterize differences in upper and lower eyelid positions among different Korean age groups.
Methods
Digital photographs of 380 patients were retrospectively selected. Patients who had no known eyelid disorders or previous surgeries that could affect eyelid position were included. The marginal reflex distance 1 (MRD1) and marginal reflex distance 2 (MRD2) were measured from photographs using Image J software. Patients were divided into four groups for analysis: a child group, 0–20 years of age; a young adult group, 20–40 years of age; a middle age group, 40–60 years of age; and an elderly group, ≥60 years of age.
Results
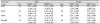
Total of 380 eyes from 380 patients were included. Mean age was 38.90 ± 22.79 years, and 200 (52.6%) were male. Mean MRD1s (mm) in each age group were: 0–20 years (n = 92), 2.94 ± 0.95; 20–40 years (n = 102), 3.23 ± 0.92; 40–60 years (n = 94), 3.33 ± 1.09; and ≥ 60 (n = 92), 2.42 ± 1.03. Mean MRD2s (mm) in each age group were: 0–20 years (n = 92), 5.37 ± 0.68; 20–40 years (n = 102), 5.66 ± 0.58; 40–60 years (n = 94), 5.29 ± 0.80; and ≥ 60 years (n = 92), 4.45 ± 0.86. The mean MRD1 was longest in the middle age group, and shortest in the elderly group. The mean MRD2 was longest in the young adult group, and shortest in the elderly group. The mean MRD1 (mm) was 2.90 ± 1.07 in males and 3.09 ± 1.03 in females. The mean MRD2 (mm) was 5.44 ± 0.68 in males and 4.95 ± 0.96 in females, and there was a statistically significant difference in the MRD2 between the two sexes (p = 0.077, p=0.000, respectively).
Conclusions
Significant decreases were observed in the MRD1 and MRD2 with Koreans aged ≥ 60 years. Notably, the decrease in MRD2 in females was more significant than in males. This could be important reference values for successful eyelid surgery, especially in elderly patients. The amount of surgical correction during upper lid surgery should be determined according to the MRD1, in order to prevent overcorrection.
Figures and Tables
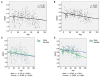 | Figure 1Correlation of marginal reflex distance 1 (MRD1) and MRD2 according to age and sex. (A) MRD1 and age. (B) MRD2 and age. (C) MRD1 and age in each sex group. (D) MRD2 and age in each sex group. *Simple linear regression test. |
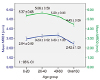 | Figure 2The mean marginal reflex distance 1 (MRD1) was longest in the middle age group, and shortest in the elderly group. The mean MRD2 was longest in the young adult group, and shortest in the elderly group. CI = confidence interval. |
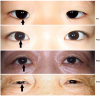 | Figure 3Examples of eyelid presentation of each age group. Arrows point decrease of marginal reflex distance 2 (MRD2) in females, according to age. There is significantly upward shift of the lower eyelids and decreased MRD2 in old age (> 60), a phenomenon called “reverse ptosis”. F= female. |
 | Figure 4A case of blepharoplasty in an elderly women. (A) 75-year old female patient with involutional ptosis in both upper eyelid and reverse ptosis in both lower eyelid. (B) Intra-operative photograph of the same patient. Surgical correction of upper eyelid involutional ptosis was done. The amount of surgical correction during upper lid surgery should be determined according to marginal reflex distance 1 (MRD1) (mm), not according to palpebral fissure height, in order to prevent overcorrection and postoperative complications such as lagophthalmos. (C) Postoperative 3 months. Lower eyelid is still positioned superior to the inferior limbus, a phenomenon frequently called ‘reverse ptosis’. However, upper eyelid involutional ptosis is successfully corrected without overcorrection. |
References
1. Baek SM, Kim SS, Tokunaga S, Bindiger A. Oriental blepharoplasty: single-stitch, nonincision technique. Plast Reconstr Surg. 1989; 83:236–242.
2. Noh SH, Choi O. The palpebral fissure of the Korean youth. J Korean Ophthalmol Soc. 1981; 22:491–498.
3. Park JS, Ham KS, Cho YJ. An anthropometric study on the young Korean faces related to their facial expression. J Korean Soc Plast Reconstr Surg. 1989; 16:920–925.
4. van den Bosch WA, Leenders I, Mulder P. Topographic anatomy of the eyelids, and the effects of sex and age. Br J Ophthalmol. 1999; 83:347–352.

5. Seo HR, Ahn HB. Morphological changes of the eyelid according to age. J Korean Ophthalmol Soc. 2009; 50:1461–1467.

6. Moon CS, Moon SH, Jang JW. Topographic anatomic difference of the eyelid according to age in Korean. J Korean Ophthalmol Soc. 2003; 44:1865–1871.
7. Nishimoto H, Takahashi Y, Kakizaki H. Relationship of horizontal lower eyelid laxity, involutional entropion occurrence, and age of Asian patients. Ophthalmic Plast Reconstr Surg. 2013; 29:492–496.

8. Bartley GB, Frueh BR, Holds JB, et al. Lower Eyelid Reverse Ptosis Repair. Ophthalmic Plast Reconstr Surg. 2002; 18:79–83.

9. Park DM, Song JW, Han KH, Kang JS. Anthropometry of normal Korean eyelids. J Korean Soc Plast Reconstr Surg. 1990; 17:822.
10. Ezure T, Yagi E, Kunizawa N, et al. Comparison of sagging at the cheek and lower eyelid between male and female faces. Skin Res Technol. 2011; 17:510–515.

11. Segal KL, Patel P, Levine B, et al. The effect of transconjunctival blepharoplasty on margin reflex distance 2. Aesthetic Plast Surg. 2015; 40:13–18.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download